Abstract
The intersection of traumatic brain injury (TBI), substance use, and mental health disorders presents a significant challenge within the incarcerated female population, where rates of these conditions are alarmingly high. This paper explores the multifaceted relationships among TBI, substance use, and mental health disorders, emphasizing the impact of intergenerational trauma on this vulnerable group. Women in correctional facilities often experience a history of trauma, exacerbating their mental health challenges and increasing the likelihood of substance use as a maladaptive coping mechanism. The cumulative effects of TBI can further complicate their psychological and emotional well-being, leading to a cycle of trauma that is perpetuated across generations. Through a review of current literature and case studies, this paper advocates for the implementation of neuropsychological rehabilitation programs that address the unique needs of incarcerated women. Such interventions are crucial not only for improving individual outcomes but also for breaking the cycle of trauma that affects families and communities. Recommendations for policy reforms and future research directions are provided to enhance the efficacy of rehabilitation efforts and support the reintegration of these women into society.
INTRODUCTION
Background on the Prevalence of Traumatic Brain Injury (TBI), Substance Use, and Mental Health Disorders
TBI poses a significant public health concern, particularly among incarcerated women, who are reported to experience higher rates of TBI compared to their male counterparts. Each year, approximately 1.5 million Americans sustain a TBI, with women disproportionately affected by violence-related head injuries, often resulting from intimate partner violence (Haag et al., 2022), as represented in Figure 1. The consequences of TBI extend beyond physical injuries, significantly impacting cognitive and emotional functioning.
In addition to TBI, substance use prevalence within this demographic is alarmingly high. Over 20% of noninstitutionalized adults with a history of substance use disorder have experienced at least one TBI (Adams & Corrigan, 2019). This relationship between TBI and substance use creates a vicious cycle, where individuals often resort to substance use as a maladaptive coping mechanism to manage the symptoms associated with their injuries.
Furthermore, individuals with co-occurring TBI and mental health disorders face unique challenges that complicate their recovery. The neurological effects of TBI can exacerbate impulsive behaviors and hinder cognitive functioning, increasing vulnerability to substance misuse and mental health issues (Ayoola, et al., 2024). Understanding these interconnected issues is crucial for developing effective interventions tailored to this vulnerable population, ensuring that rehabilitation programs address the complexities of TBI, substance use, and mental health in a holistic manner. By doing so, we can better support the recovery and reintegration of incarcerated women facing these intertwined challenges. Figure 1 depicts a young woman lying in a hospital bed with visible medical equipment, including a breathing tube and monitoring devices, indicating a severe medical condition likely resulting from a TBI. This scenario highlights the significant public health concern posed by TBI, especially among incarcerated women, who tend to experience higher rates of such injuries compared to men. Each year, approximately 1.5 million Americans sustain a TBI, with a notable proportion of these injuries linked to violence, particularly intimate partner violence, which disproportionately affects women.
The presence of invasive medical equipment suggests serious complications arising from the injury, which can extend beyond physical damage to significantly impair cognitive and emotional functioning. The cyclical relationship between TBI and substance use is also critical; individuals often resort to substances as a maladaptive coping mechanism to manage the distressing symptoms of their injuries, exacerbating both mental health and substance use issues (Balogun, et al., 2024). This reinforces the necessity for holistic interventions that address the interconnected challenges of TBI, substance use, and mental health disorders, particularly for vulnerable populations like incarcerated women. Understanding and supporting their complex recovery needs is essential for improving their rehabilitation outcomes and successful reintegration into society.
Figure 1: Picture of a Female Patient Explaining the Impact of Traumatic Brain Injury (TBI) On Individuals. (Alison, R. 2023)
Overview of Intergenerational Trauma and Its Significance in This Context
Intergenerational trauma refers to the psychological and emotional effects of trauma that one generation experiences and subsequently transmits to future generations, significantly impacting their mental health and behavior. This phenomenon is particularly salient for incarcerated women, who often bear the weight of trauma not only from their own life experiences but also from the traumatic histories of their families (Owolabi, et al., 2024). Research has demonstrated that adverse childhood experiences, such as abuse, neglect, and systemic oppression, can have profound and lasting effects, leading to increased vulnerability to mental health issues, including anxiety, depression, and substance use in subsequent generations (Menzies, 2010).
In the context of women in prison, intergenerational trauma complicates their mental health challenges and can manifest in maladaptive coping strategies, such as substance use. This cycle of trauma not only perpetuates the mental health issues faced by these women but also contributes to ongoing cycles of incarceration (Dyer & Corrigan, 2021). The significance of understanding intergenerational trauma lies in its implications for intervention. By recognizing the multifaceted nature of trauma that spans generations, it becomes possible to develop targeted interventions that address both individual and familial histories of trauma (Bashiru, et al., 2024). Such approaches can foster resilience and recovery, breaking the cycle of trauma and incarceration, and promoting better mental health outcomes for incarcerated women and their families. This holistic understanding is crucial for designing effective rehabilitation programs that support healing at both the individual and generational levels.
Objectives
The primary objective of this paper is to investigate the intricate relationships among TBI, substance use, and mental health disorders in incarcerated women, specifically focusing on how intergenerational trauma influences these dynamics. By examining the historical context of trauma and its transmission across generations, this study aims to highlight the compounded effects on mental health and behavioral outcomes in this population as presented in table 1. Additionally, the paper seeks to identify effective neuropsychological rehabilitation strategies that address both individual and familial trauma histories, thereby promoting holistic recovery. Another key objective is to explore how social and environmental factors contribute to the perpetuation of trauma, substance use, and mental health issues, emphasizing the need for tailored interventions that consider the unique challenges faced by incarcerated women.
Table 1: Objectives of the Paper
Understanding Traumatic Brain Injury (TBI) Definition and Types of TBI
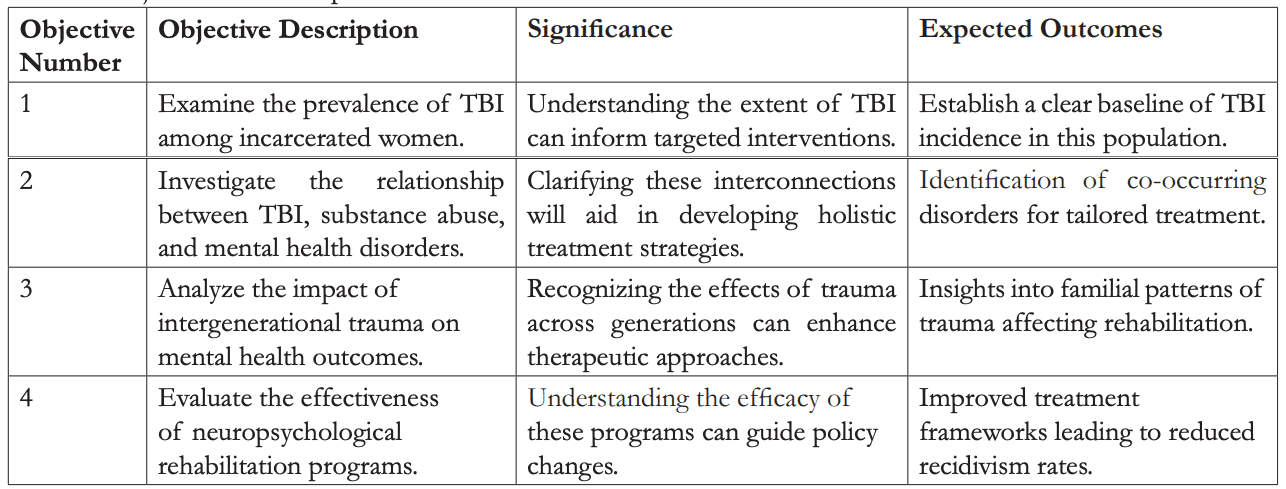
TBI is defined as a disruption in brain function resulting from an external force, which can include blows, bumps, or jolts to the head, or penetrating injuries caused by an object (Voss, et al., 2015) as represented in figure 2. TBIs are classified based on their severity into three main categories: mild, moderate, and severe. Mild traumatic brain injury (mTBI), commonly referred to as a concussion, typically leads to a brief loss of consciousness or a transient alteration in mental status. Symptoms may also include confusion, dizziness, and headaches, often resolving within a short period (Thurman & Alverson, 2022).
Moderate TBI is characterized by a loss of consciousness lasting between 30 minutes and 24 hours, often accompanied by neuroimaging findings that indicate structural injury to the brain, such as contusions or haemorrhages. Patients may experience prolonged cognitive deficits, including difficulties with memory, attention, and executive function.
Severe TBI involves a prolonged state of unconsciousness lasting more than 24 hours and is frequently associated with significant neurological deficits, including impaired motor functions and changes in behavior or cognition (Igba, et al., 2024). Understanding these classifications is essential for developing targeted interventions and rehabilitation strategies tailored to the needs of individuals affected by TBI, particularly in high-prevalence populations such as incarcerated women. Effective management of TBI is crucial for improving recovery outcomes and enhancing quality of life.
Figure 2 illustrates the concept of TBI by visually representing the impact on the brain when an external force causes injury. It highlights that TBI results from various causes, including blows or jolts to the head, as well as penetrating injuries. The diagram shows how the head moves back while the brain moves forward, indicating the motion that can lead to brain injuries, particularly in cases of mild traumatic brain injury (mTBI), commonly known as a concussion. This type of injury typically results in brief loss of consciousness or temporary alteration in mental status, with symptoms like confusion and headaches. The image also serves as a reminder of the different classifications of TBI: mild, moderate, and severe. Moderate TBI is characterized by longer loss of consciousness and cognitive deficits, while severe TBI often leads to prolonged unconsciousness and significant neurological impairments. Understanding these classifications is essential for developing targeted rehabilitation strategies, particularly for high-risk groups, such as incarcerated women, to enhance their recovery outcomes and quality of life.
Figure 2: Picture Showing the Concept of Understanding Traumatic Brain Injury (TBI). (Ravi, P. 2023)
Prevalence and Causes of TBI in Incarcerated Populations
TBI is alarmingly prevalent among incarcerated populations, with estimates suggesting that between 25% and 87% of inmates report a history of TBI. This prevalence is significantly higher than the 8.5% observed in the general population (Hughes, et al., 2015). The causes of TBI within correctional settings are multifaceted and often linked to the environments and lifestyles that lead to incarceration. Common causes include violent encounters, such as physical assaults or fights, which are frequent in prison settings, as well as falls and accidents that may occur during the chaotic circumstances of incarceration.
Substance use is another significant factor contributing to the high rates of TBI among incarcerated individuals, with many engaging in risky behaviors while under the influence. These risky behaviors not only increase the likelihood of sustaining a TBI but also impair cognitive function and decision-making abilities (Moore, et al., 2014). Moreover, individuals with a history of TBI are more prone to engage in impulsive actions, further elevating their risk for incarceration (Igba, et al., 2024). Understanding the prevalence and underlying causes of TBI in this context is crucial for developing effective interventions and support systems tailored to the unique needs of incarcerated individuals, ultimately improving their rehabilitation and long-term outcomes.
Effects of TBI on Cognitive and Emotional Functioning
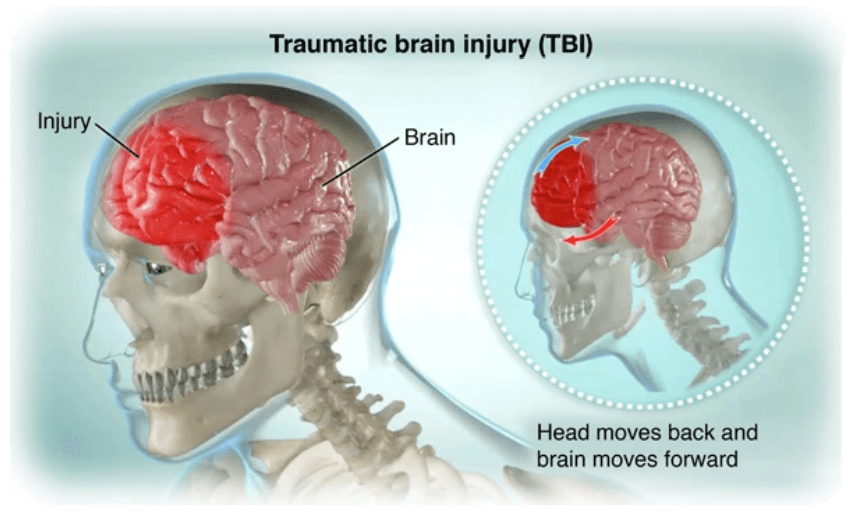
TBI significantly impacts cognitive and emotional functioning, leading to various deficits that complicate rehabilitation and daily life for affected individuals. Cognitive impairments associated with TBI are diverse, often including difficulties with attention, memory, problem-solving, and executive functioning. These deficits can severely hinder an individual’s ability to perform everyday tasks, such as managing finances, maintaining employment, or even engaging in social interactions (McGarry & Thangavel, 2021) as represented in figure 3.
Emotional disturbances are equally prevalent among individuals with TBI. Many reports experiencing heightened irritability, anxiety, depression, and mood swings as direct consequences of their injuries (Konrad, et al., 2011). These emotional challenges can exacerbate cognitive deficits, creating a complex interplay that further impairs overall functioning. For instance, difficulties with emotional regulation can lead to impulsive behavior, further complicating social relationships and rehabilitation efforts.
The cognitive and emotional sequelae of TBI can pose substantial barriers to successful reintegration into society, particularly in incarcerated populations, where such challenges may remain unrecognized or inadequately addressed (Enyejo, et al., 2024). Understanding these effects is crucial for developing effective interventions that cater to the unique needs of individuals with TBI, especially within correctional settings. Tailored rehabilitation programs that focus on both cognitive and emotional recovery are essential for promoting the wellbeing and reintegration of these individuals into their communities.
Substance Use among Incarcerated Women Overview of Substance Abuse Trends in Incarcerated Women
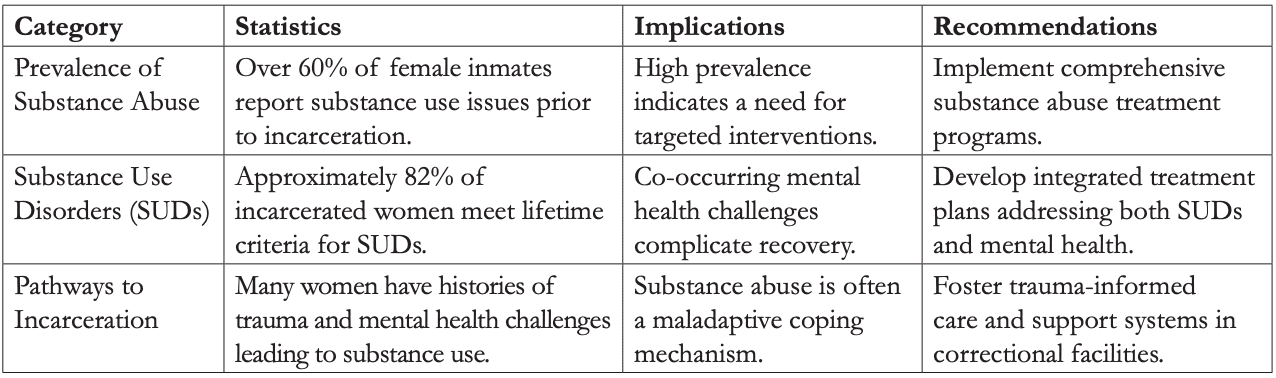
Substance use represents a critical issue among incarcerated women, significantly contributing to their overrepresentation in the criminal justice system. Research shows that women are more likely than men to be incarcerated for drug-related offenses, reflecting the pervasive nature of substance use disorders (SUDs) in this population. Notably, over 60% of female inmates report substance use issues prior to their incarceration (Bendlin & Moore, 2021) as presented in table 2. The prevalence of SUDs among incarcerated women is alarmingly high, with studies indicating that approximately 82% meet lifetime criteria for problematic drug or alcohol use or dependence (McConnell, 2017).
The pathways leading to incarceration for these women often involve complex histories marked by trauma, mental health challenges, and socio-economic factors that intersect with substance use, further complicating their rehabilitation needs (Enyejo, et al., 2024). Many incarcerated women have faced adverse childhood experiences, including physical and sexual abuse, which can predispose them to both substance use and criminal behavior. Given these trends, it is essential to develop targeted interventions and support systems within correctional facilities that address the unique challenges faced by women struggling with substance use. Such initiatives should include comprehensive treatment programs that integrate mental health services, traumainformed care, and skill-building opportunities to promote recovery and ultimately reduce recidivism. By addressing the root causes of problematic substance use in this population, rehabilitation efforts can be more effective, leading to improved outcomes for incarcerated women and their communities.
Figure 3 visually represents the multifaceted impacts of TBI on individuals’ cognitive and emotional health. At the center, it highlights two primary categories: Cognitive Impairments and Emotional Disturbances. Under cognitive impairments, the diagram elaborates on specific challenges, including difficulties with attention, memory issues, problem-solving challenges, and executive functioning deficits, all of which hinder daily tasks and overall functioning. In parallel, the emotional disturbances branch outlines issues such as heightened irritability, anxiety, depression, and mood swings, illustrating the emotional toll of TBI. The diagram further emphasizes the interplay between these cognitive and emotional challenges, indicating how cognitive deficits can exacerbate emotional issues, leading to impulsive behaviors and complicating social relationships. Lastly, it addresses the barriers to reintegration into society, showcasing the comprehensive effects of TBI that necessitate integrated and tailored rehabilitation approaches to support affected individuals effectively.
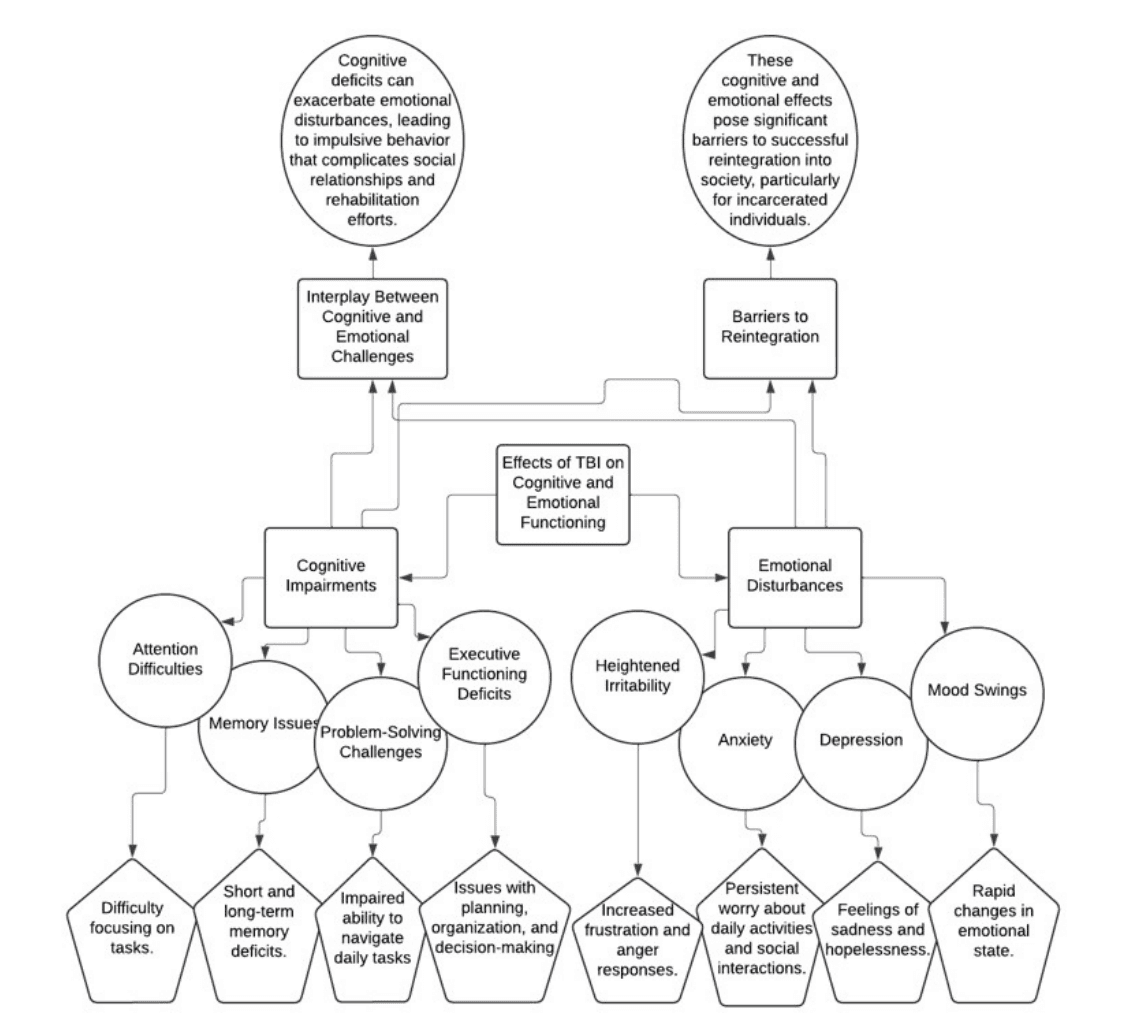
Figure 3: A diagram of Effects of TBI on Cognitive and Emotional Functioning
Table 2: Overview of Substance Abuse Trends in Incarcerated Women
Correlation between TBI and Substance Use
The correlation between TBI and substance use is well established, supported by substantial evidence indicating that individuals who have experienced a TBI are at a significantly higher risk of developing substance use disorders (SUDs). Following a TBI, individuals often exhibit behavioral changes such as impulsivity and disinhibition, which can lead to an increased likelihood of engaging in substance misuse (Graham, & Cardon, 2008). Studies have shown that more than half of individuals treated for TBI report substance use at the time of their injury, and many continue to misuse substances in the aftermath, exacerbating existing cognitive and emotional challenges (Graham, & Cardon, 2008).
This relationship is complex, as the neurological effects of TBI can impair decision-making abilities and emotional regulation, further heightening the risk of substance use as individuals attempt to cope with the psychological aftermath of their injuries. The interplay between TBI and substance use emphasizes the necessity for comprehensive assessments and tailored interventions that address both conditions simultaneously. A dual approach is essential for improving treatment outcomes and promoting recovery among individuals affected by TBI and substance misuse (Enyejo, et al., 2024). By recognizing and addressing the interconnected nature of these challenges, healthcare providers can enhance the effectiveness of rehabilitation efforts, ultimately supporting better long-term outcomes for affected individuals.
Impact of Substance Use on Mental Health
Excessive substance use has profound negative effects on mental health, particularly among incarcerated women who frequently experience co-occurring disorders. Research indicates that women with substance use disorders (SUDs) often exhibit symptoms of anxiety, depression, and other mental health issues, which can exacerbate existing conditions (Graham, & Cardon, 2008) as represented in figure 4. This vulnerability is further compounded by the self-medication hypothesis, which suggests that individuals may turn to substances as a means to alleviate psychological distress. However, this coping strategy can lead to a cycle of dependency that ultimately worsens mental health outcomes.
Additionally, the use of substances can trigger or intensify psychiatric symptoms, including psychosis and severe mood swings, complicating treatment efforts (Graham, & Cardon, 2008). For incarcerated women, the interplay between substance use and mental health issues is particularly concerning, as it not only affects their overall well-being but also complicates rehabilitation efforts and increases the likelihood of recidivism. Integrated treatment approaches that address both substance use and mental health simultaneously are essential, as failing to consider these interconnected issues may hinder recovery. Understanding these dynamics is critical for developing effective interventions tailored to the unique needs of this population, ensuring that treatment plans comprehensively address both substance use and underlying mental health disorders.
Table 3: Common Mental Health Disorders Observed in Incarcerated Women
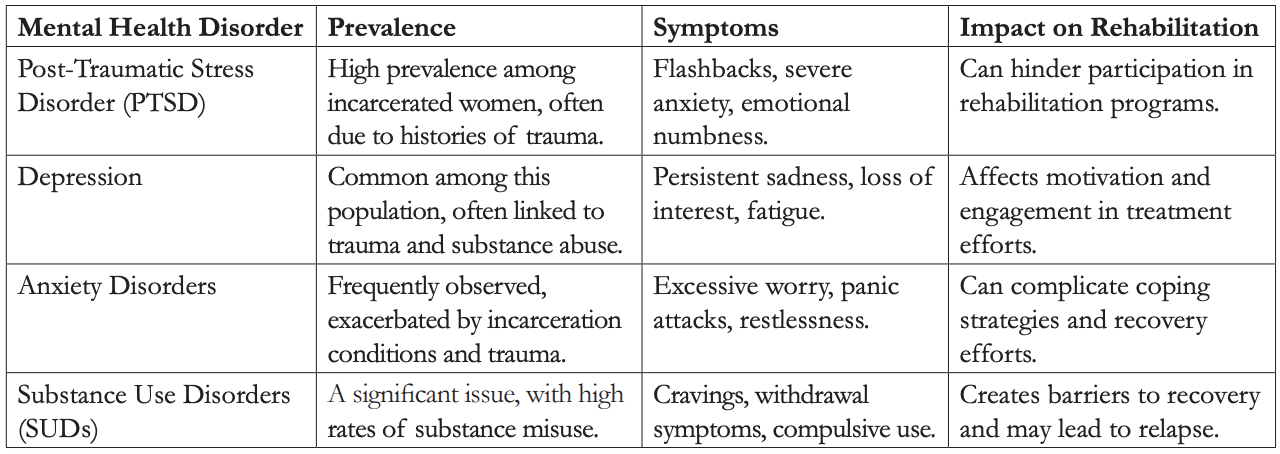
Mental Health Disorders in Incarcerated Women Common Mental Health Disorders Observed in This Population
Incarcerated women frequently experience a range of mental health disorders, with significantly higher prevalence rates compared to their male counterparts and the general population. Notably, studies indicate that approximately 66% of women in prison report having a history of mental health problems, including serious mental illness (SMI), PTSD, and substance use disorders (SUD) (Green et al., 2005; Walmsley, 2015) as presented in table 3. Common mental health disorders observed in this population include major depressive disorder, anxiety disorders, and bipolar disorder. The high rates of PTSD among incarcerated women, often stemming from histories of trauma and abuse, further complicate their mental health landscape (Idoko, et al., 2024). Additionally, many women exhibit symptoms of multiple comorbid disorders, necessitating integrated treatment approaches that address their unique psychological and social needs, particularly in the context of their incarceration and subsequent rehabilitation (Okeke, et al., 2024). Understanding these mental health challenges is crucial for developing effective interventions tailored to this vulnerable population.
Figure 4 illustrates the multifaceted effects that substance use has on mental health, highlighting the complex interplay between various negative outcomes and cooccurring disorders. At the center, it emphasizes the overarching theme of negative effects stemming from substance use, which branches into several critical areas, including increased anxiety, depression, mood swings, and impaired coping mechanisms. Each of these aspects underscores how substance use can exacerbate mental health issues, leading to heightened emotional instability and diminished resilience. The diagram also features a section on co-occurring disorders, detailing how substance use can exacerbate pre-existing mental health conditions and contribute to the development of new disorders. Additionally, it illustrates the vicious cycle that emerges from the interplay between substance use and mental health challenges, indicating how these factors reinforce one another and complicate the recovery process. This comprehensive overview highlights the urgent need for integrated treatment approaches that address both substance use and mental health simultaneously to improve overall outcomes for affected individuals.
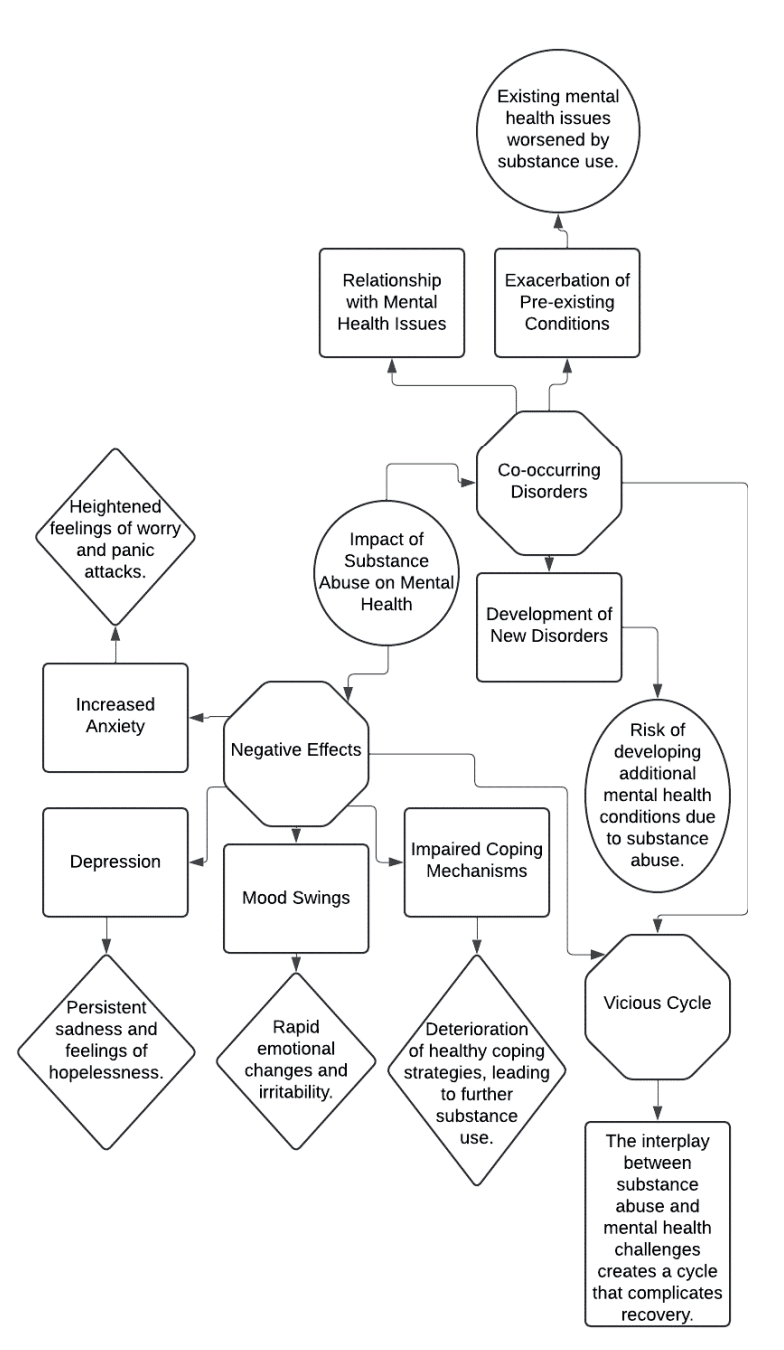
Figure 4: A diagram of Impact of substance use on mental health
The Relationship between TBI, Substance Use, and Mental Health Disorders
The relationship between TBI, substance use, and mental health disorders is complex and multifaceted, necessitating a comprehensive understanding of how these elements interact. Individuals who sustain a TBI are at an increased risk for developing substance use disorders, with studies indicating that more than 50% of TBI patients report substance use at the time of injury (Allen, et al., 2016) as represented in figure 5. This high prevalence suggests a significant overlap between these conditions, with individuals often using substances as a coping mechanism for the psychological distress associated with TBI.
The neurological impairments resulting from TBI can exacerbate pre-existing mental health issues, leading to a higher prevalence of conditions such as anxiety depression, and post-traumatic stress disorder (PTSD) (Allen, et al., 2016). The cognitive deficits associated with TBI, including impaired judgment and emotional regulation, further complicate the treatment landscape. Conversely, substance use can hinder cognitive recovery and worsen psychiatric symptoms, creating a vicious cycle that complicates rehabilitation efforts.
This interplay underscores the necessity for integrated treatment approaches that address TBI, substance use, and mental health simultaneously. Such holistic strategies are particularly crucial for populations with high incidence rates of these issues, such as incarcerated women (Ijiga, et al., 2024). By focusing on the interconnectedness of these conditions, effective interventions can be developed to improve outcomes and facilitate recovery for affected individuals, ultimately enhancing their quality of life and chances of successful reintegration into society.

Figure 5: Picture of a Person Struggling with The Heavy Burden of Substance Use Connecting to Mental Health. (Saad, 2023).
Figure 5 depicts a person in distress, hunched over and holding their head in their hands, surrounded by various drug paraphernalia laid out on a reflective surface. This powerful visual represents the complex relationship between TBI, substance use, and mental health disorders. Individuals who sustain a TBI are at an increased risk of developing substance use disorders, with studies indicating that a significant number of TBI patients report substance use at the time of injury. This prevalence reflects how many individuals turn to substances as a coping mechanism to manage the psychological distress stemming from their injuries. The image further symbolizes the dual challenges faced by those with TBI, as the neurological impairments can exacerbate preexisting mental health conditions like anxiety, depression, and PTSD. Cognitive deficits resulting from TBI, such as impaired judgment and emotional regulation, complicate treatment efforts. Additionally, substance use can hinder cognitive recovery, creating a vicious cycle that poses significant barriers to rehabilitation.
This interplay highlights the necessity for integrated treatment approaches that concurrently address TBI, substance use, and mental health, especially in populations with high incidence rates, such as incarcerated women. By focusing on the interconnectedness of these conditions, effective interventions can be designed to improve outcomes, facilitate recovery, and enhance overall quality of life for affected individuals.
The Role of Trauma in Exacerbating Mental Health Issues
Trauma plays a critical role in exacerbating mental health issues, particularly among incarcerated women, who frequently endure high levels of adverse life events. Research indicates that traumatic experiences, such as physical and sexual abuse, are prevalent in the histories of these women, leading to a significant burden of psychological distress (Green et al., 2005) as represented in figure 6. The effects of trauma can manifest in various mental health disorders, including PTSD, depression, and anxiety. For many women, trauma can lead to dysregulation of emotional responses, resulting in heightened vulnerability to developing these mental health conditions.
Moreover, the cumulative impact of multiple traumas can create a cascade of mental health challenges, where individuals struggle with feelings of shame, guilt, and isolation, further compounding their distress. The interconnectedness of these experiences underscores the need for trauma-informed care that recognizes the unique circumstances faced by incarcerated women (Ijiga, et al., 2024). Understanding the role of trauma in shaping mental health outcomes is essential for developing effective treatment and rehabilitation strategies tailored to this population. Interventions that specifically address trauma and its effects can foster resilience and promote recovery, ultimately contributing to better mental health and well-being among incarcerated women as they navigate the complexities of their lives.
Figure 6 depicts a group of refugees walking along a train track, carrying their belongings, with an emphasis on the collective experience of migration. This visual representation aligns closely with the theme of trauma and its significant role in exacerbating mental health issues, particularly among vulnerable populations. The refugee experience is often multifaceted, involving various stages of trauma and stress that can lead to considerable psychological distress. For many individuals, including those who may eventually become incarcerated women, the traumatic experiences encountered during migration—such as violence, loss of family, and the uncertainty of their future—can have profound mental health implications. These experiences can manifest in various disorders, including PTSD, anxiety, and depression. The emotional toll of such trauma often results in dysregulation of emotional responses, leaving individuals vulnerable to developing further mental health conditions.
Figure 6: A Picture Showing the Profound Trauma of the Refugee Experience in Connection with Mental Health. (Carlos, F. M. 2012)
Table 4: Definition of Intergenerational Trauma and Its Relevance to Incarcerated Women
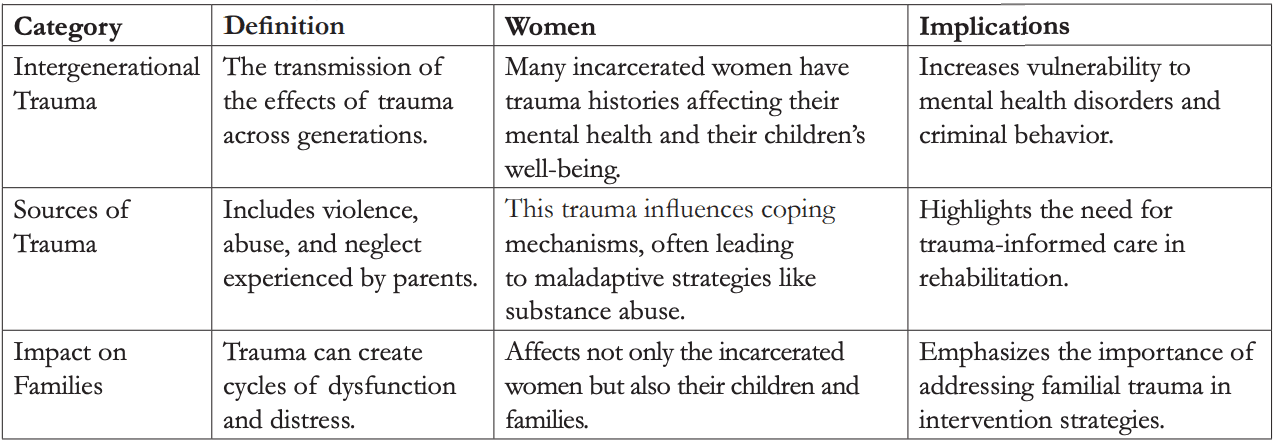
Intergenerational Trauma and Its Implications. Definition of Intergenerational Trauma and Its Relevance to Incarcerated Women
Intergenerational trauma refers to the transmission of the psychological and emotional consequences of traumatic experiences across generations, where the effects of trauma experienced by one generation are passed down to their children (Hancock et al., 2013) as presented in table 4. This phenomenon is particularly significant for incarcerated women, many of whom carry the weight of their own trauma histories, which not only affect their mental health but also the well-being of their children (Lünnemann, et al., 2019). Research indicates that women in prison often come from backgrounds characterized by violence, abuse, and neglect, contributing to cycles of trauma that perpetuate psychological distress and maladaptive coping mechanisms, such as substance use. The effects of intergenerational trauma can manifest in various ways, leading to increased vulnerability to mental health disorders, such as depression and anxiety, as well as engagement in criminal behavior. These dynamics underscore the urgent need for trauma-informed care that addresses both individual experiences and familial histories. Recognizing the interconnectedness of trauma across generations is crucial for developing effective interventions aimed at breaking the cycle of trauma and promoting healing (Ijiga, et al., 2024). By providing targeted support that encompasses the complexities of intergenerational trauma, we can better assist incarcerated women in their recovery journeys and contribute to healthier family dynamics. Understanding this relevance is vital for fostering resilience and improving overall outcomes for this vulnerable population.
The Cycle of Trauma and Its Impact on Families and Communities
The cycle of trauma has profound implications for families and communities, perpetuating patterns of dysfunction and distress across generations. Incarcerated women frequently carry histories of trauma that not only affect their own mental health but also have significant repercussions for their children and broader family systems (Bendlin & Moore, 2021). Research indicates that the trauma experienced by mothers can manifest in various behavioral and emotional challenges in their children, leading to increased risks of mental health issues, such as anxiety and depression, as well as a higher likelihood of engaging in criminal behavior in subsequent generations (Hancock et al., 2013).
This intergenerational transmission of trauma creates a cycle wherein families become trapped in patterns of use, neglect, and incarceration. The psychological burden faced by mothers can hinder their ability to provide stable and supportive environments, thereby affecting their children’s developmental outcomes (Hancock et al., 2013). Moreover, the communal effects of trauma can severely undermine social cohesion and stability, resulting in increased vulnerability to socio-economic challenges and perpetuating systemic inequalities.
The ramifications of this cycle extend beyond individual families, impacting entire communities and contributing to broader societal issues (Ijiga, et al., 2024). Addressing the cycle of trauma within families and communities is critical for promoting healing and resilience, particularly in populations at high risk for trauma exposure. Implementing trauma-informed care and support systems can help break these cycles, fostering recovery and improving the overall well-being of affected individuals and their families (Aboi, 2024). By prioritizing interventions that address the roots of trauma, communities can work towards healing and greater social stability.
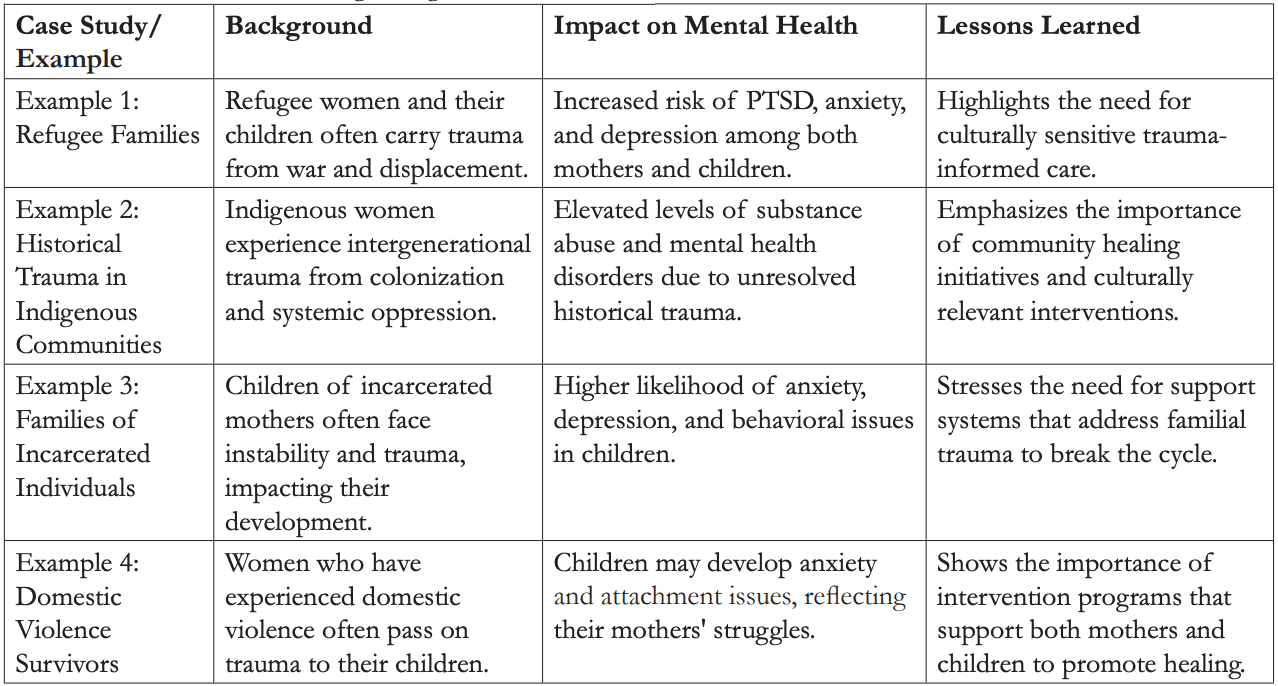
Case Studies or Examples Illustrating Intergenerational Trauma
Intergenerational trauma often manifests in communities affected by historical events, with profound implications for individuals and families. A prominent example is the Japanese American experience during World War II, where families who were forcibly relocated to internment camps experienced significant psychological distress that persisted across generations (Nagata, 2019) as presented in table 5. Research has shown that children of interned individuals often grapple with anxiety, depression, and a strong sense of identity conflict, reflecting the lasting effects of their parents’ trauma (Franco, 2022). Additionally, Native American populations have faced historical traumas through colonization, resulting in cyclical patterns of trauma that affect familial and community dynamics, leading to increased rates of substance use, mental health disorders, and violence within these communities (Franco, 2022). These examples underscore the critical need for trauma-informed care and interventions that acknowledge and address the pervasive impact of intergenerational trauma on mental health and well-being.
Table 5: Case Studies Illustrating Intergenerational Trauma
Neuropsychological Rehabilitation Approaches. Overview of Neuropsychological Rehabilitation and Its Importance for Incarcerated Women
Neuropsychological rehabilitation encompasses tailored interventions aimed at addressing cognitive and emotional deficits resulting from brain injuries, particularly TBI. This form of rehabilitation is essential for incarcerated women, who often confront unique challenges stemming from mental health issues, substance use disorders, and histories of trauma. Research indicates that a significant number of women in prison have encountered severe traumatic events, which can lead to cognitive impairments and emotional dysregulation (Karlsson & Zielinski, 2018) as represented in figure 7.
The primary objectives of neuropsychological rehabilitation include enhancing cognitive functioning, improving emotional regulation, and facilitating successful reintegration into society through targeted therapies and support systems (Chan, et al., 2023). Such interventions are designed to mitigate the adverse effects of trauma and TBI, ultimately reducing recidivism rates while promoting better mental health outcomes.
The importance of neuropsychological rehabilitation cannot be overstated; it addresses the complex interplay of cognitive, emotional, and behavioral challenges faced by this vulnerable population (Mansoor, et al., 2024). By providing comprehensive support that recognizes the multifaceted nature of their experiences, rehabilitation programs can empower incarcerated women to overcome barriers to their recovery and lead more fulfilling lives postincarceration (Ijiga, et al., 2024). This holistic approach is crucial for fostering resilience and improving overall wellbeing, enabling these women to break free from the cycles of trauma and criminality that often define their lives.
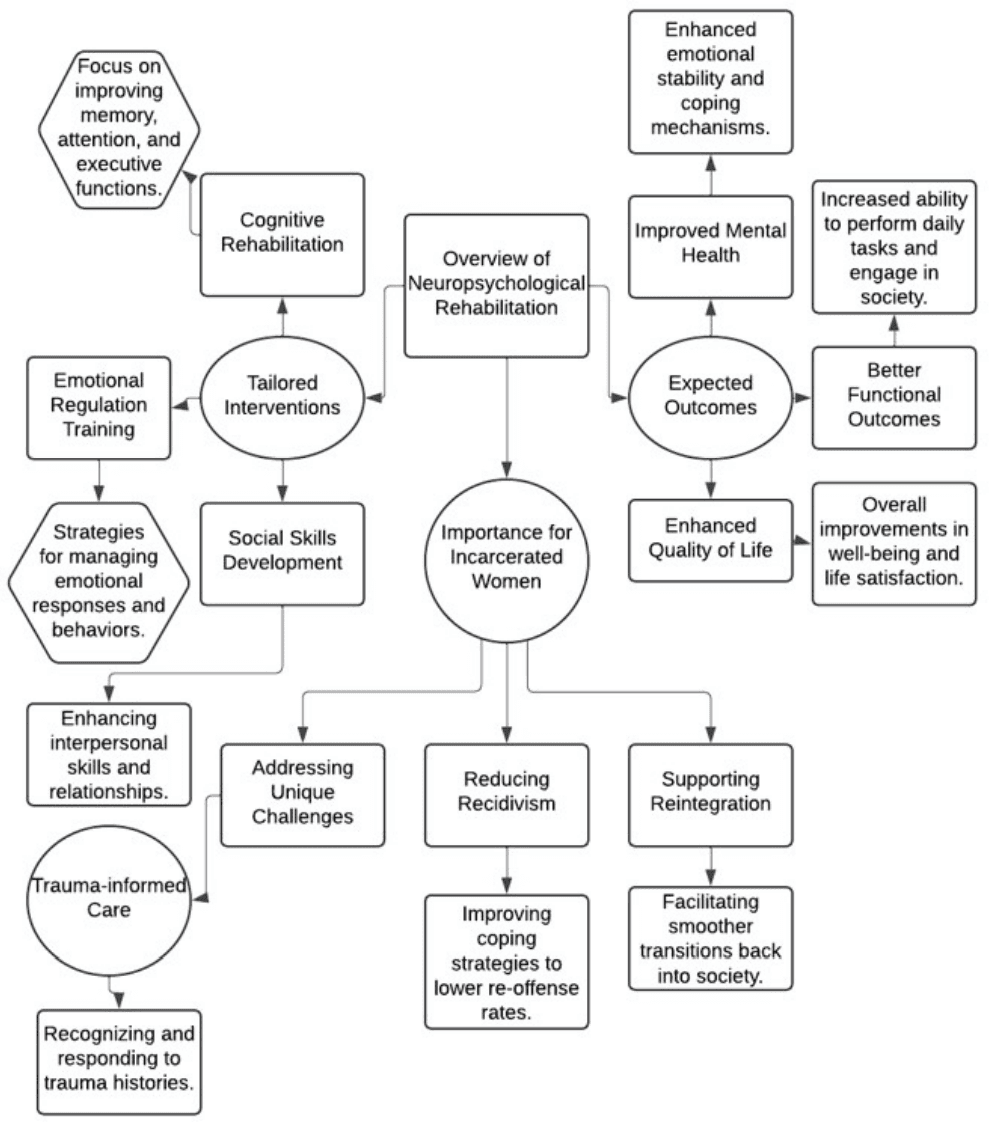
Figure 7:
Figure 7 visually encapsulates the critical components of neuropsychological rehabilitation and its significance for incarcerated women. At the center, it emphasizes the concept of tailored interventions, branching into specific areas such as cognitive rehabilitation, emotional regulation training, and social skills development. Each sub-branch highlights targeted strategies designed to address the unique cognitive and emotional challenges faced by incarcerated women, particularly those with trauma histories. The diagram further underscores the importance of neuropsychological rehabilitation in reducing recidivism, supporting reintegration, and addressing the specific needs of this population.
Additionally, it outlines the expected outcomes, including improved mental health, better functional capabilities, and enhanced overall quality of life. This comprehensive overview illustrates the necessity of integrated and individualized approaches in rehabilitation programs to foster recovery and resilience among incarcerated women.
Table 6: Evidence-Based Interventions Targeting TBI, Substance Use, and Mental Health Disorders
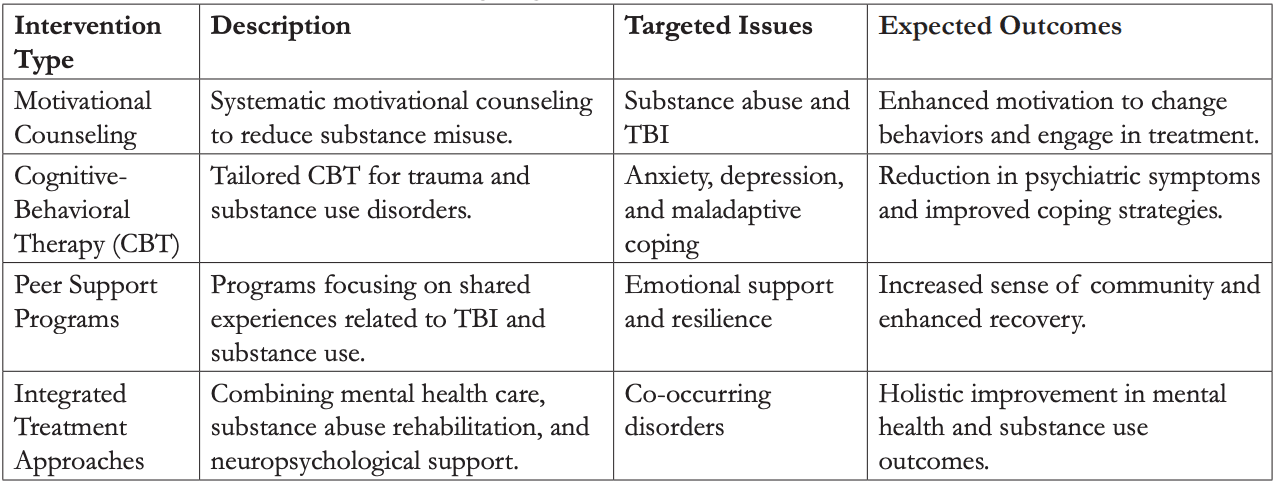
Evidence-Based Interventions Targeting TBI, Substance Use, and Mental Health Disorders
Evidence-based interventions that address the complexities of TBI, substance use, and mental health disorders are crucial for promoting recovery and improving outcomes, especially among incarcerated women. Integrated treatment approaches have demonstrated effectiveness in addressing co-occurring conditions. For example, systematic motivational counselling has proven beneficial in reducing substance misuse among individuals with TBI (Cox et al., 2003) as presented in table 6. This approach empowers individuals by enhancing their motivation to change behaviors, thereby facilitating better engagement with treatment.
Cognitive-behavioral therapies (CBT) tailored for trauma and substance use disorders have also shown efficacy in alleviating symptoms of anxiety and depression while promoting healthier coping mechanisms (Ebenibo, et al., 2024). These therapies address maladaptive thoughts and behaviors, equipping individuals with strategies to manage their emotional responses more effectively. Furthermore, peer support programs that emphasize shared experiences related to TBI and substance use have been effective in fostering resilience and recovery (Gonzaga, et al., 2024). These programs create supportive environments where individuals can share their challenges and successes, promoting a sense of community and belonging.
Collectively, these evidence-based interventions underscore the importance of a comprehensive approach that takes into account the unique challenges faced by individuals with TBI, mental health disorders, and substance use issues (Awotiwon, et al., 2024). Such integrated strategies are essential for facilitating successful rehabilitation and improving the overall quality of life for this vulnerable population.
Challenges and Barriers to Implementing Rehabilitation Programs in Correctional Facilities
Implementing rehabilitation programs in correctional facilities encounters significant challenges that hinder their overall effectiveness. One of the primary barriers is the limited availability of resources, including both funding and trained staff, which restricts the development and sustainability of comprehensive rehabilitation initiatives (Taxman, 2018). Many correctional institutions operate under tight budgets, leading to inadequate access to essential services such as mental health care, vocational training, and substance use treatment programs (Ijiga, et al., 2024). This lack of resources creates a significant gap in the support needed for incarcerated individuals seeking rehabilitation.
Additionally, the prevailing punitive culture within many correctional settings often undermines rehabilitation efforts. In these environments, security concerns may take precedence over therapeutic interventions, resulting in a lack of adequate support for inmates’ psychological and emotional needs (Taxman, 2018). This focus on punishment rather than rehabilitation can stifle the potential for meaningful change among inmates.
The stigma associated with mental health and substance use disorders also poses a barrier to engaging individuals in rehabilitation programs. Many incarcerated women may feel embarrassed or ashamed to seek help, which can deter them from participating in available programs (Ijiga, et al., 2024). These factors collectively contribute to the challenges in creating effective rehabilitation environments that promote successful re-entry into society. Addressing these barriers is critical for improving rehabilitation outcomes and facilitating the reintegration of individuals into their communities after incarceration. By focusing on enhancing resources, shifting cultural perceptions, and reducing stigma, correctional facilities can better support the rehabilitation of their populations.
CONCLUSION
This paper highlights the intricate relationships among TBI, substance use, and mental health disorders in incarcerated women. It reveals that a significant proportion of this population suffers from high rates of TBI, frequently associated with histories of violence and trauma. These experiences not only affect their physical health but also contribute to psychological distress, often leading to substance use as a common maladaptive coping mechanism. The reliance on substances exacerbates existing mental health issues, including depression and anxiety, creating a cycle that is difficult to break.
Moreover, the concept of intergenerational trauma emerges as a critical factor, illustrating how the effects of trauma can extend beyond individuals to impact families and communities. This perpetuation of trauma underscores the need for comprehensive interventions that address both individual and familial histories of trauma.
The findings also emphasize the importance of effective neuropsychological rehabilitation programs tailored to the specific needs of incarcerated women. However, significant barriers remain, including limited resources and the prevailing punitive culture within correctional facilities that often prioritizes security over rehabilitation. These obstacles hinder the implementation of effective treatment strategies.
Overall, the paper stresses the urgent need for integrated, trauma-informed interventions designed to address the unique challenges faced by incarcerated women. By focusing on their specific needs, these interventions can facilitate successful re-entry into society, ultimately improving their quality of life and reducing recidivism rates.
Recommendations
To enhance rehabilitation for incarcerated women, several key policy and practice recommendations arise from the findings of this study. First and foremost, correctional facilities should implement integrated, trauma-informed care models that specifically address the unique needs of women. This holistic approach should focus on the interplay between TBI, substance use, and mental health disorders, ensuring that all aspects of an individual’s well-being are considered during treatment.
Increased funding and resources are essential for developing comprehensive rehabilitation programs that include mental health services, vocational training, and substance use treatment. These programs should be designed to empower women, providing them with the tools and skills necessary for successful reintegration into society.
Additionally, training for correctional staff should emphasize the importance of understanding trauma and its effects on behavior, fostering a supportive environment that promotes recovery. Creating an environment where staff are equipped to recognize and address the psychological needs of inmates can significantly improve treatment outcomes.
Establishing partnerships with community organizations can facilitate the provision of post-release support, ensuring continuity of care as individuals transition back into society. Such collaborations can also help in building a supportive network for formerly incarcerated women. Finally, advocating for legislative reforms is crucial to eliminate barriers to accessing rehabilitation services. Promoting alternatives to incarceration for individuals with complex needs can further enhance successful reintegration efforts. By focusing on these recommendations, correctional facilities can create a more effective rehabilitation system that addresses the multifaceted challenges faced by incarcerated women.
Future Research Directions in Addressing the Intersection of TBI, Substance Use, and Mental Health in This Population
Future research should concentrate on several pivotal areas to deepen the understanding of the intersection between TBI, substance use, and mental health disorders in incarcerated women. First, longitudinal studies are essential to track the long-term effects of TBI on mental health and substance use, as they can provide valuable insights into the evolving challenges faced by this demographic over time. By following individuals across different stages of their lives, researchers can identify patterns and risk factors that contribute to ongoing issues.
Additionally, investigations into the effectiveness of integrated treatment programs are crucial. These programs should combine mental health care, substance use rehabilitation, and neuropsychological support, specifically tailored to meet the unique needs of women. Understanding how these comprehensive approaches can improve outcomes will be vital for informing future interventions.
Exploring the role of community-based interventions post-incarceration will also be critical for facilitating successful reintegration. Research should examine how support systems, resources, and peer networks can enhance recovery and reduce recidivism rates among women transitioning back into society.
Finally, studies should focus on the systemic barriers affecting the implementation of rehabilitation programs, such as funding limitations and staffing shortages. Analyzing these obstacles will provide insights necessary for advocating policy changes aimed at enhancing support for incarcerated women. Addressing these research areas will be essential in developing effective strategies to improve the lives of women facing the compounded challenges of TBI, substance use, and mental health disorders.