Abstract
Background: Alcohol and cannabis use rates are highest in college-aged young adults, and both alcohol and cannabis use are independently related to high-risk sexual behaviors (HRSBs). HRSBs (e.g., sex without protection against sexually transmitted infections) are a prevalent public health problem in college students, with little research examining simultaneous alcohol and cannabis use (i.e., using both alcohol and cannabis at the same time so the effects overlap) and HRSBs.
Method: We examined simultaneous alcohol and cannabis-related HRSB frequency, gender differences in simultaneous alcohol and cannabis-related HRSBs, and differences in HRSBs between simultaneous and non-simultaneous users. Alcohol and cannabis using college students (N = 534; Average Age = 19; 66.9% reported identifying as female) were recruited through a psychology department's human subjects research pool and completed a one-time, online, self-report survey.
Results: One-third of participants engaged in simultaneous alcohol and cannabis use prior to sexual intercourse in the past 3 months. Additionally, over one-third of participants reported heavy drinking (4/5 or more drinks for women/men) simultaneously with cannabis use prior to sexual intercourse in the past 3 months. Simultaneous alcohol and cannabis use was significantly and positively related to sexual intercourse after simultaneous use and after heavy drinking simultaneously with cannabis use. Past year simultaneous alcohol and cannabis users, relative to non-simultaneous users, reported increased incidents of sex without protection against sexually transmitted infections. No gender differences in simultaneous alcohol and cannabis-related HRSBs were found.
Conclusions: Future research should continue examining simultaneous alcohol and cannabis use and HRSBs.
High-risk sexual behaviors (HRSBs) are often defined as behaviors that increase one's chance for contracting a sexually transmitted infection (STI) or an unwanted pregnancy (Deckman & DeWall, 2011). These behaviors, which can include sex without protection against pregnancy or sexually transmitted infections (STIs), sex with multiple partners, or sex after substance use, are prevalent public health problems associated with a myriad of negative outcomes in college students (Metrik et al., 2016; Simons et al., 2010). Indeed, negative outcomes related to HRSBs include contraction of STIs and unwanted pregnancies (Cooper, 2002). The treatment of STIs is costly, totaling approximately $15.6 billion in the United States per year (Owusu-Edusei et al., 2013). In a recent study of college students, nearly 9% reported having four or more sexual partners in the past 12 months, nearly half reported not using a contraceptive method the last time they had vaginal intercourse, and 70% reported using alcohol and/or drugs prior to or during sexual activity (American College Health Association, 2017; Scott-Sheldon et al., 2010).
Further, rates of cannabis and alcohol use are high in college students. Cannabis is a commonly used drug on college campuses, with 42% of students reporting past-year cannabis use (Schulenberg et al., 2019). Additionally, the majority of college students (78%) report alcohol use in the past year, with 33% engaging in a heavy drinking episode (5/4 or more drinks in a row for men/women) in the past two weeks (Schulenberg et al., 2019). Further, simultaneous alcohol and cannabis use (i.e., using both alcohol and cannabis at the same time so the effects overlap) is common in college students, with nearly 75% reporting at least one occasion of simultaneous alcohol and cannabis use in the past year (White et al., 2019). Despite the high rates of HRSBs, alcohol use, and cannabis use in college students, there is a lack of research examining the relationship between simultaneous alcohol and cannabis use and HRSBs. The increasing legalization of cannabis combined with the prevalence of simultaneous alcohol and cannabis use and HRSBs in college students indicate a need to investigate this relationship to inform HRSB prevention and interventions.
Alcohol and Cannabis Use and HRSBs
Research has demonstrated a strong link between alcohol use and HRSBs. Among college students, 50% engage in alcohol use prior to sexual activity with a new partner, and 32% report drinking alcohol prior to unprotected vaginal intercourse (Brown & Vanable, 2007). Further, alcohol use is related to unprotected vaginal sex with a non-steady partner (e.g., a casual acquaintance) in college students (Brown & Vanable, 2007), and heavy alcohol use among college women is related to less condom use with steady partners (Scott-Sheldon et al., 2010). Further, a meta-analysis in college students found that an increase in blood alcohol concentration (BAC) of 0.1 mg/ml equated to an increased likelihood of 5% of having unprotected sex, indicating that increased alcohol consumption within a drinking period is related to increased intentions to have high-risk sex (Rehm et al., 2012).
The relationship between cannabis use and HRSBs is less clear. For example, cannabis use is associated with increased odds of having sexual intercourse, reduced condom use with casual partners, and a decreased likelihood of discussing sexual risk before sexual engagement in both young adults and adolescents (Anderson & Stein, 2011; Kingree & Betz, 2003; Metrik et al., 2016). Yet, other studies have found no relationship between cannabis use and HRSBs. For instance, a study using retrospective interview methods found that cannabis use was not associated with increased odds of unprotected sex with a casual partner (Metrik et al., 2016). Overall, the findings on the relationship between cannabis and HRSBs are mixed, with future research necessary to continue investigating this relationship.
Simultaneous Alcohol and Cannabis Use and HRSBs
Individuals who use both alcohol and cannabis are two times more likely to use them simultaneously (i.e., at the same time, so the effects of each substance overlap) rather than concurrently (i.e., using both alcohol and cannabis, but not necessarily at the same time), with almost half of cannabis-using college students and young adults reporting using alcohol simultaneously (Haas et al., 2015; Subbaraman & Kerr, 2015). Additionally, simultaneous alcohol and cannabis use is associated with a myriad of negative outcomes (e.g., increased alcohol use, social consequences) and increases the risk for these outcomes beyond either alcohol or cannabis use alone (Subbaraman & Kerr, 2015; Yurasek et al., 2017).
Yet, few studies have investigated the relationship between simultaneous alcohol and cannabis use and HRSBs, and those that have found mixed results. For instance, a cross-sectional study determined that BAC levels and frequency of cannabis use were independently related to increased risk of engaging in HRSBs, but did not interact to predict HRSBs (Simons et al., 2010). Further, a study using retrospective interviews in young adult women did not find a relationship between simultaneous alcohol and cannabis use and HRSBs (Anderson & Stein, 2011). A different retrospective interview study in young adults found that engaging in both heavy alcohol use and cannabis use increased the odds of engaging in unprotected sex with an established partner, but each substance did not independently increase odds for unprotected sex with an established partner (Metrik et al., 2016). Overall, there is a lack of research examining these constructs, and the existing research demonstrates an unclear relationship between simultaneous alcohol and cannabis use and HRSBs. Thus, additional research is necessary to examine the relationship between simultaneous alcohol and cannabis use and HRSBs.
Additionally, previous research has demonstrated that people who identify as men are more likely to engage in HRSBs (MacDonald et al., 2000; Nolen-Hoeksema, 2004) and have higher rates of simultaneous alcohol and cannabis (Brière et al., 2011; Patrick et al, 2019; Subbaraman et al., 2015) compared to people who identify as women. Indeed, one study found no instances of alcohol or cannabis use prior to engaging in sexual intercourse without protection against STIs or pregnancy with a casual partner in people who identify as women (Metrik et al., 2016). However, there are no studies examining gender differences within the prevalence of simultaneous alcohol and cannabis-related HRSBs, at times due to lack of prevalence of these behaviors in their samples (Metrik et al., 2016). Thus, it is important to investigate whether these gender differences persist with simultaneous alcohol and cannabis-related HRSBs, which will inform future studies in developing interventions aimed at reducing these HRSBs.
Existing theory has yet to be applied to explain the relationship between simultaneous alcohol and cannabis use and HRSBs. Alcohol Myopia Theory (Steele & Josephs, 1990), the leading theory utilized to define the relationship between alcohol use and HRSBs, states that the disinhibiting effects of alcohol increase attention on salient cues (e.g., sexual arousal) while decreasing the salience of other cues (e.g., STI risks from not using a condom during sexual intercourse), thus increasing risky decision making. Additionally, cannabis use may increase a person's risk for HRSBs through impairing inhibition (Skosnik et al., 2001), increasing risky decision making (Lane et al., 2005; Metrik et al., 2012), and reducing cognitive performance (e.g., attention; Harvey et al., 2007). Further, simultaneous administration of alcohol and cannabis has been shown to increase subjective intoxication effects and behavioral and cognitive impairment, resulting in increased disinhibition (Chait & Perry, 1994; Lukas & Orozco, 2001; Ramaekers et al., 2011). The effects produced by simultaneous alcohol and cannabis use may therefore increase a person's likelihood of making risky decisions and, thus, their risk of engaging in HRSBs beyond either substance alone.
Current Study
Overall, there is a dearth of research on the relationship between simultaneous alcohol and cannabis use and HRSBs. The present study aims to help fill this gap by examining simultaneous alcohol and cannabis use and HRSBs in a large college student sample, investigating novel types of HRSBs (e.g., sexual intercourse after heavy drinking simultaneously with cannabis use), and exploring unique aspects of the simultaneous alcohol and cannabis use-HRSB relationship (e.g., gender differences within this relationship). Thus, the present study aimed to (1) investigate the prevalence of simultaneous alcohol and cannabis-related HRSBs in a college student sample, (2) investigate the associations between simultaneous alcohol and cannabis use and HRSBs (e.g., sex without a condom or another form of protection, sex with multiple partners, or sex after substance use), and (3) examine gender differences within the prevalence of simultaneous alcohol and cannabis-related HRSBs.
METHODS
Participants
A total of 696 college students at a large Midwestern university were recruited for the present study. A total of 162 participants were removed due to not meeting inclusion criteria for the study. Thus, a final sample of 534 participants was utilized. The majority of participants reported identified as a woman (66.9%), 31.6% identified as a man, and the remaining identified as transgender, genderqueer, gender nonconforming, or preferred not to answer. Over half of participants reported their sex assigned at birth as female (67.6%). The majority (88.4%) of participants identified as White, 6.7% identified as Black/African American, 3.2% identified as Multiracial, 2.2% identified as Asian, 1.5% identified as American Indian or Alaska Native, 0.9% identified as Other, 0.7% identified as Middle Eastern, and 0.4% identified as Native Hawaiian or Other Pacific Islander.1 The majority of participants identified as not Hispanic or Latino (91.9%). Participants' average age was 19.04 (SD = 1.66, range 18 to 28 years old) and the majority were first year students (55.9%). Most participants were currently in a relationship with a dating partner (60.8%). Based on the Kinsey Scale (Kinsey, Pomeroy, & Martin, 1948), 77.7% of participants identified as exclusively heterosexual.
Participants were recruited utilizing the Psychology Department's Human Subjects Pool. Prior to participating, participants were able to view a study advertisement on the Human Subjects Pool website that provided a brief description of the study and eligibility criteria, the course credit they would receive, and the approximate study length. To be eligible for the study, participants had to be 18 years or older, used alcohol in the past 12 months, used cannabis in the past 12 months, and be involved in a dating relationship lasting at least one month in the past 12 months (due to this study being part of a larger project aimed at investigating the potential effects of substance use on dating relationships). The informed consent and surveys were completed via Qualtrics.com. Participants viewed a debriefing form describing the purpose of the study, contact information for the study investigators, and local mental health resources after completing the study. All study procedures took approximately one hour and participants received course credit for their psychology course as compensation. The Institutional Review Board approved all procedures prior to data collection.
Measures
Demographics Questionnaire. Participants were asked to report their gender identity, age, year in college, race, ethnicity, sexual orientation, and current relationship status. A dating relationship was defined broadly (i.e., “intimate relationship”) in the present study, thus a relationship may not necessarily have been exclusive.
Alcohol Use. The Alcohol Use Disorders Identification Test (AUDIT) was utilized to assess for alcohol use and problems (Saunders et al., 1993). The AUDIT is a 10-item self-report measure, with scores ranging from 0 to 40, with higher scores indicating increased alcohol use and problems. The AUDIT is a reliable and valid measure for use in college students (e.g., Lundin et al., 2015) and has good internal consistency (Cronbach's alpha in the .80's; Reinert & Allen, 2002). The internal consistency in the current sample was good (α = .77).
Cannabis Use. The Cannabis Use Disorders Identification Test – Revised (CUDIT-R) was used to examine cannabis use (Adamson et al., 2010). The CUDIT-R is an 8-item self-report measure, with scores ranging from 0 to 32, with higher scores indicating increased cannabis use and related problems. The CUDIT-R's internal consistency (α = .91) and discriminant validity in distinguishing cannabis use and cannabis dependence is excellent (Adamson et al., 2010). The internal consistency in the current sample was good (α = .78).
Simultaneous Alcohol and Cannabis Use. One item was utilized to measure past 12-month simultaneous alcohol and cannabis use: “How often did you use both alcohol and marijuana on the same occasion during the past 12 months, so that the effects of alcohol and marijuana overlapped?”, with response options including never (scored as 0), monthly or less, 2 to 4 times a month, 2 to 3 times a week, and 4 or more times a week (scored as 4). This item is similar to prior research examining simultaneous alcohol and cannabis use (Patrick et al., 2018, Subbaraman & Kerr, 2015).
HRSBs. Participants were asked to identify the frequency with which they engaged in HRSBs over the past 3 months, including 1) the number of times they engaged in sexual intercourse without a condom or another form of protection and 2) the number of sexual partners they had, consistent with prior research (e.g., Snipes & Benotsch, 2013). Additionally, participants were asked to identify the frequency of simultaneous alcohol and cannabis-related HRSBs, with the following two items: “How many times did you have sexual intercourse (oral, anal, or vaginal) after having drunk alcohol and used marijuana in the same occasion in the past 3 months?” and “How many times did you have sexual intercourse (oral, anal, or vaginal) after having 4 or more alcoholic drinks if you are a woman, or 5 or more alcoholic drinks if you are a man, while also having used marijuana on the same occasion in the past 3 months?” Three months was chosen for these items due to previous research indicating participants can accurately recall sexual behavior over that timeframe (Napper et al., 2010).
Data Analytic Plan
To begin, we examined the prevalence of simultaneous alcohol and cannabis use and HRSBs (i.e., frequency of sexual intercourse after simultaneous alcohol and cannabis use in past 3 months, frequency of sexual intercourse after heavy drinking and cannabis use in past 3 months, frequency of vaginal or anal sex without a condom or another form of protection in past 3 months, and number of sexual partners in past 3 months) in IBM SPSS Statistics (Version 28.0). Next, we examined bivariate correlations between all study variables. We also conducted partial correlations to examine the associations between simultaneous alcohol and cannabis use and HRSB after controlling for alcohol and cannabis use. After that, we utilized independent samples t-tests to determine whether gender differences between people who identified as men and women existed between simultaneous alcohol and cannabis-related HRSBs variables (e.g., frequency of sexual intercourse after simultaneous alcohol and cannabis use in past 3 months). Finally, we utilized independent samples t-tests to examine whether people who engaged in simultaneous alcohol and cannabis in the past year differed on sex without protection and number of sexual partners compared to people who did not engage in simultaneous alcohol and cannabis use.
RESULTS
The majority (82.2%; n = 439) of participants were past-year simultaneous alcohol and cannabis users, with over one quarter (26.4%; n = 141) reporting simultaneous alcohol and cannabis use two to four times a month. In terms of sexual behavior, participants reported an average number of 1.61 (SD = 1.95) sexual partners in the last 3 months. Further, 57.6% (n = 308) reported having vaginal or anal sex without a condom or another form of protection at least once in the past 3 months. Additionally, 36.5% (n = 195) reported engaging in simultaneous alcohol and cannabis use prior to sexual intercourse at least once in the past 3 months, and 34.1% endorsed heavy drinking simultaneously with cannabis use prior to sexual intercourse at least once in the past 3 months.
Bivariate correlations revealed small to medium effects between study variables (see Table 1). Past-year simultaneous alcohol and cannabis use wassignificantly related to simultaneous alcohol and cannabis use prior to sexual intercourse, heavy drinking simultaneously with cannabis use prior to sexual intercourse, sexual intercourse without a condom or another form of protection, and number of sexual partners. Results also demonstrated that alcohol use and problems were significantly and positively related to both simultaneous alcohol and cannabis use prior to sexual intercourse, heavy drinking simultaneously with cannabis use prior to sexual intercourse, and number of sexual partners. Cannabis use and problems were significantly and positively related to simultaneous alcohol and cannabis use prior to sexual intercourse, heavy drinking simultaneously with cannabis use prior to sexual intercourse, and sexual intercourse without a condom or another form of protection. Partial correlations, while controlling for alcohol and cannabis use, revealed positive and significant associations between simultaneous alcohol and cannabis use and two HRSB variables: simultaneous alcohol and cannabis use prior to sexual intercourse (r(436) = .22, p < .001) and heavy drinking simultaneously with cannabis use prior to sexual intercourse (r(436) = .21, p < .001).
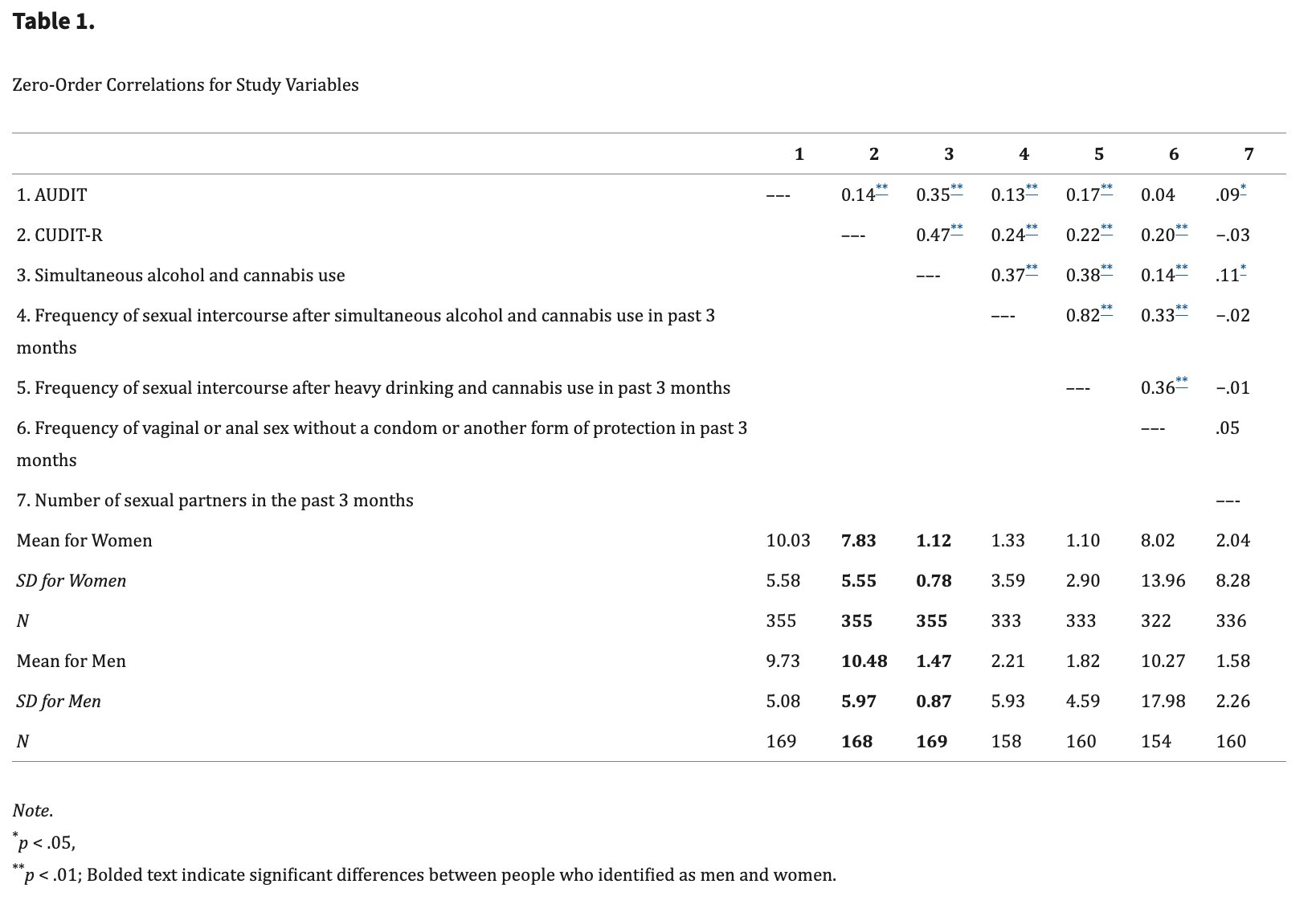
Independent samples t-test results revealed no gender differences between people who identified as men and women on simultaneous alcohol and cannabis-HRSBs (see Table 1). People who did not identify as men and women (e.g., transgender, gender nonconforming) were not included in analyses due to small sample size (N = 6).
Independent samples t-tests did yield differences on HRSBs when comparing past year simultaneous alcohol and cannabis users to non-past year simultaneous users. Results indicated that past year simultaneous alcohol and cannabis users reported more instances of sexual intercourse without a condom or other forms of protection in the past 3 months (M = 9.31, SD = 16.02) than non-simultaneous users (M = 5.71, SD = 10.79; t(481) = 1.95, p = 0.05). Finally, no differences were found between past year (M = 2.05, SD = 7.51) and non-past year simultaneous alcohol and cannabis users (M = 1.15, SD = 0.82) in number of sexual partners in the past 3 months t(501) = 1.08, p = 0.28.
DISCUSSION
The present study found that over one-third (36.1%) of participants reported engaging in simultaneous alcohol and cannabis use prior to sexual intercourse in the past 3 months, and 34.1% endorsed heavy drinking (four or more drinks for women, five or more for men) simultaneously with cannabis use prior to sexual intercourse in the past 3 months. Previous studies examining simultaneous alcohol and cannabis use and HRSBs have found similar prevalence rates. For instance, a retrospective study examining HRSBs and simultaneous alcohol and cannabis use over a 60-day period found that unprotected sex with a casual partner was reported on 29% of cannabis use days when participants also reported heavy drinking on the same day (Metrik et al., 2016). These prevalence rates provide important descriptive information regarding simultaneous alcohol and cannabis use and sexual intercourse. These results indicate a need to continue investigating the impact of simultaneous alcohol and cannabis use and HRSBs in college students, given the prevalence of these behaviors and associated negative outcomes.
Additionally, results of partial correlations indicated that after controlling for alcohol and cannabis use, simultaneous alcohol and cannabis use was significantly related to sexual intercourse after engaging in simultaneous alcohol and cannabis use and sexual intercourse after heavy drinking simultaneously with cannabis use. Simultaneous alcohol and cannabis use was not significantly related to sexual intercourse without a condom or another form of protection and number of sexual partners after controlling for alcohol and cannabis use. This suggests individual, in the bivariate correlations, alcohol and cannabis use may have been driving the significant relationship between simultaneous alcohol and cannabis use and these specific HRSBs. Further replication of these results is needed, but they may indicate a need to specifically target individual alcohol and cannabis use within simultaneous alcohol and cannabis users to reduce sexual intercourse without protection against STIs and pregnancy.
Further, the present study did not find any gender differences within simultaneous alcohol and cannabis-related HRSBs. However, people who identify as men are more likely to engage in risky sexual behavior (MacDonald et al., 2000; Nolen-Hoeksema, 2004), and prevalence of simultaneous alcohol and cannabis use is substantially higher among people who identify as men than people who identify as women (Brière et al., 2011; Patrick et al, 2019; Subbaraman et al., 2015). There is a paucity of existing research investigating gender differences within simultaneous alcohol and cannabis-related HRSBs and more research is necessary to elucidate whether simultaneous alcohol and cannabis use differentially impacts risk of engaging in HRSBs for women than men to better inform future interventions.
Additionally, the present study found differences within past year and non-past year simultaneous alcohol cannabis users, with past year simultaneous alcohol and cannabis users engaging in increased instances of sexual intercourse without a condom or other form of protection. No differences between users and non-users were found within number of sexual partners over the past 3 months. These results indicate simultaneous alcohol and cannabis use may increase the prevalence of certain types of HRSBs. Future studies are necessary to replicate this finding but may suggest targeting simultaneous alcohol and cannabis use to reduce specific types of HRSBs (e.g., sex without protection against STIs).
The present study had a few limitations. The majority of the sample identified as White, heterosexual, and as women, which decreases the generalizability of the findings to more diverse college populations. Additionally, participants were required to be in a relationship in the past year, which also decreases generalizability of the present findings. For instance, participants may have primarily engaged in sexual behavior with established partners. Previous research has indicated condom usage may vary depending on partner type, with decreased usage occurring with established partners (Macaluso et al., 2000). Further, the present study took place in a Midwestern state in which recreational cannabis use was not legal, and thus the findings may not generalize to states with different laws regarding recreational use. Future research should continue to investigate the prevalence of, and gender differences within, simultaneous alcohol and cannabis use and HRSBs in states in which recreational cannabis use is legal. Additionally, the present study consisted of college students. While simultaneous alcohol and cannabis use and HRSBs are prevalent in this population, future research should examine these behaviors in community-based young adult samples. Further, the present study was cross-sectional, and it is possible gender differences within the simultaneous alcohol and cannabis use and HRSB relationship may differ when these constructs are examined over time. The cross-sectional nature of the present study also does not provide causality. It is possible that simultaneous alcohol and cannabis use you do not increase risk for HRSBs, but instead an outside construct, such as impulsivity (e.g., sensation seeking), may be driving the relationship between these variables. Additionally, the effect sizes between simultaneous alcohol and cannabis use and the HRSBs examined (e.g., sex without a condom or another form of protection) were mostly small and were not significant when controlling for alcohol and cannabis use. Additional replication in other studies is needed to further confirm these findings. Further, the Kinsey Scale was utilized to measure sexual orientation. This scale does not provide specific options for sexual orientation (e.g., bisexual, lesbian), thus we were unable to provide this demographic information. Future studies investigating sexual orientation in people who use simultaneous alcohol and cannabis and engage in HRSBs is warranted. Finally, the present study did not ask about context of HRSBs with simultaneous alcohol and cannabis use (e.g., did HRSBs occur with established or casual partners). Given the prevalence of simultaneous alcohol and cannabis use prior to sexual intercourse in the current sample, it is important for future studies to determine whether this use leads to sex without protection against STIs or pregnancy and other types of HRSBs.
There are numerous directions for future research regarding simultaneous alcohol and cannabis-related HRSBs. For instance, future research could expand the types of simultaneous alcohol and cannabis-related HRSBs to examine (e.g., simultaneous alcohol and cannabis use prior to sexual behaviors other than sexual intercourse, such as touching a partner underneath their clothing). Future research could additionally investigate the prevalence of and gender differences within simultaneous alcohol and cannabis-related HRSBs in non-college young adults to determine if results generalize to this population. Additionally, future investigations could also utilize event-level data (e.g., daily diary assessments) to better investigate the proximal relationship between simultaneous alcohol and cannabis use and HRSBs or timeline follow back methodology to reduce recall bias. With prior research indicating simultaneous alcohol and cannabis use effects are additive (Chait & Perry, 1994; Ramaekers et al., 2011), additional research is necessary to determine whether simultaneous alcohol and cannabis use may impart additional risk for HRSBs above either alcohol or cannabis use alone. Overall, future research is necessary to replicate and extend the present study's findings.