Abstract
Comorbidity between post-traumatic stress disorder (PTSD) and substance use disorder may be explained by a prospective trauma risk conferred by both conditions. The current study modeled concurrent and prospective associations of trauma, PTSD symptoms, and substance use (SU) behavior among trauma exposed youth (ages 8-20). Clinical interviews assessed trauma exposure, PTSD symptom severity, and SU behavior at baseline and at six- and 12-month follow up study visits (N = 2,069). Structural equation models assessed the associations of trauma, PTSD symptoms, and SU behavior. Lifetime trauma was associated with more severe PTSD symptoms and SU behaviors, whereas trauma exposure during the study was only associated with PTSD symptoms. PTSD symptom severity was prospectively associated with trauma exposure. PTSD symptom severity and SU behavior at follow-up study visits were prospectively associated. These results highlight the dynamic interplay between trauma, PTSD symptoms, and SU behavior during youth, a developmental period during which complex psychiatric presentations can have longstanding consequences for health.
1. Introduction
Trauma exposure during early life is a leading epidemiological predictor of long-term morbidity and mortality (Moffitt et al., 2013). One prominent psychiatric presentation that is associated with early life trauma is comorbid post-traumatic stress disorder (PTSD) and substance use disorder (SUD; Dell’Aquila and Berle, 2023; Kilpatrick et al., 2003), a comorbidity with a high disease burden that presents unique challenges for treatment (Gilpin and Weiner, 2017; Hien et al., 2024). Although the role of trauma in the temporal onset of comorbid PTSD and SUD has been well researched, less is known about how recurrent trauma perpetuates the co-expression of symptom severity once PTSD and problematic substance use behaviors have emerged, particularly during youth development.
Early life trauma has been identified as a risk factor for PTSD or SUD in both retrospective and longitudinal studies (Carliner et al., 2016; Kirsch et al., 2020; Moustafa et al., 2021; Pratchett and Yehuda, 2011). Although single instances of trauma can cue the emergence of PTSD or SUD, both PTSD and SUD are more likely to occur among individuals with multiple trauma exposures (Dell’Aquila and Berle, 2023; Hoffmann and Jones, 2022; Kolassa et al., 2010). The increased likelihood of comorbid PTSD and SUD is magnified among people who have experienced repetitive interpersonal traumas specifically, such as sexual assault, caregiver abuse, or bullying, and among individuals who have accrued multiple types of trauma exposures (Blanco et al., 2013; Dell’Aquila and Berle, 2023; Fetzner et al., 2011). The correlation between cumulative trauma exposure and the likelihood of comorbid PTSD and SUD highlights recurrent trauma as a risk factor for complex psychopathology.
Moreover, both PTSD and SUD have been identified as independent risk factors for subsequent trauma exposure (Dardis et al., 2021; Espelage et al., 2018; Jaffe et al., 2019). The prospective risk for trauma conferred by PTSD and SUD is underpinned by changes in threat processing and cognitive processes that contribute to risk taking (Cisler et al., 2015; Testa and Livingston, 2009). Indeed, PTSD symptoms and alcohol use have been shown to mediate the longitudinal association between sexual assault and sexual revictimization among college age women (Cusack et al., 2021; Messman-Moore et al., 2009; Ullman et al., 2009). In addition to indicating that PTSD and SUD independently confer risk for trauma exposure, these findings suggest that concurrent PTSD and SUD may compound the risk for recurrent trauma exposure.
The current study sought to extend the extant research by using a longitudinal dataset from a large sample of trauma exposed youth to model the prospective associations of trauma, PTSD symptoms, and substance use (SU) behaviors. Much of the longitudinal research on how trauma contributes to concurrent PTSD and SU behavior is derived from adult populations and research among youth has been predominately cross-sectional (Carliner et al., 2016; McCart et al., 2011). As such, the longitudinal design of the current study contributes novel insight into the etiology of PTSD and SU behavior during a sensitive period of development when many psychiatric conditions first emerge and shape future risk. Indeed, adolescent PTSD is thought to alter neural development (Cisler and Herringa, 2021) and substance use during adolescence is associated with an increased incidence of lifetime SUD (Kirsch and Lippard, 2022). The results of this study will thus elucidate the longitudinal sequala of trauma, PTSD symptoms, and SU behaviors among trauma-exposed youth and inform the broader literature which links early life trauma to health outcomes.
2. Methods
2.1. Procedures
This study used data collected by the Texas Childhood Trauma Research Network (TX-CTRN), overseen by the Texas Child Mental Health Care Consortium (TCMHCC), at twelve academic medical centers across the state. Complete details of the study procedures are described in the publicly available study protocol (Nemeroff and Wagner, 2023). All study procedures were approved by the Institutional Review Board (IRB) at The University of Texas Southwestern and instantiated via IRB reliance agreements with the other eleven institutions. In brief, youth (aged 8–20 years) were recruited from outpatient and inpatient psychiatric settings, emergency departments, primary care clinics, and community mental health centers. Youth that were interested in the study were referred to research personnel and screened for eligibility. Youth (and/or their caregiver) provided informed consent (or assent as applicable) prior to screening. Screening visits were conducted both in person and remotely, contingent on logistical constraints. Study staff screened youth for the presence of at least one qualifying trauma exposure, language comprehension (either English or Spanish), psychotic symptoms, developmental disorders, and severe intellectual disability. Eligible youth that enrolled in the study were then scheduled for a baseline visit and six subsequent follow-up study visits (1-, 6-, 12-, 18, and 24-months).
Trained study staff (Shahidullah et al., 2023) administered psychometric assessments at each study visit. Structured interviews were used to measure youth’s experiences of trauma, PTSD symptoms, and substance use. Trauma exposure was measured at the baseline, 6-, 12-, 18-, and 24-month study visits. PTSD symptoms and substance use were measured at all six study visits. During the baseline study visit, family health history and household demographics were self-reported by caregivers or youth (if age >= 17 and participating in the study alone). Youth aged 8–11 were assisted with personal health history self-report measures by the study staff.
Recruitment for the CTRN registry is ongoing, and the current study utilized data collected from participants who completed their first baseline visit between October 2020 and October 2023. The current analysis used data from the baseline, 6-, and 12-month study visits due to the progression of participants through the study protocol at the time of publication (i.e., excludes 18- and 24-month visits due to sample size) and because trauma exposure was not assessed at the 1-month study visit. To ensure the longitudinal fidelity of the study’s time course, data from follow-up study visits were retained for analysis if the study visit occurred within (+/−) 30 days of the scheduled study visit.
2.2. Measures
2.2.1. Trauma exposure
The Traumatic Events Screening Inventory for Children (TESI-C) was administered by trained interviewers to measure youth’s trauma exposure (Ford et al., 2000). Youth reported if they had been exposed to any of the 20 types of experiences. At the baseline interview, youth reported lifetime exposure. At the follow-up study visits, youth reported if they had been exposed to each item during the 6-months since the previous study visit. Youth’s descriptions of endorsed items were used to determine if the exposure met Diagnostic and Statistical Manual (5th edition; DSM-5; American Psychiatric Association, 2013) PTSD criterion A (i.e., was an event that involved actual or threatened death or injury, or a threat to the physical integrity of self or others; Aksan et al., 2024). Item responses were coded as binary exposures if the exposure met criterion A (1 = exposed, 0 = not exposed) and a sum score was calculated for each study visit.
2.2.2. Symptoms of post-traumatic stress disorder
The Clinician-Administered PTSD Scale for DSM-5 Child/Adolescent Version (CAPS-CA-5) indexed symptoms of post-traumatic stress disorder during the previous 30-days (Pynoos et al., 2015). Trained interviewers administered the CAPS-CA-5 in a structured interview format to generate severity scores for each of the 20 items which comprise the four major subcategories of PTSD symptoms (re-experiencing, avoidance, negative alterations in cognition and mood, and arousal and reactivity). Severity scores for each item could range between 0 and 4. Severity scores were summed across all 20 items to create a total PTSD symptom severity score which could range between 0 and 80. The PTSD symptom severity score, not a binary PTSD diagnosis, was used for analysis.
2.2.3. Substance use behaviors
Youth substance use behaviors were measured via the CRAFFT 2.1 + N (Car, Relax, Alone, Forget, Friends, Trouble: Version 2.1+ Nicotine; The Center for Adolescent Behavioral Health Research, 2021). The baseline visit referred to substance use behaviors during the previous 12-months, whereas the follow-up study visits referred to substance use since the previous study visit. The first four items assessed the number of days that alcohol, cannabis products, nicotine, or other drugs were used. Participant’s reports of the number of days on which substances were consumed were transformed into binary responses (1 = endorsed use for that category; 0 = did not endorse use for that category). The remaining six items (1 = yes; 0 = no) indexed substance use behaviors that are considered indicators for substance use disorder. The six items were summed to create a substance use behavior score (range between 0 and 6). The sum score does not constitute a diagnosis of substance use disorder, although previous research suggests that a score of two or above constitutes a high likelihood of having a SUD as defined by DSM criteria (Mitchell et al., 2014).
2.3. Data analysis
Statistical analyses were executed using R statistical software, version 4.3.1. The analytic sample size for each study visit is shown in Table 1 (baseline n = 2069, 6-month study visit n = 1055, 12-month study visit n = 797). The proportion of missing data ranged from 0 % to 63 % contingent on the specific variable and study visit (i.e., there were higher rates of missing data at follow-up study visits given more participants had not matriculated to those study visits, see Supplemental Table 1 for rates of missing data per variable). Little’s missing completely at random test (Little, 1988a; Tierney and Cook, 2023) suggested that the missing data were not missing completely at random (χ2(2, 966) = 3612.81, p < .001). To accommodate missing data, multiple imputation was performed prior to analyses using the predictive mean matching algorithm (Little, 1988b) implemented in the “mice” package (van Buuren and Groothuis-Oudshoorn, 2011). All variables assessed at the baseline visit were used to impute missing baseline data. Missing data from follow-up study visits were not imputed and were accommodated with full information maximum likelihood estimation. The “lavaan” package (Rosseel, 2012) was used to fit cross-lagged panel models (CLPM) on all imputed datasets and parameter estimates were pooled across imputations (n = 100). The Satterthwaite method was used to produce robust standard errors and test statistics. Chi-square difference tests, root mean square error of approximation (RMSEA), the comparative fit index (CFI), the standardized root mean square residual (SRMR), and R2 values were used to compare model fit.
Table 1.
Descriptive statistics for participant demographics and variables of interest from the observed cases at each study visit.
Baseline N= 2069 | 6-months N= 1055 | 12-months N= 797 | |
Age | 15.25 (3.37) | 15.63 (3.34) | 15.98 (3.36) |
Sex (female) | 59 % | 60 % | 59 % |
Race | |||
White | 67 % | 66 % | 67 % |
Black | 14 % | 14 % | 14 % |
Other | 7 % | 7 % | 6 % |
Multiracial | 13 % | 13 % | 13 % |
Hispanic | 48 % | 44 % | 44 % |
Household income | |||
< $25,000 | 42 % | 36 % | 37 % |
$25,000 – $99,999 | 39 % | 42 % | 40 % |
> $99,999 | 19 % | 22 % | 22 % |
Family history | |||
Psychiatric disorders | 53 % | 57 % | 59 % |
Substance use disorder | 23 % | 23 % | 22 % |
Criterion A lifetime trauma | 4 (0–18) | – | – |
1–4 | 54 % | – | – |
5–8 | 33 % | – | – |
9–12 | 10 % | – | – |
13+ | 2 % | – | – |
Criterion A trauma exposure between study visits | – | 0 (0–8) | 0 (0–8) |
1 | – | 22 % | 26 % |
2 | – | 12 % | 9 % |
3 | – | 5 % | 6 % |
4+ | – | 5 % | 4 % |
PTSD symptom severity | 16.85 (13.75) | 10.09 (11.96) | 9.96 (11.62) |
SU behaviors | 0.82 (1.47) | 0.65 (1.34) | 0.63 (1.35) |
Substance use | |||
No substance use | 70 % | 71 % | 73 % |
Monosubstance use | 12 % | 11 % | 10 % |
Tobacco | 1 % | 1 % | 1 % |
Alcohol | 8 % | 8 % | 7 % |
Cannabis | 3 % | 3 % | 2 % |
Other | 0.2 % | 0.1 % | 0.1 % |
Polysubstance use | 18 % | 18 % | 17 % |
Tobacco | 12 % | 12 % | 11 % |
Alcohol | 16 % | 17 % | 16 % |
Cannabis | 16 % | 17 % | 15 % |
Other | 4 % | 4 % | 5 % |
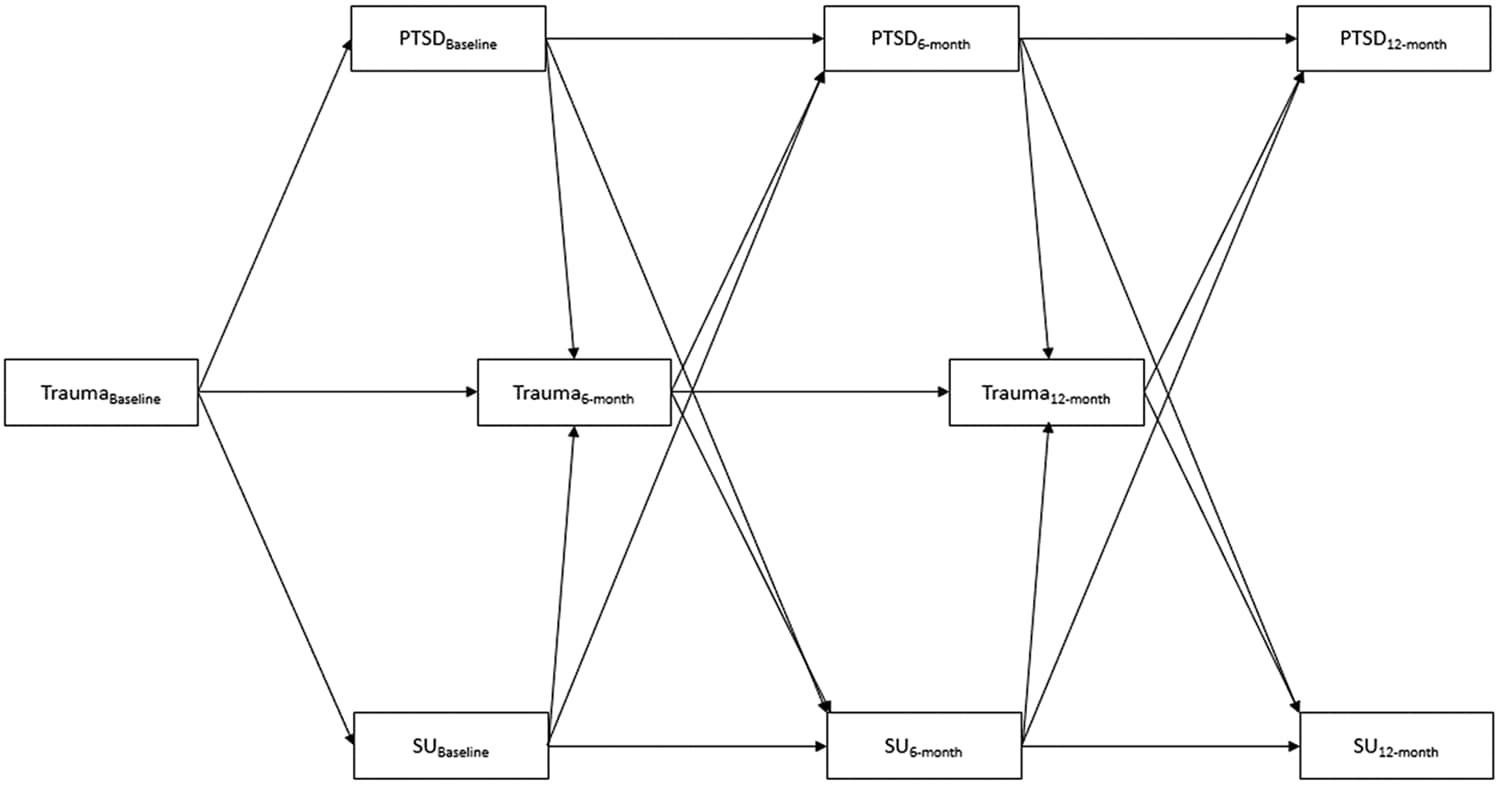
Two CLPMs were fit for the primary analyses. The first model included only trauma exposure, PTSD symptom severity, SU behaviors and the respective autoregressive and cross-lagged associations (Fig. 1). The second model added age at baseline, sex assigned at birth, Hispanic ethnicity, race (White, Black, multiracial, other; the other category collapsed the Asian, American Indian or Alaska Native, and Native Hawaiian or Pacific Islander participants into a single group for sample size concerns), household income (< $25,000, $25,000-$99,999, > $99,999), and family histories of psychiatric and substance use disorders to the regression equations as control variables. Although random-intercept CLPMs (RI-CLPM) are generally favored over CLPMs (Hamaker et al., 2015), attempts to fit a RI-CLPM were stymied by pooled Heyward cases and model convergence issues. As such, the analyses consisted of a random-intercepts CLPM with the variances and covariances of the random-intercepts for trauma, PTSD symptoms, and SU behaviors constrained to zero. This analytic strategy is equivalent to a CLPM (Mulder and Hamaker, 2021), and thus assessed how youth’s value (ie., trauma exposure, PTSD symptoms, SU behaviors) for a given construct at one timepoint predicted their value on constructs assessed at subsequent study visits.
3. Results
3.1. Descriptive statistics
Table 1 presents the sample demographics and descriptive statistics for the observed cases at each study visit. Participants (mean age=15.25, SD = 3.37; 59 % female) were from households that spanned the socioeconomic spectrum (42 % had household incomes < $25,000). Most participants identified as White (67 %), and a relatively large percentage of participants identified as Hispanic (48 %) or as a racial minority (33 %). All participants were exposed to at least one qualifying trauma as a condition of study participation; nevertheless, most youth had been exposed to more than one type of criterion A trauma during their lifetime (90.6 %). Between study visits, nearly half of youth were exposed to one or more types of criterion A traumas (baseline to 6-month study visit = 42.9 %, six-month to 12-month study visit = 45.1 %). The range of trauma exposures was larger for lifetime trauma (0–18 exposures) than the range of trauma exposures between study visits (0–8). Most participants displayed some number of PTSD symptoms (i.e., > 0, baseline = 93.1 %, 6-month study visit = 76.5 %, 12-month study visit = 72.3 %). Most youth did not engage in substance use during the study (70–73 %). Of youth who engaged in substance use, most engaged in polysubstance use (17–18 %) as opposed to monosubstance use (10–12 %).
3.2. Primary analyses
The initial CLPM (χ2(55) = 291.24, p < .001, RMSEA = 0.084, CFI = 0.127, SRMR = 0.106) which included the autoregressive and cross-lagged associations accounted for significant amounts of variance in youth’s trauma exposure (lifetime trauma R2 = 0, six-month R2 = 0.159, 12-month R2 = 0.205), PTSD symptom severity (baseline R2 = 0.338, six-month R2 = 0.490, 12-month R2 = 0.617), and SU behaviors (baseline R2 = 0.092, six-month R2 = 0.501, 12-month R2 = 0.514). The covariate adjusted CLPM fit the data well (χ2(9) = 43.82, p < .001, RMSEA = 0.079, CFI = 0.872, SRMR = 0.017) and significantly improved model fit (χ2(46) = 236.91, p < .001) compared to the initial CLPM (see Supplemental Table 2for covariate parameter estimates). Covariates principally improved model fit by accounting for variance of trauma exposure, PTSD symptom severity, and SU behaviors at the baseline study visit (lifetime trauma ΔR2 = 0.225, PTSD symptoms ΔR2 = 0.076, SU behaviors ΔR2 = 0.089), as opposed to the six- (trauma ΔR2 = 0.021, PTSD symptoms ΔR2 = 0.044, SU behaviors ΔR2 = 0.011) or 12-month study visits (trauma ΔR2 = 0.021, PTSD symptoms ΔR2 = 0.017, SU behaviors ΔR2 = 0.008).
In the covariate-adjusted model (see Fig. 2), all three constructs had significant and positive autoregressive associations across the course of the study (all p <= 0.004). Youth with higher levels of lifetime exposure to traumatic events were more likely to exhibit SU behaviors (b = 0.08, p = < 0.001) and more severe PTSD symptoms at the baseline visit (b = 1.96, p < .001). Trauma exposure between study visits was not significantly associated with SU behaviors at the follow-up study visits (p >= 0.083). Likewise, SU behaviors at baseline and the 6-month study visit were not significantly associated with prospective trauma exposure between study visits (p >= 0.123). Trauma exposure between study visits was positively associated with PTSD symptoms at the six- (b = 2.47, p < .001) and 12-month study visits (b = 1.57, p < .001). Moreover, PTSD symptoms at the baseline (b = 0.02, p = .007) and six-month study visits (b = 0.02, p = .001) were prospectively associated with more trauma exposure between study visits. PTSD symptoms (b = 0.01, p = .046) and SU behaviors (b = 0.69, p = .023) at the six-month study visit were prospectively, and reciprocally, associated at the 12-month study visit. Symptoms of PTSD and SU behaviors were positively correlated within study visits (all p <= 0.059). The unstandardized regression coefficients from the unadjusted and adjusted models are shown in Table 2.
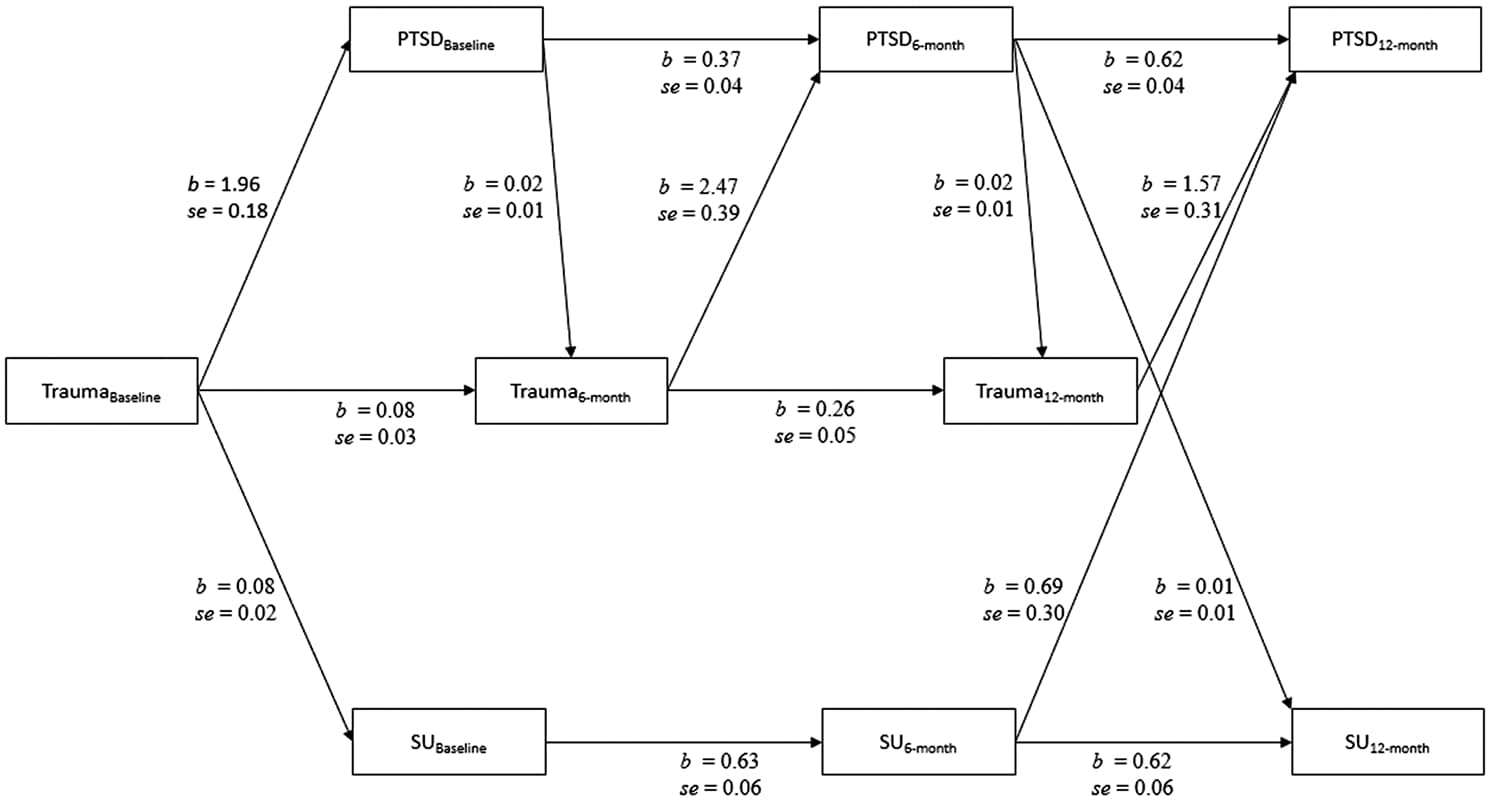 Table 2
Table 24. Discussion
This study used a large longitudinal sample of trauma exposed youth to assess the role of trauma exposure on the associations between PTSD symptom severity and SU behaviors. Lifetime trauma exposure was associated with baseline levels of both PTSD symptom severity and SU behaviors, whereas recurrent trauma only contributed to PTSD symptom severity. PTSD symptoms severity and SU behaviors exhibited reciprocal associations at follow up study visits. These prospective results generally support extant cross-sectional research that links trauma to elevated PTSD symptoms and SU behaviors (Carliner et al., 2016; Dell’Aquila and Berle, 2023; Kilpatrick et al., 2003), but also indicate that the causal pathways between trauma, PTSD symptoms, and SU behaviors remain to be fully elucidated among youth.
Lifetime trauma exposure was a risk factor for PTSD symptoms and SU behaviors in this trauma selected population. Specifically, we observed that lifetime trauma exposure was associated with more PTSD symptom severity and SU behaviors at the baseline study visit. These findings are consistent with a broad literature that finds individuals who exhibit SU behavior and more severe PTSD experience higher rates of early life trauma than individuals who do not engage in SU behaviors or who do not exhibit PTSD symptoms (Carliner et al., 2016; Kirsch et al., 2020; Moustafa et al., 2021; Pratchett and Yehuda, 2011).
Recurrent trauma exposure during the study was linked to higher levels of PTSD symptom severity, but not SU behaviors. These findings indicate that additional trauma exposure contributes to worse PTSD symptoms among youth previously exposed to trauma, a finding consistent with extant literature (Dell’Aquila and Berle, 2023; Kolassa et al., 2010). These results also suggest that trauma exposed youth, although at a higher risk for engaging in SU behavior generally, are not more likely to engage in substance use following subsequent trauma exposures. This interpretation highlights the importance of investigating pathways to SU behavior beyond trauma exposure, such as coping with subjective distress (Boness et al., 2021).
PTSD symptoms, but not SU behaviors, acted as a prospective risk factor for recurrent trauma exposure. Baseline PTSD symptoms significantly predicted more trauma exposure between the baseline and the six-month study visits. Likewise, PTSD symptoms at the six-month study visit were associated with more trauma exposure between the six- and 12-month study visits. These observations support the idea that PTSD symptoms may increase subsequent trauma exposure (Jaffe et al., 2019); which may potentially be related to perturbations in cognition and threat processing (Cisler et al., 2015). In contrast, there was no evidence to indicate that SU behaviors increased trauma exposure between study visits, which is consistent with another large study of adolescents (Patel et al., 2024). These results suggest that PTSD symptoms and SU behaviors may confer differential increases of prospective trauma exposure risk. Moreover, these findings indicate that clinical interventions which reduce recurrent trauma exposure could have potential to mitigate PTSD symptom severity across time.
Youth’s PTSD symptom severity and SU behavior were significantly associated throughout the course of the study. Within each study visit, PTSD symptom severity and SU were positively associated, consistent with a range of literature that highlights high comorbidity of PTSD and SUD and cross-sectional associations between PTSD and problematic substance use behavior (Brady et al., 2021; Dell’Aquila and Berle, 2023; Smith et al., 2016). PTSD symptom severity and SU behavior also exhibited prospective associations, although only at select timepoints. Specifically, baseline PTSD symptoms and SU behaviors were not prospectively associated with each other at the six-month study visit, whereas PTSD symptoms and SU behaviors at the 6-month study visit were, respectively, positively associated with SU behaviors and PTSD symptoms at the 12-month study visit. These findings support previous adolescent literature that finds PTSD symptoms and SU behaviors are prospectively associated (Conway et al., 2016; Haller and Chassin, 2014), but also suggest that these associations may not be constant across development or may only manifest during specific temporal windows. The temporal specificities of these findings highlight the importance of longitudinal study designs for understanding the etiology of complex psychiatric presentations during development.
4.1. Strengths and limitations
A major strength of this study was the use of clinical interviews to index trauma exposure and PTSD symptoms. The trauma interviews allowed the current study to classify trauma exposure as an event which was perceived or experienced as having the potential to inflict life threatening injury or death. Similarly, the clinical PTSD interview ensured that youth were able to comprehend and provide valid responses. These aspects of the study design ensured the validity of the core measurements, which contribute novel observations of the prospective associations between trauma, PTSD symptoms, and SU behavior among youth.
Consideration should be given to the measure of substance use implemented in the current study. The effects observed herein are relative to a commonly used screening tool validated among American youth and which broadly indexes substance use behavior without respect to specific substances. Caution is thus warranted in generalizing these non-substance specific observations to usage patterns for specific substances.
5. Conclusion
The current study used a large sample of trauma exposed youth to assess the joint levels of trauma exposure, PTSD symptoms, and SU behaviors across 12-months. The results suggested that lifetime trauma exposure is associated with PTSD symptoms and SU behaviors and that recurrent traumas contribute to increased PTSD symptoms. The current study did observe that PTSD symptoms and SU behaviors were prospectively associated, although only at specific points during the study. There was also evidence that PTSD symptom severity contributed to trauma exposure risk. Together the results of this study provide insight into the causal pathways that link trauma to the concurrent presentation of PTSD symptoms and SU during youth development.