Abstract
Background Substance use disorders are associated with severe negative social and health-related outcomes. Evidence has accumulated that long-term substance use is associated with alterations in social interaction behavior, which likely contributes to the vicious cycle of substance use disorder. However, little is known about whether these social problems originate from contextual factors only or also from the substance use itself—in other words, if they are predisposed or substance induced. Methods We studied the causation behind behavioral alterations of substance users over a 9-year period (ages 11–20 years) in an urban age cohort (N = 1002) with a high prevalence of substance use at age 20. We identified common substance use patterns using toxicological hair analysis, examined behavioral alterations with incentivized games, and used teacher assessments across different ages to determine the causes and effects that underlie substance use–related impairments in social interaction. Results We found that opioid and stimulant users showed reduced prosocial behavior compared with nonusers, particularly in interpersonal trust and perspective taking (e.g., they were approximately 50% less likely to trust others). Our longitudinal analyses suggest a causal relationship between the nonmedical use of prescription opioids and impaired social behavior, whereas impairments among stimulant users seem to be partially predisposed. Moreover, women tended to be more severely affected by opioid use than men. However, no behavioral alterations were found among young adult cannabis or ecstasy users. Conclusions Highly addictive substances such as opioids can impair users’ social behavior by undermining fundamental human interaction, thereby fueling a vicious cycle of substance use and social isolation.
Problematic substance use is a global public health issue with far-reaching social implications (1). Beyond the increased morbidity and mortality of individuals with substance use disorders (SUDs), those affected often experience a variety of mental and social issues such as reduced well-being, depressive disorders, anxiety disorders, increased chances of job loss, and disrupted relationships (2, 3, 4). It has been proposed that many of these social problems, which can sustain and exacerbate the addictive use, are induced by substance-driven impairments in social cognition and behavior that augments the risks of social isolation, depression, and aggression and thus contribute to the vicious cycle of addiction (5, 6, 7). Consequently, interpersonal impairments may further increase substance use and relapse vulnerability, thereby making long-term substance use a global social problem.
This is supported by several clinical studies that have shown impairments in diverse social cognitive skills—ranging from empathy to mental perspective taking—specifically among long-term stimulant and opioid users (8, 9, 10, 11). For example, patients with heroin dependence showed increased self-serving behavior and altered fairness as well as inequity tolerance in social interactions depending on contextual factors (12). Similarly, individuals with alcohol use disorders (13), nonmedical methylphenidate (14), methamphetamine (15), and both recreational and dependent cocaine use (8) showed less prosocial and more self-serving behavior than substance-naïve control participants. Additionally, neuroimaging studies suggest a relationship between substance use and altered brain activity in areas involved in social cognition and social decision making (16, 17, 18, 19), and cocaine users who reduced their consumption over a 1-year period showed improvement in prosocial behavior and empathy (11). Taken together, these descriptive findings indicate a link between altered social decision making and the repeated use of specific substances.
Despite the recent progress in revealing the association between interpersonal impairments and substance use, little is known about their origin. The abovementioned studies focused primarily on highly selected and relatively small clinical samples of middle-aged substance users and compared users with conveniently approachable nonusers who were often similar on only a few characteristics such as age, sex, or intelligence. Thus, it is unknown whether the impairments originate from substance use, represent risk factors for substance use, or result from other factors related to prolonged or addictive substance use. Thus, the causation behind substance users’ interpersonal impairments not only remains untested but also needs to be validated with comparable nonusers.
Moreover, for most illegal substances, our knowledge from the studies available are limited by 3 additional reasons. First, previous studies focused primarily on altruism and fairness, neglecting other essential aspects of social decision making related to substance users’ social isolation and marginalization, such as interpersonal trust, cooperativeness, and honesty. Second, previous studies mostly considered one or only a few substances, leaving other substances unconsidered despite frequent co- and polysubstance use. Third, a substantial proportion of the available studies relied on participants’ self-reports regarding their substance consumption, which are known to be associated with underreporting biases, specifically in research settings (20,21). Even more surprisingly, to date, social decision making has not been systematically studied among cannabis users, non–medical prescription opioid users, and polysubstance users (22,23); although cannabis is the most commonly used illegal substance worldwide, nonmedical use of prescription opioids is currently more prevalent than heroin use, and polysubstance use is becoming increasingly common (24). Consequently, little is still known about the cause-and-effect relationship behind substance use–related alterations in social decision making; aspects involving interpersonal trust and honesty; how specifically cannabis, prescription opioids, and polysubstance use affect social cognition; and whether these impairments are already present among young and recreational users.
Unlike previous studies, we studied substance use–related impairments in social decision making and the underlying causation in a cohort of young mostly nondependent users and their former classmates in a longitudinal setting. This allowed us to assess whether users were predisposed to these possible alterations or whether the alterations were substance induced while excluding other contextual factors related to prolonged and addictive substance use. We conducted a large-scale longitudinal field study in which we evaluated the social behavior and substance use behavior of 1002 individuals who were >14 years of age using forensic hair toxicological analyses and decision-making experiments in combination with external assessments of social behavior. All participants entered the same randomly selected schools in the same city in the same year, representing approximately half of the entire age cohort in this area at this time. This allowed us to compare highly similar individuals raised in the same environments and schools at a young age when other factors related to severe substance use such as marginalization, unemployment, or severe health impairments play a subordinate role. To our knowledge, this study also provides the first comprehensive overview of substance use–related behavioral alterations in fundamental aspects of social interactions using a wide range of established and incentivized economic games (25). That is, we assessed individuals’ ability to give and return trust, as well as trust expectations in the trust game, altruism and fairness concerns in the dictator and ultimatum game, cooperation in the public goods game, and honesty in the dice game. In combination with teacher assessments of individuals’ social behavior and results from toxicological hair analysis, we minimized the risks of social desirability bias and tested whether impairments were related to the intensity of recent use in an exposure-response relationship. Moreover, additional self-reported information on potential confounders was collected from participants and their parents, such as information on substance use, including alcohol and nicotine use, attention-deficit/hyperactivity disorder, depression, anxiety symptoms, personality traits, parent-child relationships, delinquency, attitudes toward crime, and victimization. More in-depth information regarding our measures can be found in the Methods and Materials and in the Supplement.
Methods and Materials
A total of 1002 young adults (50.2% female, age ∼20 years) were sampled from the z-proso cohort (26). The cohort originates from a cluster-stratified randomized experiment at 56 randomly selected public primary schools in Zürich, Switzerland’s largest city. Initial assessment took place in 2004 with 1360 individuals (at age 7) representative of all public school first-graders in Zürich. An additional 7 observations were carried out at ages 8, 9, 11, 13, 15, 17, and 20 years. The data analyzed for this article were primarily collected between ages 11 and 20 years. Hair sampling and decision-making games were carried out at the Decision Science Laboratory at the ETH Zürich at age 20. All procedures were approved by the responsible local ethics committees (Nos. 2017-02021 and 2018.2.12), and the authors assert that all procedures complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975 as revised in 2008. Written informed consent was obtained from all participants.
Social decision making was measured by 5 established economic games in which participants could earn money depending on their choices and the choices of their randomly determined interaction partners. Respondents participated in a dice, trust, public goods, dictator, and ultimatum game (in order of appearance). More information can be found in Supplemental Methods.
Substance use was measured based on hair toxicological analysis using liquid chromatography–tandem mass spectrometry. A proximal hair sample of 3 cm was taken from the occiput, representing the consumption behavior over the past 3 months. Body hair was sampled if the participants’ scalp hair was not sufficiently long (n = 87). We applied latent profile analysis to stratify participants who tested positive for cannabinoids, MDMA, stimulants, or opioids into independent groups according to their hair concentration of these substances. Nineteen participants were excluded before latent profile analysis and complete analysis because they only tested positive for other substances (e.g., benzodiazepines or Z-drugs). Participants who tested negative for all the above substances were assigned to the abstinent (control) group. See Supplemental Methods for more details, including Table S11, for all tested substances.
Additional covariates measured using questionnaires included self-reported of legal and illegal substance use, including incidence over the past 3 and 12 months and age of first use. We also used the Social Behavior Questionnaire (27) and measured attention-deficit/hyperactivity disorder, depression, anxiety symptoms, personality traits, parent-child relationships, delinquency, attitudes toward crime, and victimization scales. More in-depth information regarding our measures can be found in the Supplement.
To analyze the behavioral alterations in social decision making (in comparison to nonusers), we used a 2-stage procedure for each aspect of social decision making and a composite score. First, to determine differences in social behavior between nonusers and different user groups, a regression analysis was conducted in which individuals’ substance use group memberships (with the cohorts’ negative-tested participants as a control and reference group) and a series of covariates were included in the model. Second, for the user groups that revealed alterations of specific social behaviors, a dose-response relationship analysis was conducted to determine whether the substances’ hair concentration (intensity of recent use) in the user group was associated with the magnitude of altered behavior. The composite prosociality score was derived from the standardized average of all standardized behaviors in the decision-making games. Standardization was conducted by demeaning and normalizing based on nonusers’ behavior. Additional covariates measured using questionnaires including self-reported legal substance use prevalence, attention-deficit/hyperactivity disorder, depression, and anxiety scales were included in the regression analyses, and all tests were 2 sided with an alpha level of 0.05.
To determine whether users were predisposed to prosocial impairments, we used a 2-stage procedure. First, we used self-reported substance use data to determine participants’ first contact with the substances. At age 11, only 3 individuals reported having used any relevant substances (excluded from the analyses). Second, for each substance use profile, we compared z-standardized composite scores of students’ prosocial behavior assessed at age 11 by teachers with those of later nonusers to identify pronounced predisposed prosocial impairments. Composite scores were derived from teachers’ 7 z-standardized 5-point scale items (e.g., “the child volunteers to help others” or “shares things with others”). More in-depth information can be found in the Supplement (including explicit wording).
To estimate the effect of substance use on prosocial behavior, we used a propensity score matching procedure with Mahalanobis calipers. Based on 42 covariates that captured sociodemographic characteristics, self- and external evaluation of social behaviors, personality traits, parent-child relationships, delinquency, attitudes toward crime, and victimization, we estimated the likelihood of becoming a user based on pre-exposure characteristics at age 11 (or 13 if applicable). Due to the large number of covariates, missing values were imputed for the matching. Imputed values were mainly parent characteristics, which corresponded to approximately 0.3% of the matching data. Sixty-five individuals with more than 20% missing values were excluded from the analysis. Subsequently, users were matched on a one-to-one basis within a caliper width of 0.2 SD of the propensity scores to comparable nonusers. We achieved a balance of covariates by using an iterative Mahalanobis procedure, which is more fully described in the Supplement together with more information concerning the matching and used covariates. The standardized composite prosociality scores of users and their unique matched partners were compared at ages 11 (teacher assessment) and 20 (games) for each use profile using a 2-sided t test.
Results
We used hair testing to determine the extent of substance use among our cohort of 20 year olds. Figure 1 shows the results of the toxicological analysis of 1002 hair samples. Two-thirds of participants tested negative for all measured substances (n = 664). Of those 338 participants who tested positive for at least 1 substance (Figure 1B), 122 (36.1%) tested positive for multiple substances (Figure 1C)1. A latent profile analysis classified substance users by their intensity of single and polysubstance use into 5 user groups, namely those who mainly use cannabis (n = 85), nonmedical prescription opioids (n = 83), MDMA or ecstasy (n = 65), or illegal stimulants (n = 29, predominantly cocaine), and those who displayed intense use of multiple (poly-)substances (n = 57; mainly stimulants in combination with cannabis, MDMA, and to a lesser extent opioids)(Figure 1D).
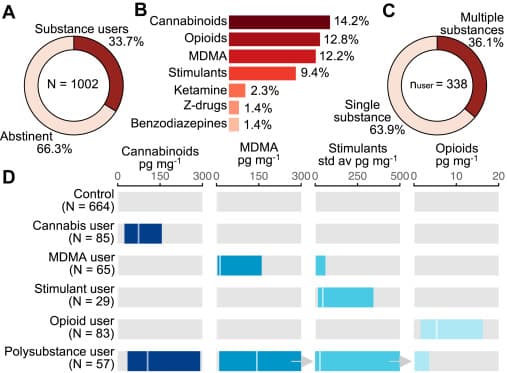
Figure 1. Cohorts’ substance use patterns according to hair toxicological analysis. (A) Proportion of substance users and abstinent participants disregarding alcohol and tobacco use. (B) Three-month prevalence per substance class in the full sample. (C) Relative proportion of participants who tested positive for only one or for multiple substances. (D) Distribution of substance hair concentration for the nonusing control participants and 5 different substance use patterns identified using latent profile analyses. Values shown are the 20th and 80th percentiles along with the median hair concentration (white horizontal line).
Did Young Substance Users Show Alterations in Prosocial Decision Making?
We proceeded by comparing the behaviors of nonusers with the different user groups in the decision-making experiments at age 20. To compare the overall prosociality of users with that of nonusers, we unified the 5 decision-making games in a z-standardized composite score of prosociality, thereby capturing different aspects of human prosocial behavior (i.e., honesty, trust, trustworthiness, cooperation, fairness). Figure 2 shows the composite prosociality score for the identified user groups and the relative differences in the individual decision-making games between users and nonusers. We found that individuals of the opioid and stimulant use profiles revealed a composite prosociality score that was reduced by approximately 0.35 SDs compared with nonusers (opioid users: standardized regression coefficient b = −0.31, t971 = −2.71, p = .007; stimulant users: b = −0.41, t971 = −2.17, p = .030) (also see Figure 2A and Table S1). Subsequently, we also tested whether the intensity of opioids and stimulant use was linked to the severity of impairments. No association between use intensity (measured by substance hair concentrations) and altered composite prosociality scores was found in the respective substance use profiles (Table S3).
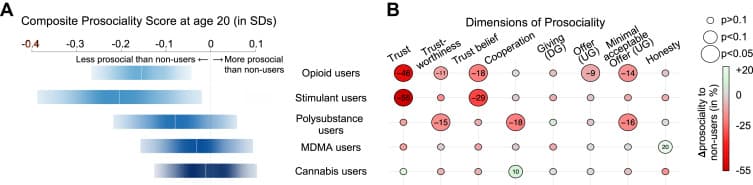
Figure 2. Overview of the association between young users’ substance use and altered social decision making. (A) Point estimates of the prosociality difference between user groups and nonusing control participants measured in standard deviations of the composite prosociality scores of nonusing control participants (vertical white lines) along with the 95% CI (blue bars). (B) Comprehensive summary of the association between substance use and alterations in social decision making. Circle sizes indicate the size of the significant differences between user groups and nonusing control participants. Alterations are colored from dark red (less prosocial) to medium gray (similar prosocial) to light green (more prosocial) depending on the relative effect size of the difference between user groups and the nonusing control group from the same cohort. Supporting numbers of the relative difference between users and nonusers are provided for behaviors with effects p > .1. The full regression tables can be found in the Supplement. DG, dice game; UG, ultimatum game.
Additionally, to assess different facets of prosocial deficits for the different substance use profiles, we compared participants’ decision making in the different games in nonusers and participants with different substance use profiles at age 20. Individuals from the MDMA and cannabis use profiles revealed no impairments, whereas individuals from the opioid, stimulant, and polysubstance use profiles revealed pronounced differences in aspects of social decision making, which are highlighted in the sections below (also see Figure 2B and Table S1). Regarding the composite prosociality score, we did not find a dose-response relationship between recent substance use intensity (hair concentration) and the magnitude of the impairment among individuals from the same user profile (Tables S2 and S3).
Opioid Use
We found that participants who predominantly used prescription opioids without medical indication were approximately 46% less likely to trust other individuals when real money was at risk [log(odds) = −0.61, odds ratio = 0.54, t965 = −2.53, p = .011] and had around 18% diminished beliefs about others’ trustworthiness compared with nonusers (b = −11.25, t963 = −2.23, p = .026). As a trustee in the trust game, opioid users tended to return around 11% less money to trusting partners than nonusers, pointing to reduced trustworthiness and a propensity for positive reciprocity (b = −9.16, t962 = −1.94, p = .053). While offers of individuals from the opioid use profile and nonusers were indistinguishable in the dictator game giving, opioid users offered 9% lower shares in the ultimatum game (b = −6.49, t961 = −2.19, p = .029), indicating that the groups processed the risk of being rejected by an interaction partner differently. At the same time, opioid users were more likely to reject unfavorable offers as their minimum acceptable offer because the recipient in the ultimatum game was 14% higher than nonusers (b = 7.76, t971 = 2.47, p = .014). Thus, they gave less as proposers in the ultimatum game but at the same time expected to receive more as recipients, which can indicate hypocritical tendencies and deficits in perspective taking, which is consistent with previous observations (10,29).
Stimulant Use
The individuals classified into the predominantly stimulant-using profile were approximately 55% less likely to trust other individuals when real money was at risk [log(odds) = −0.79, odds ratio = 0.45, t965 = −2.01, p = .044] and had diminished beliefs about others’ trustworthiness compared with nonusers (b = −18.31, t963 = −2.22, p = .026).
Polysubstance Use
Although polysubstance users did not reveal overall reduced prosociality, they showed pronounced differences in individual dimensions of social decision making. As a trustee in the trust game, polysubstance users tended to return less money to trusting partners, indicating reduced trustworthiness and a propensity for positive reciprocity (b = −12.44, t962 = −2.13, p = .033), which translated to a 15% reduction compared with the nonusers. Regarding cooperation behavior, contributions to the public good were negatively associated with polysubstance use, reducing contributions to the public good by 18% compared with the nonusers (b = −5.94, t958 = −2.51, p = .012). The level of the minimum acceptable offer in the ultimatum game was 16% higher in polysubstance users than in nonusers, indicating stronger sensitivity to unfairness and a preference for negative reciprocity (b = 9.22, t971 = 2.38, p = .017).
Was the Reduced Prosociality Observed in Opioid and Stimulant Users Predisposed or Caused by the Use?
To test for predisposed impairments in prosociality, we compared the prosocial behaviors of users and nonusers before first use at age 11.2 At this time, teachers evaluated students’ prosocial behavior based on seven 5-point Likert scale items (e.g., “the child volunteers to help others” or “shares things with others”). The resulting standardized prosociality scores at age 11 revealed that later users showed no systematical differences from nonusers (−0.1 to 0.08 SD differences, all p > .52) except for later intense polysubstance users; teachers rated their prosociality as being significantly lower than that of later nonusers (−0.43 SD, t515 = 2.72, p = .010). This indicates that reduced prosociality (and related factors) during childhood may constitute a risk factor for later intense polysubstance use.
The use of substances may also be tied causally to impairments in prosociality. Because experimental studies are unfeasible, we used quasi-experimental matching methods to compare the development of users and nonusers who shared similar characteristics and risks of becoming a user during early adolescence. Similarity was assessed based on 42 pre–substance use covariates measuring sociodemographic characteristics, self- and external evaluation of social behaviors, personality traits, parent-child relationships, delinquency, attitudes toward crime, and victimization at ages 11 or 13 years, if applicable. See Methods and Materials for additional information about matching. Comparable user-nonuser pairs were found for 267 individuals of the substance use profiles; 25 high-risk individuals and 27 further individuals from the substance use profiles could not be matched due to a lack of comparable nonusers or (excessive) missing information, respectively. Unmatched users also demonstrated significantly lower prosociality than nonusers and matched users at age 11. A full table of the achieved balance and detailed results can be found in Tables S4 and S5. Although the matched individuals from the specific substance use profiles and control participants showed similar levels of prosociality (among other characteristics) during pre–substance use in early adolescence, individuals of the opioid use profile revealed significantly lower levels of prosociality at age 20 than their matched control participants (Figure 3). In contrast, the individuals from the stimulants, polysubstance, MDMA, and cannabis use profiles revealed no differences in composite prosociality scores from those of their matched control participants at age 20, although the stimulant profiles revealed a similar decline in prosociality as the opioid profile. This may indicate a causal relationship between the use of prescription opioids and impairments in prosociality.
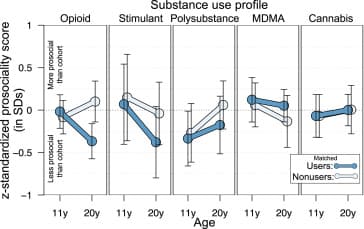
Figure 3. Development of prosocial decision making in association with substance use. Shown are the development of prosociality scores between ages 11 and 20 years for individuals of the substance use profiles (dark blue) and corresponding highly similar individuals—based on Mahalanobis propensity score matching of 42 covariates—without proven substance use (light blue, slight right shifted). Prosociality scores were z-standardized at the cohort level, i.e., horizontal line at 0 indicates the population average for each observational point. The data shown represent only matched individuals of the substance use profiles; 26 high-risk individuals and 27 individuals with missing information could not be matched. Vertical lines indicate the 95% CI.
To further assess the potential causal effect of substance use on social behavior, we conducted a series of additional analyses on the temporal relationship between substance use and altered social behavior. However, unlike the previous analyses, these analyses were not based exclusively on external evaluations and should be viewed with caution because self-reported substance use tends to be less reliable in the research setting (20,21). For example, about half of the hair sample–identified individuals in the stimulant profile never reported having taken any stimulants, and some individuals reported varying ages of first use during different observations (Table S7).
Were Changes in Social Behaviors Temporally Tied to Changes in Substance Use?
Based on the self-reported substance use data and the evaluations of social behavior by teachers, we conducted a first-difference estimation in which we regressed individual change in substance use on change in social behavior evaluated by teachers. Results showed that increases in self-reported opioid and stimulant use (from “never used before” to “recreational use” to “frequent use,” i.e., more than 51 times per year) between 2 observational points were usually associated with decreases in measured prosocial behavior. However, the effects were not significant or were only marginally significant (opioids: −0.85 SD, p = .26; stimulants: −0.26 SD, p = .12; MDMA: 0.11 SD, p = .50; cannabis: −0.01 SD, p = .46). Further ex-post analyses in which we analyzed men and women separately revealed that especially among women, changes in self-reported opioid use were associated with a reduction in teacher-rated social behavior (opioids: −2.4 SD, p = .02; stimulants: −0.38 SD, p = .17; MDMA: 0.46 SD, p = .07; cannabis: −0.04 SD, p = .14). This was not true for men (all p > .4). However, it should be emphasized that these analyses are based on underreported self-reported substance use and, in some cases, on only a few cases. Nonetheless, the findings suggest a possible differential effect of substances, especially opioids, on the prosocial behavior of young men and women. For more information, see Tables S8 to S10.
In summary, we found that young prescription opioid and stimulant users showed behavioral impairments in social decision making, especially in situations related to trust or perspective taking. We found no pronounced impairments among young MDMA- or cannabis-using individuals. Intense polysubstance users revealed reduced prosociality in early adolescent social behavior (ages 11–13), which may constitute a risk factor for later use. The use of opioids impaired the development of prosocial behavior, and the use of stimulants possibly did also. Moreover, we found suggestive evidence that opioid use affects the social behavior of men and women differently, i.e., increased opioid use affected the social behavior of women more negatively than that of men.
Discussion
Substance use is a significant public health concern with far-reaching costs (30), but its impact on interpersonal decision making and relationships often goes unnoticed. Its influence during adolescence is particularly concerning because it can set the stage for later SUDs (31). Understanding the causes and effects of substance use during adolescence is a highly relevant but ethically challenging objective. In contrast to previous work, we did not preselect individuals based on use history and intensity criteria. Instead, we sampled 1002 participants from a near-representative community cohort study of 20 year olds (initially sampled at age 7). We conducted large-scale hair toxicological analyses together with incentivized social decision-making experiments and behavioral assessments done by previous teachers. With this, the work makes 4 critical contributions to our understanding of early substance use and its close connection to social decision-making skills.
First, our research underscores the relationship between 20-year-olds’ use of highly addictive substance (i.e., opioids and stimulants) and impaired social decision-making skills, particularly in the areas of interpersonal trust and perspective taking. While our findings with opioid users are consistent with previous nonbehavioral (10,29,32,33) and behavioral (12) evidence, we did not find the pronounced self-serving behavior among our young stimulant users found in previous research (8,11,15). This may indicate that selfish tendencies may emerge after prolonged intensified or combined substance use, which is partially supported by our finding on intense polysubstance users, who tend to reveal selfish tendencies in cooperation and trust situations (Figure 2B). The absence of a dose-response relationship between substance use intensity and impairment severity may also result from attempts at self-medication (34) or other contextual factors, such as peer influences (35). Moreover, substance hair concentrations have some limitations in determining the precise frequency, context, or pattern of use, which is specifically true in the context of cannabis use (28,36,37).
Second, we found that young MDMA and cannabis users showed no pronounced deficits in social decision making. Our results do not provide evidence supporting increased prosocial behavior among MDMA users (38) or reduced prosociality among cannabis users (39). Context (rural vs. urban population), measurement methods (self-reported vs. revealed behavior), and limited co-use analyses may partially explain the difference from these previous findings. We conclude that regular cannabis or recreational MDMA use is not associated with severe deficits in social decision making, at least during young adulthood in urban areas.
Third, we found that childhood deficits in prosocial behavior may increase the risk of later intense polysubstance use. While a previous study linked prosocial deficits in children from rural areas to later cannabis use (39), our urban sample did not confirm this for pure cannabis users. We also did not identify any single-substance user groups with predisposed prosocial deficits during early adolescence, as was suggested for cocaine users (8). Instead, our findings indicate that childhood deficits were only evident among later intense polysubstance users, characterized by combined and intense stimulant, cannabis, and MDMA use. This is consistent with both results mentioned, considering that they did not measure (39) or excluded (8) co-use of the other substances, which underscores the importance of comprehensive toxicological analyses.
Fourth, our longitudinal findings indicate a causal relationship between prescription opioid use and behavioral impairment in social decision making. While opioid users’ behaviors in the dictator game were similar to those of control participants, they offered significantly less in the ultimatum game, suggesting altered risk assessment. Opioid users also tended to reject unfavorable outcomes more frequently, creating a paradox of giving less and expecting more from their partners in these social interactions. This supports previous observations of impaired perspective-taking skills among opioid users (10,29). Exogenous opiates and opioids such as morphine, heroin, oxycodone, and fentanyl relieve pain but disrupt social behavior through neural pathways that overlap with social-emotional functioning (40,41). Substance use activates reward circuits that involve endogenous opioids and dopamine. Therefore, synthetic opioids can lead to tolerance and maladaptive learning. At the same time, social stressors such as losing social connections can trigger relapses, leading to a vicious cycle of opioid use (7).
Additionally, further ex-post analyses suggest that opioid use affected the social behavior of men and women differently, with opioid use having a more adverse effect on women. While this finding is based on self-report data, which has moderate reliability (20,21), it indicates that opioid use may affect women’s prosocial behavior differently compared with men, which warrants further investigation.
Although our study has several advantages over previous studies by utilizing and combining different revealed measures of substance use and social decision making in a representative cohort of ages 14 to 20 years, it is not without limitations. While the uniform local context of our cohort facilitated more suitable comparisons between the trajectories of users and nonusers, it limits the generalizability of our findings to other cultural and geographical contexts. Even though the attrition rate of our cohort was comparatively low, we found that not participating in the cohort was related to slightly lower prosociality scores but not to substance use, which nevertheless could have biased our results (see the Supplement). While hair analyses offer several advantages over urine or blood tests specifically in measuring cumulative exposure, they also have some limitations in capturing dynamic changes in substance use intensity, which may explain the absence of a dose-response relationship. Nevertheless, they can effectively mitigate known issues of social desirability bias associated with self-reported substance use (42).