Abstract
Background: The use of neuromodulation in the treatment of psychiatric conditions is controversial despite its lengthy history. This particularly applies to the use of invasive neuromodulation, such as deep brain stimulation (DBS), to treat substance use disorder (SUD) due to the considerable risks of the procedures. However, given the advances in DBS research and the shortcomings of current treatment modalities for addiction, off-label use and clinical trials are being implemented for the management of treatment-refractory patients.
Methods: Here we conduct an ethical and legal analysis of DBS for SUD, referencing the four foundational principles of medical ethics and key legal concepts.
Results: There are major concerns related to the capacity of a SUD patient to provide informed consent, as well as the risks and benefits of DBS compared to traditional treatment methods. In addition to ethical concerns, we explore potential legal issues that may arise from DBS in the treatment of addiction. These include the potential mandate of these procedures in the context of the criminalization of substance use, and the issue of familial consent in the decision-making process. Given the paucity of relevant clinical guidelines or legal cases, general medico-legal principles serve as the reference in making decisions about the responsible use of DBS as a treatment for addiction.
Conclusions: Given the rapidly increasing evidence for DBS as a treatment for SUD, it is an urgent imperative to consider the relevant key ethical and legal issues. Incorporating IDEAL (Idea, Development, Exploration, Assessment, Long-term follow-up) framework into future research in DBS is recommended to evaluate patient safety and ethical perspectives. With the broad criminalization of SUD across the globe, legal coercion of DBS is not impossible, especially if proven to be effective to treat SUD. It is advised for stakeholders to urgently consider incorporating DBS-related drug policies so that the potential benefits of DBS within the rights of people with SUD are not hindered by the lack of clinical guidance and legislations.
Introduction
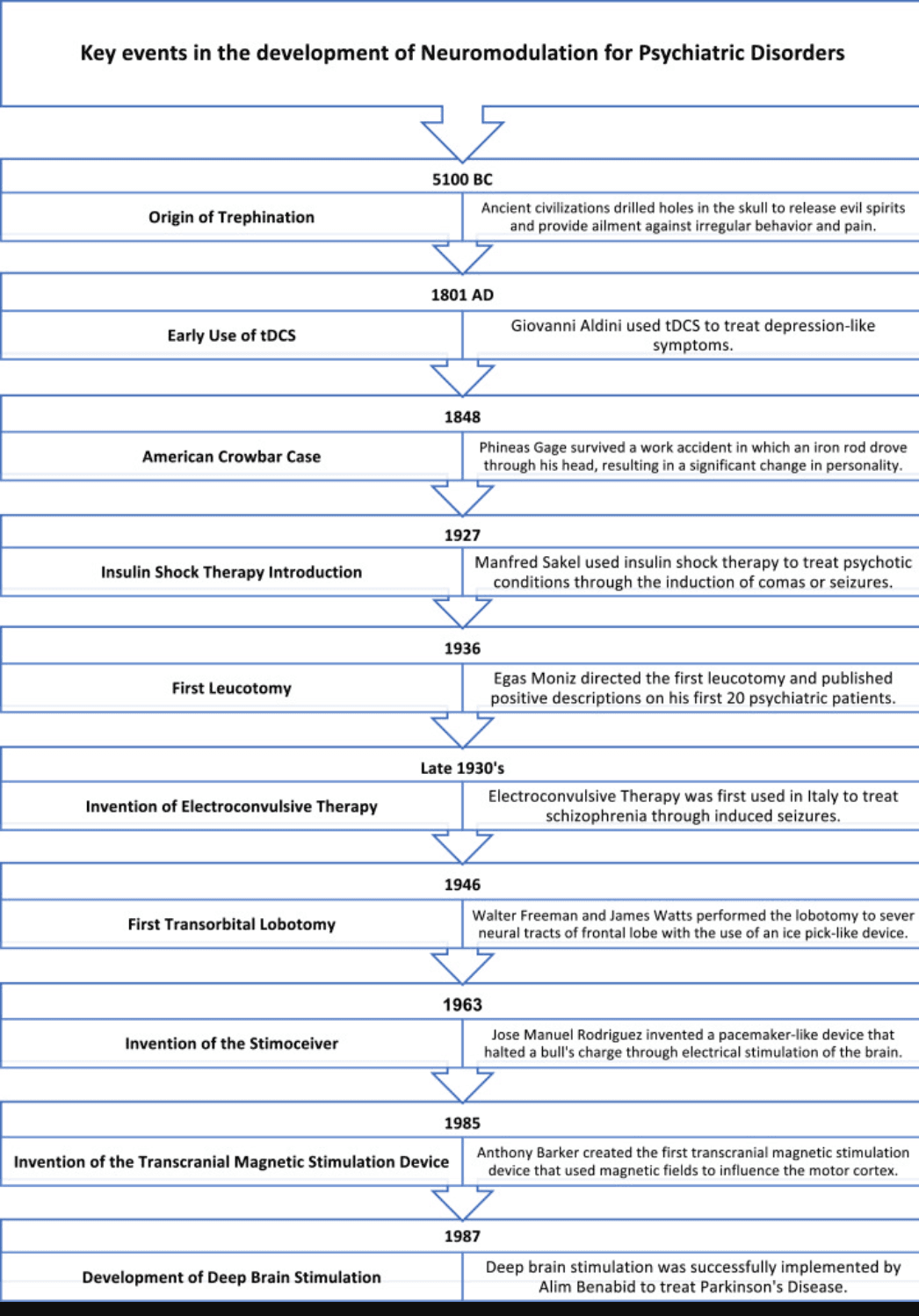
Modern psychosurgery began in the 1940s through the introduction of lobotomies, but the use of neurosurgery in treating psychiatric disorders dates to prehistoric times. From 5100 BC, our ancestors believed that drilling trephine holes in the skull would release evil spirits and provide ailment against irregular behavior and pain (Fig. 1) (Faria, 2013b). Following the surge of phrenological studies regarding phrenology throughout the 19th century, the hallmark “American Crowbar Case” further defended the physiology of personality and behavior, i.e., personality is not a spiritual concept but rather brain-based. Phineas Gage, an American construction worker, suffered a work injury in which an iron rod was driven through his skull, resulting in a complete transformation of personality (Gallea, 2017). As the interest in brain localization grew, associated neurosurgical techniques were developed. The leucotomy, and associated lobotomy, gained prevalence through the 1930s and 1940s, promising success and short operation time. Unfortunately, despite its popularity, the procedure often led to severe side effects, such as personality changes and the inability to function independently. While the prevalence of lobotomy decreased in the ensuing years, studies surrounding brain localization continued to flourish. As the understanding of localization of function grew, another psychosurgery treatment emerged: electrical stimulation of the brain (ESB). The ESB concept was popularized by Jose Delgado through the stimoceiver: a pacemaker-like device that utilized ESB to influence emotions and behavior, famously halting a bull's charge by the click of a button (Faria, 2013a). Although his work was subject to criticism due to concerns of extremism, Delgado is widely considered a significant figure in the history of neuromodulation.
Fig. 1. Summary of the key events that shaped the history of neuromodulation in psychiatric disorders.
The achievements of these scientists and physicians have paved the path for the use of neurostimulatory devices for psychiatric disorders. There has been great recent progress in neuromodulation techniques in treating mental illnesses, such as depression (Crowell et al., 2019; Yuen, Rusheen, et al., 2021) and obsessive-compulsive disorder (OCD) (Hamani, et al., 2014). Although these results are promising, its application to substance use disorder (SUD) remains a highly controversial gray area. SUD, or drug addiction, is defined as the recurrent use of a substance despite harmful consequences including a loss in social function and substance use control (SAMHSA, 2020b). In many countries, SUD remains stigmatized or even criminalized, which raises the question of whether the condition should be considered a medical disease or learned behavior. In 1987, the American Medical Association officially declared addiction to be a disease, although certain members of the medical community still hold negative biases against SUD patients (Bettinardi-Angres & Angres, 2010).
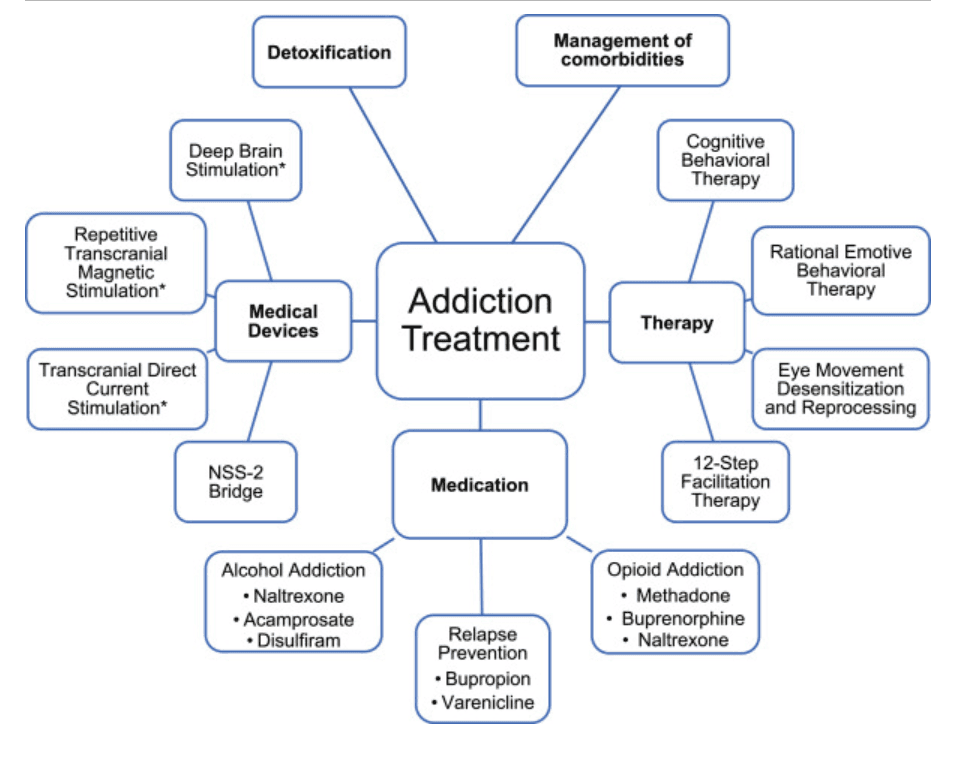
Current treatments for SUD involve detoxification, behavioral therapy, motivational interviewing, peer support, medication, and medical devices (Fig. 2) (National Institutes on Drug Abuse (US), 2020). Though each of these methods has displayed some efficacy in the treatment of addiction, a large unmet need remains. For example, the majority of patients who fail to receive further care relapse within a year (McCance-Katz, 2020). In 2019, 40.3 million people in the US alone had a substance use disorder (SAMHSA, 2020a). Among those who have been treated for alcohol and other substance dependence, 40-60% relapsed to active substance use within one year post discharge of treatment (McLellan, Lewis, O'Brien, & Kleber, 2000). Similarly, another large observational study showed that at the five-year follow-up a further substantive proportion returned to drug use (Hubbard, Craddock, & Anderson, 2003), indicating a strong need for alternative treatment options (McLellan, et al., 2000). Due to the deficiencies of current addiction treatment methods, there is a growing interest in neuromodulation in treating addiction.
Fig. 2. Main treatment options that addiction patients are recommended depending on the source of their addiction. * Denotes non-FDA approved treatment methods.
The use of neuromodulation as treatment for addiction began in the 1960s through lesional procedures including cingulotomy and hypothalamotomy. However, these procedures had both limited efficacy and unacceptably high risks (Wang, Moosa, Dallapiazza, Elias, & Lynch, 2018). With improving understanding of addiction circuit, such as from observations where brain lesions in specific area led to improvement in some patients’ addiction-associated behaviors (Joutsa, et al., 2022; Tranel, McNutt, & Bechara, 2012), three more promising treatment modalities emerge: transcranial direct current stimulation (tDCS), repetitive transcranial magnetic stimulation (rTMS) and deep brain stimulation (DBS). Both tDCS and rTMS are considered “non-invasive”. They use strong electrical currents and magnetic fields respectively to modulate neural activities. Studies have demonstrated these can lead to statistically significant reductions compared to baseline in craving for substances, e.g., for cocaine, nicotine, marijuana, alcohol, and heroin (Fregni, et al., 2008; Makani, Pradhan, Shah, & Parikh, 2017; Spagnolo & Goldman, 2017). The effectiveness varies according to the substance and parameters used. For example, rTMS appeared to be effective in two-thirds of patients who suffer from nicotine, alcohol, and cocaine dependence but 100% effective in those with cannabis dependence (Makani, et al., 2017). While positive results have been reported, there have been several cases in which the interventions have not yielded statistically significant benefits but has side-effects such as scalp discomfort and sleep disturbances (da Silva, et al., 2013; Del Felice, et al., 2016; Hoppner, Broese, Wendler, Berger, & Thome, 2011; Spagnolo & Goldman, 2017; Xu, Fregni, Brody, & Rahman, 2013). Given the small number of studies currently available, more published data is needed to ascertain the effectiveness and safety profile of tDCS and rTMS in this context.
How does deep brain stimulation work?
DBS, which involves permanent implantation of electrodes into specific deep neural structures, is a well-established treatment for movement disorders such as Parkinson's disease (Benabid, 2003; Lee, Lozano, Dallapiazza, & Lozano, 2019). By targeting specific parts of dysfunctional neural circuits, neurological symptoms are ameliorated. The exact mechanism of action is currently unknown, and it may differ depending on the DBS target and stimulation parameters. Nevertheless, the following theories have been proposed as its potential mechanism for a range of disorders: 1) direct inhibition of neural activity, 2) direct excitation of neural activity, 3) information interruption, and 4) synaptic filtering (see (Lee, et al., 2019) for a detailed review). In preclinical studies of drug use, there is strong evidence of local inhibition of baseline and drug-related neural activity where DBS is targeted (Baunez, Dias, Cador, & Amalric, 2005; Lozano, et al., 2019; Rouaud, et al., 2010). Such inhibition may be driven by the inhibitory neurotransmitter gamma-aminobutryic acid (Wilden, et al., 2014), and/or involves quenching of glutamatergic/dopaminergic excitation via metabotropic receptor signaling (Creed, Pascoli, & Luscher, 2015; Levy, et al., 2007; Niu, et al., 2020). In contrast, some preclinical studies showed that DBS may lead to an increase in dopamine and reduce use by replacing the dopamine surge associated with the addictive substance (Hadar, et al., 2016). While this is a plausible explanation since addictive substances are known to induce strong dopaminergic response (Grace, 2000; Yuen, Goyal, et al., 2021), evidence for dopamine replacement mechanism for DBS to treat SUD is yet scarce. DBS in SUD likely operates in a much more complicated manner as preclinical studies showed other neurotransmitters such as serotonin and glutamate also play important role (Yuen, Goyal, et al., 2022; Yuen, Kouzani, et al., 2022).
Potential advantages of deep brain stimulation
DBS has the potential to reduce harm and relapse in multiple types of addiction (e.g., alcohol, cocaine, heroin) (Yuen, Kouzani, et al., 2022). In addition, it reduces the need for patients to pay frequent visits to specialist addiction centers to refill their prescription of controlled substances used in conventional maintenance, which can lead to heavy time costs and social stigma, ultimately leading to treatment non-compliance and discontinuation. DBS also saves the healthcare organizations resources in distributing drugs such as methadone and buprenorphine. This can cost $6000 per year per patient, which is even more than how much it would cost to treat a diabetes or chronic kidney disease patient (National Institute on Drug Abuse, 2021).
Compared to tDCS and rTMS, DBS offers more focused stimulation to the neural structures that are implicated in addiction-related behaviors, which are often deep in the brain. These areas may not be reachable by tDCS or rTMS. In addition, DBS can simultaneously alleviate psychiatric comorbidities such as depression, which is not uncommon in SUD (Drobisz & Damborska, 2019; National Institutes on Drug Abuse 2020). Furthermore, with recent technological advances, it is now possible for physicians to hold virtual consultation with DBS patients and program their device remotely (Abbott, 2021). This helps to mitigate the necessity of repeated appointments at a specialized tertiary center, which are often required for tDCS and rTMS treatments.
Although there are few published case reports of treating addiction with DBS, the results are encouraging (Ali, et al., 2016). DBS may have effects on decision-making and hedonic drive, causing patients with addiction to abstain from alcohol and heroin use (Spagnolo & Goldman, 2017). A recent review in 2022 summarized the pre-clinical and clinical studies concerning DBS as a treatment technique for SUD (Yuen, Kouzani, et al., 2022). It concluded that DBS, specifically of the nucleus accumbens (NAc) and prefrontal cortex, has encouraging indications as a treatment option. Clinicaltrials.gov currently lists 16 ongoing trials involving DBS for addiction (U.S. National Library of Medicine, 2021), demonstrating the ongoing interest in the area. Therefore, given scientific evidence is accumulating towards clinical recommendation for the routine use of DBS in refractory SUD, it is mandatory for policy makers to seriously consider at present the ethical and legal implications of DBS in drug policies to ensure clinical guidance and legislation do not lag behind the benefits that the technology can offer.
Potential risks
However, the risks from DBS should not be understated. They include brain hemorrhage (<2% of patients), and more commonly, wound infection and stimulation-caused side effects (up to 9% of cases) (Spagnolo & Goldman, 2017). For these reasons, DBS is currently only considered as a last resort in patients who are refractory to standard treatments for SUD. However, there are no standard definitions of “treatment-resistance” or “treatment-refractory”, and a pragmatic definition of “repeated failure in orthodox treatment” has been offered to describe refractory addiction (Soyka & Mutschler, 2016). This is particularly complex in SUD because patients can, and commonly do, for example, fail a trial of rehabilitation only for the same treatment to succeed on another attempt. Resistance may also be driven by factors outside of addiction itself, such as socioeconomic deprivation or comorbidity of severe personality disorder or other psychiatric disorders. In addition, what counts as “repeated failure” does depend on the patient, clinician, and local resources. Considering all these factors, the decisions to offer patients DBS treatment for addiction are not straightforward, with multiple ethical and medicolegal pitfalls, which we will explore here.
Ethical dilemmas
Four foundational principles
Medical ethics is built upon four traditional principles that provide a reliable framework for examining moral challenges that arise in the practice of medicine. These four widely taught principles are autonomy, beneficence, non-maleficence, and justice (Beauchamp & Childress, 2019). It should be noted that while our analysis here focuses predominantly on the use of DBS, an invasive surgical treatment, some of the issues raised here can also be generalized to other experimental pharmacotherapies or non-standard behavioral interventions.
Autonomy
The first principle, the respect for patient autonomy, ensures that individuals have agency in their own decisions and actions. However, it is crucial that these choices are being made by those who have the mental capacity to make such decisions and they should have the right to refuse treatment regardless of social, financial, and cognitive situation (Carter & Hall, 2008). The threshold for this capacity is governed by the patient's ability to understand, apply, and utilize the information that is present regarding their case (Gillon, 1994). Carter and Hall suggested there are four key requirements for informed consent in drug addiction treatments. In addition to the three conventional criteria: 1) possession of mental capacity, 2) freedom to make decisions, and 3) adequate information, a fourth criteria is necessary, which is equal access to all effective treatment modalities (Carter & Hall, 2008). The authors believe the latter is particularly relevant (and difficult to implement) in the context of SUD because of the interacting health care resourcing, political and social factors that may limit the accessibility of all treatment options. To overcome this, both physicians and patients must first be educated on the effectiveness, risks, and availability of the treatment. To take OCD as an example, despite the proven effectiveness of DBS by a good number of studies, its access continues to be limited due to lack of education of health care providers (Visser-Vandewalle, et al., 2022).
Since SUD is known to induce changes in the ability to prioritize, tendencies to engage in risky behavior, and paranoia, assessing capacity is challenging (Bettinardi-Angres & Angres, 2010). Changes in personality, behavior, and cognition, often compounded by associated socio-economic issues, may lead to undue pressure on patients to consent to invasive treatments that they may not normally agree to. A similar framework to the patient selection recommendations for DBS in Tourette's patients can be used as a guideline for individuals with addiction. Here, the surgical candidates must (1) be informed of the risks, benefits, and alternative therapies, (2) undergo an evaluation confirming that DBS is the suitable treatment plan, and (3) require the public documentation of early clinical studies (Mink, et al., 2006). Another potential solution to the question of autonomous capacity is the use of a standard fitness assessment (Grisso & Appelbaum, 1998). One example is the MacArthur Competence Assessment Tool for Clinical Research, where Appelbaum et. al. reported good performance in assessing depressed patients’ capacities to consent to research in the outpatient setting (Appelbaum, Grisso, Frank, O'Donnell, & Kupfer, 1999). Also, fitness assessments are commonly used in the legal settings where an accused person may be deemed “unfit to stand trial” if the judge has reasonable grounds in doing so. Likewise, if there are reasons to believe the patient does not have the mental capacity to make a reasonable decision, there may be a higher emphasis on family regard or the insight of a physician or courts, with the patient's best interest in mind.
In addition, patients who have reduced levels of consciousness following brain injury have used surrogate decision-makers to make judgments that appeal to what the patient would have chosen and what is in the patient's best medical interests (Graham, 2020). A similar concept may be applied to SUD patients whose capacity is unlikely to recover in the short-term. Some also go further and argue that, by definition, those who truly suffer from SUD does not possess the freedom to make decisions (key criteria for informed consent), and therefore does not have capacity (Caplan, 2008). Hence they could be subjected to mandatory treatment (Caplan, 2008). However, this should be assessed on an individual basis by a multidisciplinary team, considering a range of patient factors and clinical evidence such as the substance(s) used, drug tolerance, length of time used, treatment history especially treatment resistance, and available social supports.
Beneficence
The principle of beneficence describes a medical care provider's moral duty to do good unto others and center the welfare of others as their end goal (Kinsinger, 2009). This principle emphasizes the intention and mentality that is expected of medical care providers. Applying to neuromodulation to treat addiction, it requires providers to carefully consider the benefits the treatment will potentially offer to individual patients. Beneficence relates directly to the provider's goal to improve the patient's quality of life through treatment, guided by the latest evidence and experts’ recommendations. This may be achieved through mandating a multidisciplinary panel to provide their opinion on the necessity of neuromodulation, prior to treatment (Ford & Kubu, 2006). Such panel may consist of addiction counselors, addiction psychiatrists, neurosurgeons, social workers, patients’ next-of-kin, and the patients themselves to curate objective considerations for their wellbeing. DBS should be considered for neuropsychiatric diseases only when other evidence-based treatments such as pharmacological therapies and psychotherapy do not elicit an adequate response, fail to sustain a response, or the patient experiences unacceptable adverse effects (Nuttin, et al., 2014), which likely include consequences that are permanent and unacceptable to the individual patients, resulting in lifestyle changes.
Currently, patients with SUD face immense pressure (subtly and overtly) from the judicial and social systems to receive treatment. This can lead to a slippery slope situation where a precedent is established for coerced psychosurgery. Therefore, the necessary resources that safeguard patients’ informed consent in entering treatment should be demonstrated before any healthcare system is allowed to provides psychosurgery services such as DBS.
Non-maleficence
The third principle, non-maleficence, obligates that the medical provider must not inflict harm. This elicits the conversation on whether DBS may pose too much potential harm for those suffering from SUD, considering there are alternative options (Ford & Deshpande, 2013). With DBS, not only is there the risk of complications during surgery, but there are also potential post-operative complications. For example, the classic Olds and Milner rat experiments demonstrated that self-administration of electrical stimulation into certain parts of the brain may lead to repeated pressing of the triggering lever (analogous to human compulsive behavior) (Olds & Milner, 1954). Furthermore, there is a case report of a single patient with Parkinson's disease that DBS can induce radical personality changes such as mania and hypersexuality and at times, patients may refuse to stop electrical stimulation and revert to their, often more subdued, pre-treatment personality, despite the insistence of their family to terminate treatment (Kim, et al., 2012). These mood changes are directly correlated to an individual's quality of life, may generate substantial risks to the person and are a significant concern of neuromodulation. Furthermore, there are associated psychosocial complications for the patient and family. There are risks for adjustment difficulties and emerging conflicts with personal relationships, specifically with their spouse, due to the patient's abrupt change in independence following DBS (Bell, Maxwell, McAndrews, Sadikot, & Racine, 2011). It is thus necessary to define the threshold of addiction severity and treatment resistance in which neuromodulation would be recommended using the best medical evidence available. Despite rapid scientific advances in the applying DBS in treatment-refractory SUD, the difficulty lies is the current lack of high-quality evidence in the field regarding the risks and benefits of the treatment (Spagnolo & Goldman, 2017). One more recent study of 8 patients with heroin SUD showed side-effects such as fever, headache, insomnia, and subjective slight memory decline were all transient. One patient also had a small intracranial hemorrhage with no neurological sequalae (Chen, et al., 2019).
Furthermore, while those with a history of near-lethal overdosing, treatment resistance and high-risk psychiatric comorbidities may benefit most from more radical treatments, there is not enough evidence to identify which patient group would benefit the most from DBS and which group would most likely be affected by potential adverse effects. In addition, social context and behavioral component may help to predict who would show the best response from DBS treatment because they bear critical importance in SUD development (Leshner, 1997; Guerin & Kim, 2021). For example, intravenous users are shown to experience more drug-cue induced craving (Guerin, et al., 2021), which DBS has been shown alleviate. Extrapolating from studies focusing on pharmacological intervention/s, certain predictors such as employment status (being employed is correlated with positive treatment response) may help to target treatment-refractory SUD and be useful for patient selection for DBS (Brewer, Catalano, Haggerty, Gainey, & Fleming, 1998).
When appraising neuromodulation, one must also consider ablative procedures where a permanent lesion is induced. The benefit of DBS over such procedure is the reversible nature of the treatment, where the energy delivered can be varied. Compared to other options such as the MRI-guided focused ultrasound and radiofrequency ablation, DBS can be switched off if the procedure negatively impacted the patient (Yuen, Kouzani, et al., 2022). This favors its use over other ablative techniques as the potential harm caused is likely to be less. This is particularly important here as the long-term outcome of SUD patients with neuromodulation is yet to be fully determined.
Justice
The final principle is that of justice, where the “idea that the burdens and benefits of new or experimental treatments must be distributed equally among all groups in society” (Johnson, 2000). Following the logic, the treatment must be justified by the benefit it will bring to the society. The cost of the DBS procedure ranges from $35,000 to $45,000 (Jacob, Geddes, McCartney, & Burchiel, 2016). This estimate may be higher considering the required pre- and post-operative care and need for ongoing monitoring. In contrast, on an individual level, a person with heroin use disorder will spend between $24,000 and $93,805 annually on maintaining their addiction (Aspenridge Recovery, 2020). Similarly, maintaining a serious methamphetamine addiction can cost over $40,000 annually (Aspenridge Recovery, 2020). The cost will be even higher to the society if one considers those with SUD may have increased risk of being involved in crimes and receive prison sentences. With DBS treatment, the cost of device installation constitutes most of the costs, with comparatively small amounts of resources required for reprogramming over time. Therefore, large amount of annual savings could potentially be made when considering the treatment of patients with refractory SUD.
To more formally quantify the value of health outcomes, one may consider a cost-utility analysis using measures such as the quality-adjusted life years (QALY) (Prieto & Sacristán, 2003). A theoretical calculation using QALY showed that DBS only needs to be 49% effective (abstinence 6 months after treatment) to be as cost-effective as methadone in treating opiate addiction (Stephen, et al., 2012). Therefore, comparing the cost of treatment to the cost of addiction for the patient and for society, DBS treatment seems to uphold the prima facie of justice, assuming further research confirms its effectiveness.
Another consideration regarding the cost of the procedure is accessibility. People with a stable income are, for example, less likely to have an addiction compared to people with socioeconomic disadvantage (Nagel & Correa, 2022). The stress of unemployment can lead to or aggravate substance misuse, thus creating a vicious cycle in those who suffer from addiction without having access to resources and treatment. In accordance with the biopsychosocial model of psychiatric diseases, stressors, risks in people's biology or social life can impact their psychological health. The criminalization of substance use adds more barriers to the road to recovery by reinforcing the false narrative that addiction is not a medical disorder. With emerging evidence demonstrating DBS as a promising treatment, it is necessary to define the population that are likely to benefit from and uphold the principle of justice by offering treatment to those in need.
Ethics in the research setting
Clinical trials are key advancing our understanding of the efficacy, safety, and risks of these novel treatments. The majority of published studies have been single case studies or localized on one part of the circuitry involved in addiction (Yuen, Kouzani, et al., 2022). While current research models have provided valuable insights, the focus on animal subjects can have limitations in replicating human conditions (Wang, et al., 2018). Also sample size is limited due to the scarce resources and the various ethical considerations in the process of conducting neuromodulation research in this domain, given the vulnerability of the patients. For example, the inclusion of monetary benefits for the study participation might hinder the individual's ability to give unbiased consent. Nonetheless, through careful consideration in the recruitment process by an ethics committee, these issues can be mitigated. Incorporation of the ideas of existing research framework, such as the IDEAL (Idea, Development, Exploration, Assessment, Long-term follow-up) framework (Sedrakyan, et al., 2016), may also promote continuous evaluation of the research process and patient safety, yet with earlier access to those in need. The framework helps to evaluate different stages of surgical innovation, and allows a more unified, logical manner in the development and evaluation of the technique, balancing innovation and safety (Marcus, et al., 2022). One example is the use of a novel low-cost minimally invasive spinal surgical technique, which has been through the innovation and development stages and is now advancing towards the larger scale randomized controlled trial stage (Flores, Beltran, & Ogando-Rivas, 2019). This is an example where a well-recognized, standardized research framework can be applied to an innovative idea.
Due to the hazardous nature of neuromodulation for psychiatric disorders, there must be significant evidence prior to the designation of “approved therapy”. According to an expert consensus on stereotactic neurosurgery for psychiatric illnesses, to qualify, at least two groups of researchers must publish good quality randomized controlled clinical studies with similar risk-benefit ratios as current approved therapies (Nuttin, et al., 2014).
Local resources, legislation and investigators’ experience currently dictate the inclusion and exclusion criteria of individual clinical trials. Strict protocols are developed by a multidisciplinary panel. In general, current trials only include adult patients who have the capacity to consent and have failed conventional treatment. Those with other significant psychiatric disorders, those who are pregnant, and those who possess contraindication for DBS surgery are generally excluded (U.S. National Library of Medicine, 2014, U.S. National Library of Medicine, 2016a, U.S. National Library of Medicine, 2016b). These are consistent with the four principles we outlined above and aim to safeguard the most vulnerable. To maximize the potential benefits offered by DBS, those who are at highest risk of suffering from a lethal overdose given the clinical history and social context would likely be acceptable candidates given the risks of significant morbidity and mortality if left without treatment. This is provided that they have no other contraindications to be included in the study (such as unacceptable surgical risks).
Legal considerations
Upon cogitating on the ethical dilemmas that arise in treating addiction with neuromodulation, it is imperative to consider the medicolegal aspects. By doing so, one can ensure patients’ legal rights are respected, and medical practitioners are protected from lawsuits. As studies of neuromodulation's effect on SUD are still preliminary, there are few precedent legal cases and real-life applications that can be discussed. This can be done through the analysis of past legal rulings of medical practice and applying these precedents to neuromodulation in addiction.
Though there are few laws in place regarding the practice of DBS specifically, we can follow the legal precedent set by electroconvulsive therapy (ECT) regulations. ECT has a negative image in society because of its unethical usage in the past, and its portrayal in popular media. Because of this, ECT is a highly regulated procedure with many state laws and organizational standards. Informed consent is an important aspect of these statutes and standards. The American Psychiatric Association's (APA) Task Force Report on ECT states that the psychiatrist should provide a thorough explanation of the following areas to each prospective ECT patient: (1) indication and rationale of using ECT, including the available and reasonable alternatives and their attendant risks and benefits; (2) the likelihood and severity of relevant risks; (3) the possibility of the need to perform emergency medical intervention in the event of complications; (4) assurance that the consent is voluntary and can be revoked at any time without penalty; (5) encouragement to ask questions at any time about ECT; and (6) restrictions on patient behavior that are likely to be necessary prior to, during, and following ECT (Leong & Eth, 1991). We can use these guidelines for ECT as a framework for guidelines for DBS. In application to DBS to treat addiction, it is of the utmost importance that patients understand the risks and benefits of this procedure. Should the patients decide to undergo DBS to treat their addiction, their autonomy should be safeguarded by equipping them with the full knowledge of the risks, benefits, and alternatives to DBS treatment.
Medico-legal frameworks vary widely across the globe, partly due to the local history and culture. Some examples of the differences between the East and West are illustrated in Table 1. In the United States, it is legal to allow families and medical practitioners to petition to have a person with a mental illness undergo court-mandated treatment in 37 out of 50 states, and the District of Columbia (Treatment Advocacy Center, 2021). These laws vary state by state, but the main premise and most used standard behind these mandates is whether the person poses a real and present threat of danger to themself or others. However, in most instances, the treatments are psychosocial in nature with or without pharmacological adjunctive therapy and this poses very different risk benefit ratios to DBS. SUD is a mental disorder, but substance misuse is often criminalized. Those who suffer from SUD face legal repercussions such as jail time, heavy fines, community service, and probation. The legal repercussions also create very important considerations for ethical approval of invasive therapies. The criminalization is also followed by societal stigmas which affects job and financial security, leading many people to view SUD patients as societal deviants (Patterson, 2021). It is important to note that although these laws exist, very few states make use of it. The stance this statute takes on autonomy and beneficence is selective in its use. The law favors the collective over the individual by legally infringing on a patient's autonomy in pursuit of beneficence by medical practitioners and family members. However, the courts can only order inpatient or outpatient treatments that are non-invasive. A consensus view on treatment under coercion was reached by the World Health Organization in 1986 (Porter, 1986). This group suggested that compulsory treatment was legally and ethically justified only if the rights of the individuals were protected by “due process”, and if effective and humane treatment was provided. In the absence of due process, the way was left open for de facto imprisonment to occur without judicial oversight (Hall, 1997).Table 1. Comparison of medicolegal cases and codes of ethics between examples of western and eastern countries. The cases and codes in each row address a similar issue, and the verdicts determine how the cases were settled based on medico-ethical norms. Further examples of legislations in other countries are illustrated in a review article by Chandler, et al. (2020).
Area of Ethics | Western Medicolegal Cases | Eastern Medicolegal Cases |
Informed consent | Montgomery Case (UK) “The law on consent has progressed from doctor-focused to patient-focused. The practice of medicine has moved significantly away from the idea of the paternalistic doctor who tells their patient what to do, even if this was thought to be in the patient's best interests. A patient is autonomous and should be supported to make decisions about their own health and to take ownership of the fact that sometimes success is uncertain and complications can occur despite the best treatment.” (Royal College of Physicians and Surgeons of Glasgow, 2021; 2015) | China's Tort Liability Law “Article 57 Where any medical staff member fails to fulfill the obligations of diagnosis and treatment up to the standard at the time of the diagnosis and treatment and causes any harm to a patient, the medical institution shall assume the compensatory liability.” Article 58 Under any of the following circumstances, a medical institution shall be at fault constructively for any harm caused to a patient…2. concealing or refusing to provide the medical history data related to a dispute” (2012) |
Biomedical research involving humans | Belmont Report (USA) This document outlines the biomedical and behavioral ethics in research involving human subjects through consideration of “ (i)
the boundaries between biomedical and behavioral research and the accepted and routine practice of medicine,
(ii)
the role of assessment of risk-benefit criteria in the determination of the appropriateness of research involving human subjects,
(iii)
appropriate guidelines for the selection of human subjects for participation in such research and
(iv)
the nature and definition of informed consent in various research settings.” (Office for Human Research Protections, 2021) | Measures for the Ethical Review of Biomedical Research Involving Humans (For Trial Implementation) The Chinese Ministry of Health released this document in 2007 to promote the institutionalization and development of medical ethics committees on various levels across China in research settings. These ethical codes are based on the principles of autonomy, beneficence, and justice (Wang & Henderson, 2008) |
Psychosurgery Precedents | Aden v. Younger “If a patient wants psychosurgery, then the conditions for performing such surgery include:(a) The patient must give written informed consent, dated, witnessed and entered in his record. The consent may be withdrawn at any time. An oral explanation by the doctor is necessary. (b) The patient must have capacity to consent. (c) An oral explanation must be given to a responsible relative, guardian, or conservator. (d) The reasons for surgery must be in the patient's treatment record, other treatments must be exhausted and surgery must be critically needed. (e) Three appointed physicians (two board-certified psychiatrists or neurosurgeons), must examine the patient and unanimously agree with the treating physician's determinations and that the patient has capacity to consent. There must be a 72-hour wait after the patient's written consent before surgery.” (Brown, 2021; California. Court of Appeal, 1976) | Notification Regarding Improvement of Management and Related Issues in Neurosurgery for Psychiatric Disorders from General Office of Ministry of Health (China) 2008 “Neurosurgery for psychiatric disorders can only be used in “refractory obsessive-compulsive disorder, depression and anxiety disorder” that, as “undisputed among international medical societies,” is “not responding to long-term standard non-surgical treatment” and is “causing severe family and social devastation.” “[Neurosurgery] is not a standard therapy, and should be free of charge to the patients.” ( Wu, Gabriels, & Nuttin, 2012 ) |
Patient Autonomy | Case of Ms. V Due to religious practices, the patient and her family did not consent to a blood transfusion. Medical practitioners proceeded with the transfusion in order to save her life. Courts ruled that the doctors had infringed on her autonomy, and though this simple procedure saved her life, she had the right to refuse treatment (Zhang, Zhang, Zhang, & Wang, 2021) | Case of Ms. L The patient was in a coma and was not able to consent to an emergency surgery. Her husband refused to consent to the surgery, and the medical practitioners could not find a family member to consent for her; the patient's autonomy and right to consent was in the hands of her close relatives. They did not perform the surgery, as a result, the patient and her baby died. The courts ruled “if the opinions of patients or their close relatives cannot be obtained due to emergency situations such as rescuing patients in critical condition, corresponding medical measures can be adopted immediately with the approval of the leader or authorized person of the medical institution” (Zhang, et al., 2021) |
Given the challenges of acquiring court-ordered minimally invasive treatment, it is unlikely any mandates on a high-risk procedure, such as neuromodulation, will be feasible in western countries such as the U.S., although this may vary in other countries with a more authoritarian approach to healthcare (Fernandez-Ballesteros, et al., 2019). In all, there are not many legal statutes guiding psychosurgery. As medical advances are made, legal advancements must follow closely after. These legal advancements could be made through the work of international medical societies (Wu, Gabriels, & Nuttin, 2012). Examples include the World Society for Stereotactic and Functional Neurosurgery (WSSFN) and the Congress of Neurological Surgeons (CNS), as well as ethics-focused organizations such as International Neuroethics Society (International Neuroethics Society, 2022) and the Brain Initiative Neuroethics Working Group (NIH Brain Initiative, 2022) to construct guidelines for DBS to treat addiction. This is exemplified through the process in which DBS was considered as a treatment for OCD by the CNS (Hamani, et al., 2014). Such guidelines would need to be regularly updated to reflect medical evidence and best practice. Then, lawmakers can look to these guidelines to inform the legal structures they plan to put in place. The discussion of legal coercion of DBS may be a premature discussion, however these are the ethical and legal concerns that would arise once DBS is established as a safe, cost efficient, and effective treatment for addiction.
Conclusions
Although SUD is a major global social and medical concern, there are major limitations within the current treatment methods, urging the need for alternative approaches. While invasive neuromodulation techniques such as DBS shows promise in the treatment of addiction, numerous ethical and medico-legal issues must be considered. Here, we outlined the key aspects focusing on the use of DBS and made recommendations for stakeholders (clinicians, researchers, service providers, ethicists, and policy makers) involved in the care of these patients. However, given the complex social circumstances and physiological differences, each patient must be considered individually by a multidisciplinary team of experts. We hope the present review stimulates more studies to deeply understand the individual and societal benefits and risks of DBS to treat recalcitrant SUD refractory to conventional therapy.