Abstract
Objective Peer support specialists (PSSs) can effectively link patients with substance use disorders (SUD) to treatment. These specialists can engage patients in treatment after emergency department (ED) visits or inpatient hospitalization, crucial points in time when these patients have contact with the health care system. We describe success of PSSs in recruiting SUD patients into treatment, with attention to racial disparities in linkage to care.
Methods This is a retrospective, observational cohort study performed at an urban, academic medical center. Patients with SUD who indicated interest in pursuing addiction treatment were linked with PSSs by staff at discharge from the ED or inpatient hospitalization. PSSs then transported willing patients to a partnering addiction treatment facility. The treatment facility provided data on successful linkage to care, defined as enrolling in an inpatient or outpatient treatment program. Our primary outcome was successful enrollment in treatment after engagement. The secondary outcome was patients' agreement to transport to the treatment facility after engagement by a PSS. We performed subgroup analysis of patients by self-described race.
Results A total of 785 patients met inclusion criteria for the study: 168 Black patients and 617 White patients. White patients were more likely than Black patients to be enrolled in treatment by PSSs (adjusted odds ratio [aOR; 95% confidence interval {CI}] = 1.61 [1.11 to 2.34]), after adjusting for the effects of age, sex, insurance, and marital status, p = 0.012. We found no statistically significant differences between races in agreeing to be transported for the total sample or inpatient subjects. For ED patients, White individuals were more likely to be transported to treatment compared to Black or African American patients (adjusted odds ratio [aOR; 95% confidence interval {CI}] = 1.50 [1.00 to 2.23]).
Conclusion Our results provide evidence of racial disparities in successful linkage to care by PSSs among patients with SUD. Fewer Black patients were successfully linked to care when approached in the ED, where the majority of these patients were engaged, and after controlling age, sex, insurance, and marital status. Future research should study factors that drive these disparities, and how to successfully link all patients to care.
Highlights
Peer support specialists may be an effective way to link patients with substance use disorders to treatment
Black patients with SUD were not as likely to be engaged in treatment by peer support specialists in the ED
Evaluating interventions for evidence of racial disparities is an important step in improving health equity
1. Introduction
The United States has witnessed increased mortality related to substance use disorders (SUD) in the last 20 years, mostly driven by the opioid epidemic (Hedegaard et al., 2017). Public health experts prioritize research on how to best link these patients to evidence-based treatments.
Interest and funding for the use of peer support specialists (PSSs) have increased over the past several years (Myrick & del Vecchio, 2016). These specialists, with similar life-experience to patients with SUD, offer unique advantages in engaging SUD patients into treatment. These advantages include helping patients navigate services, supporting behavior change, harm reduction, and relationship building. Compared to other types of intervention, PSSs may offer improved accessibility to treatment and social support once engaged in treatment (Jack et al., 2018). A 2016 systematic review of the literature found 24 studies involving the use of PSSs in SUD, with seven randomized controlled trials (Bassuk et al., 2016). Authors found many positive effects of PSSs, including reduced substance use and SUD relapse rates, improved relationships with treatment provider, increased retention in treatment programs, and greater treatment satisfaction.
Linking patients to evidence-based addiction treatment is challenging, with one study finding only 17% of patients engaged in any form of SUD treatment after hospitalization for opioid use disorder (OUD) or opioid overdose (Naeger et al., 2016). This lack of access or engagement in addiction treatment disproportionately affects Black communities, with lower rates of addiction treatment even when controlling for sociodemographic characteristics (Pinedo, 2019).
Previous research has suggested that Black patients may be apprehensive about acknowledging mental health illness or accessing mental health care due to perceived stigma (Ward et al., 2013). Additionally, these patients are underrepresented in the mental health workforce. Despite that 13.2% of the U.S. population identifies as Black, only 2% of psychiatrists (Starks, 2021) and 4% of psychologists (Hamp et al., 2015) identify as Black. Due to racial discrimination in medical research and clinical settings, mistrust in medical providers is more common among Black patients in the United States (Boulware et al., 2003).
In this investigation, we compare the effectiveness of PSSs in linking Black and White patients to SUD treatment. We also analyze the subgroups of patients from the ED and inpatient settings to assess if racial disparities exist in either location of intervention.
2. Methods
2.1. Setting and participants
This study is a retrospective, observational, cohort study performed at an urban academic tertiary-care hospital, in partnership with a local addiction treatment center. The University of Louisville institutional review board approved this retrospective review.
University of Louisville Hospital (ULH) is an academic, tertiary-care center located in Louisville, Kentucky. Annual patient volumes for the emergency department (ED) average 60,000 visits. The affiliated addiction treatment center (Centerstone) has a large network, with 170 offices spread over five states. They are located two blocks from ULH, with a bus stop located directly in front of the treatment center. Centerstone offers both inpatient and outpatient treatment for SUD, including for OUD, alcohol use disorder (AUD), and stimulant use disorder (StUD). They accept most private insurance, Kentucky Medicaid, and full fee and sliding scale payment plans. Appointments for outpatient treatment can be scheduled Monday through Saturday during both day and evening hours.
Inclusion criteria involved engagement by a PSS after expression of interest to pursue treatment at the partnering addiction treatment center. ED physicians and/or nurses completed screenings for SUD on ED patients based on self-reported history of current or previous substance use, regardless of chief complaint at time of presentation or frequency of substance use. Providers offered contact with PSSs (available 24/7) per their discretion and patient willingness. This process was followed for inpatients as well, who could be referred to PSSs regardless of admitting diagnosis. We excluded repeat visits, pregnant patients, and those under 18 years old. Centerstone provided patient data for all subjects who met criteria between May 2018 and September of 2019.
PSSs were employed by Centerstone Acute Rehabilitation Center. To qualify to become a PSS, employees had to have shared life experience with the patients related to substance use, two years of sobriety, two weeks of training with a certification test, and 6 h of continued training per year. While the training of PSSs and transport procedures are standardized, individual patient interviews are not standardized. They are overseen by a licensed professional clinical counselor. PSSs initially meet with the patients and offer resources, including escorting the patient to the rehab facility. Next, they perform the ongoing roles of connecting patients with sponsors, other rehab facilities, and if needed, housing and employment resources.
2.2. Patient recruitment
When a patient expressed interest in pursuing treatment, hospital staff would contact Centerstone, which would send the on-call PSS to meet in person with the patient prior to discharge from the ED or the day of discharge from inpatient admission. The same PSS pool served ED and inpatients. Patient engagement in outpatient or inpatient admission was recorded by the addiction treatment center. The research team conducted a retrospective review of hospital electronic health records to determine patient age, race, insurance status, marital status, medications for opioid use disorder (MOUD) use, and type of substance use disorder.
2.3. Study outcomes and analysis
The primary outcome was differences in SUD treatment enrollment based on race. The team defined treatment enrollment as a patient attending an outpatient or inpatient treatment visit with the affiliated addiction treatment center. The secondary outcome was use of same-day transportation to the treatment facility. The study assessed these outcomes in the subgroup of patients engaged in the ED and those engaged in the inpatient setting.
This paper presents data as median and interquartile ranges for age and frequencies and proportions for all other variables to summarize patient characteristics and outcome variables among the entire sample and stratified by race/ethnicity. The research team used binary logistic regression to determine if differences existed in treatment engagement based on race. We checked assumptions prior to full analyses, including detection of multicollinearity diagnostics and outliers. The research team selected model covariates based on established racial/ethnic variation in health care outcomes related to social determinants of health, including sex (female, male), insurance status (insured, not insured), marital status (married, not married), and age (continuous variable). This paper presents regression results with adjusted odds ratios (aORs), confidence intervals (Cis) for aORs, and p values. All comparisons were two-sided and statistical significance was at p < 0.05. Study staff completed data analysis using IBM SPSS Version 27.
3. Results
A total of 785 patients met inclusion criteria: 168 Black or African American and 617 White patients. Black or African American patients were older (median age 41 years) compared to White patients (median age 37 years) and had a higher percentage of individuals with medical insurance. Both groups had similarly higher percentages of male patients (Table 1).
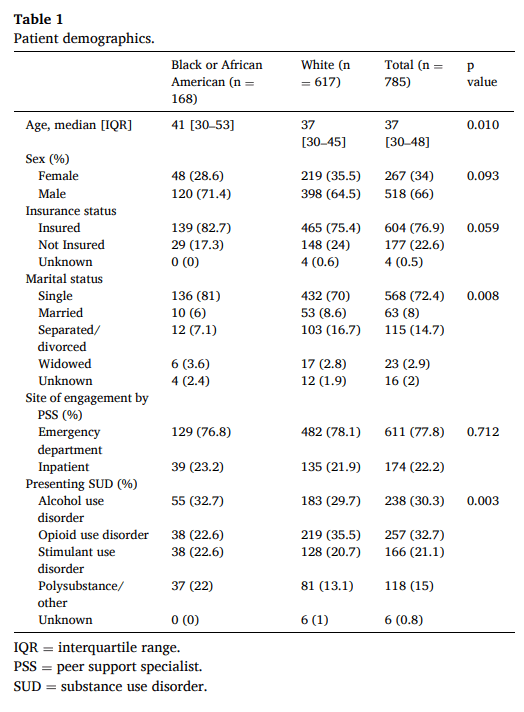
White patients had higher likelihood of OUD, while Black or African American patients had a higher rate of polysubstance use. Each group had similar percentages of patients with AUD and StUD. For the 257 individuals who had OUD, 43 were taking a MOUD. Stratified by race, 4 (10.5%) Black or African American patients with OUD were on an MOUD, compared to 39 (17.8%) White individuals with OUD. Table 1 provides patient demographics.
Logistic regression results revealed that White patients were more likely to enroll in treatment compared to Black or African American patients (adjusted odds ratio [aOR; 95% confidence interval {CI}] = 1.61 [1.11 to 2.34]), after adjusting for the effects of age, sex, insurance, and marital status, p = 0.012. No statistically significant differences occurred in treatment enrollment by race for inpatient subjects (Table 2), but ED patients revealed statistically significant differences. White ED patients were more likely to enroll in treatment compared to Black or African Americans ED patients (adjusted odds ratio [aOR; 95% confidence interval {CI}] = 1.93 [1.25 to 2.99]), after adjusting for age, sex, insurance, and marital status, p = 0.003.
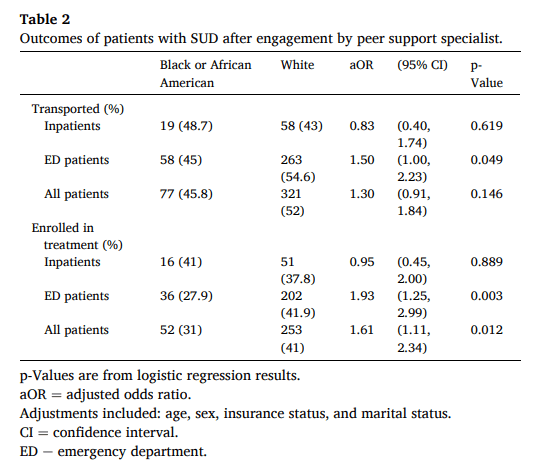
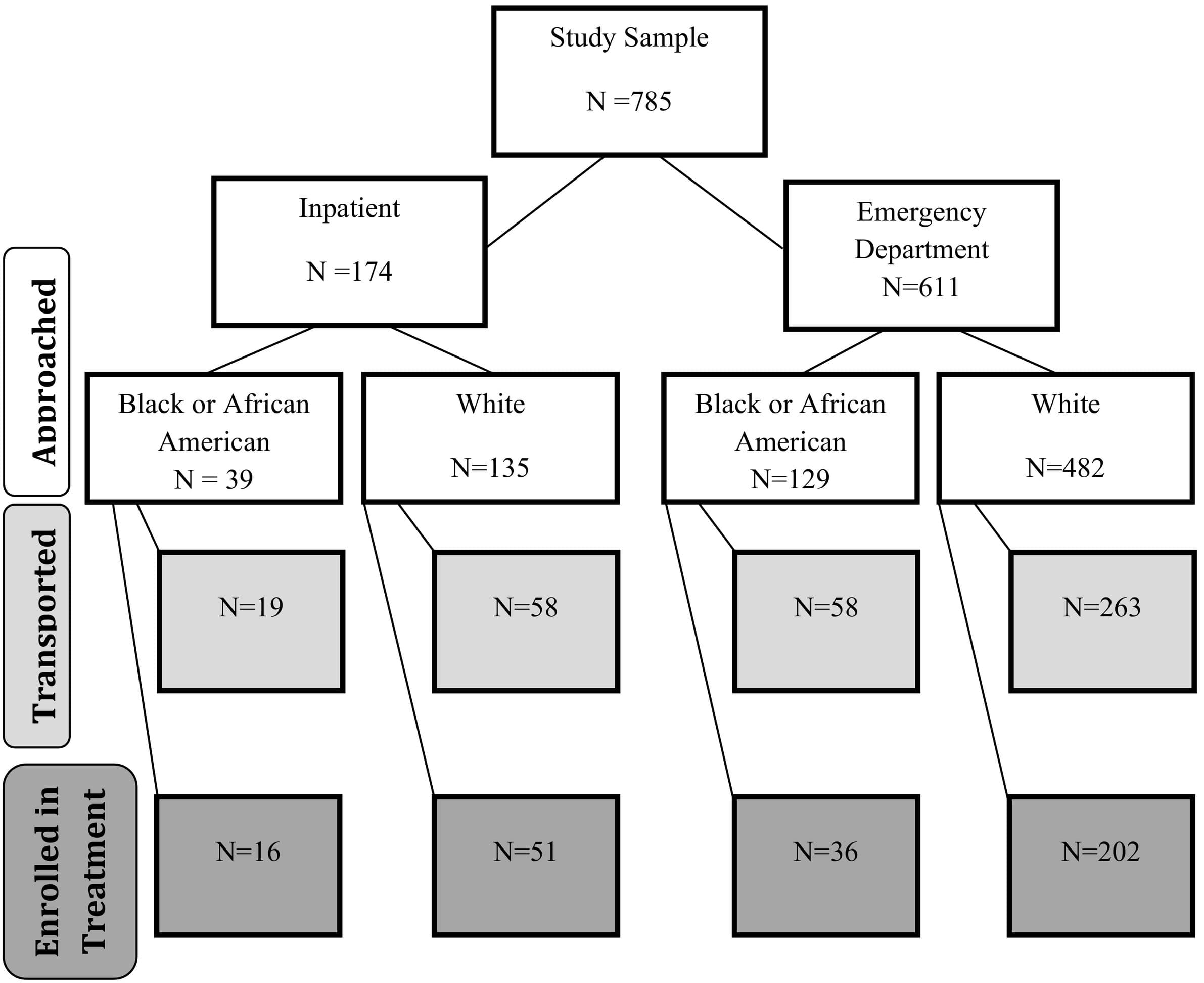
To address the secondary outcome, the team looked for differences in patient same-day transport to the treatment facility by race. Results indicated no statistically significant differences between races for the total sample or inpatient subjects in same-day transport. For ED patients, White individuals were more likely to be transported to treatment compared to Black or African American patients (adjusted odds ratio [aOR; 95% confidence interval {CI}] = 1.50 [1.00 to 2.23]), after adjusting for age, sex, insurance, and marital status, p = 0.049. Fig. 1 shows number of patients meeting the primary and secondary outcomes within each race and clinical setting subgroup. Table 2 provides analysis of study outcomes stratified by race and clinical setting engagement site.
4. Discussion
Our data highlight disparities in outcomes among Black patients receiving referral to SUD treatment by peer support specialists. In this study, Black patients recruited from the ED were less likely to be transported to or enroll in treatment offered by PSSs. This difference was not observed in the patients recruited from the inpatient setting. The same PSS group was responsible for engaging patients at discharge from either the ED or inpatient setting, so differences in background, training, and demographics of the PSSs should not account for these findings. Inpatients do have longer lengths of stay than patients discharged from the ED. Therefore, inpatients potentially had a longer time since last substance use, and could have developed more trust in medical providers.Results showed notable differences between the demographics of each group, which may play some role in the differences in successful enrollment in treatment. Black patients had a median age of 41, significantly older than White patients (median age 37). This finding is consistent with previous research that demonstrates that Black patients tend to have higher prevalence of SUD at older ages than White patients (Vasilenko et al., 2017). Alcohol and opioid use disorders were most common in the overall population, with OUD most prevalent in Whites and AUD and polysubstance use most prevalent in Black patients.Black patients had overall lower rates of MOUD use compared to White patients, though overall existing MOUD was low among all patients. Similar to our findings, research has demonstrated that Black patients have lower rates of access to SUD treatment, particularly those with OUD, with White patients receiving 12.7 million of the 13.4 million visits resulting in a buprenorphine prescription between 2012 and 2015 (Lagisetty et al., 2019).Previous work has suggested that outpatient SUD treatment programs are less likely to retain Black patients through to the completion of treatment regardless of substance of choice, even after controlling for geographic clustering or socioeconomic status (Mennis & Stahler, 2016). However, limited research has investigated how to effectively enroll diverse patient populations in treatment, and even less directly investigated the role of PSSs.In other areas of behavioral health, clients attend more appointments and have improvement in global assessment of function when matched with counselors of similar race (Kim & Kang, 2018). However, racially matching PSSs to clients may not be practical or feasible in situations where one PSS engages a high volume of clients. Another solution could involve providing cultural sensitivity training to PSSs. A previous study on targeting culturally appropriate SUD treatment to adolescent minorities found a significant reduction in substance-use levels (Steinka-Fry et al., 2017).Preliminary studies assessing the effectiveness of PSSs in patients with SUD have yielded mostly positive results, including decreased substance use, increased treatment retention, and improved treatment satisfaction (Eddie et al., 2019). Implementation of PSSs after ED visits has demonstrated preliminary feasibility. In Rhode Island, PSS contact led to success in linking patients with OUD to treatment (Waye et al., 2019) and training patients to use naloxone provided by the ED (Samuels et al., 2018). .Research should continue to investigate how to best facilitate PSS connection with SUD patients while mitigating racial disparities in the context of social determinants of health.
5. Limitations
This study incorporated data from a single urban, academic facility with high endemic rates of substance use disorders, thus its findings may have limited generalizability to other populations. The study team pulled the racial category data directly from electronic medical records, thus they are potentially subject to inconsistencies; though these data are generally recorded by asking the patient his or her race. Some heterogeneity existed between Black and White cohorts, with statistically significant differences in age, marital status, and presenting SUD. Patients were referred based on the discretion of the treating physician and nurse, so selection bias may have occurred or racial differences in who was referred to be engaged by PSSs. The study is retrospective, thus limited by the data collected and provided by the affiliated treatment center. The affiliated treatment center did not provide data on the race/ethnicity of PSSs, and we do not know the importance of this factor in the patient/PSS relationship. Although the study hypothesized that enrollment in a long-term program would lead to higher rates of long-term treatment adherence, no longitudinal data were available from the affiliated partner to evaluate this hypothesis.
6. Conclusion
This study demonstrates that Black patients with SUD engaged by PSSs in the ED were not as likely to successfully enroll in treatment compared to White patients after controlling for age, sex, insurance, and marital status. Evaluating interventions for substance use disorders for disparities between racial groups is an important step in achieving health equity between these groups. Race is a social construct, and achieving this health equity requires us to evaluate how these interventions can be improved. Research should continue to determine how to effectively utilize peer support to engage diverse SUD patient populations.
Financial support
None.
CRediT authorship contribution statement
IS and MH designed the study. CW, IS, AK, and BM performed data extraction on overall data set. JS provided statistical analysis for the project and analyzed data. CW and IS drafted the manuscript, and all authors contributed to revision of the final paper.
Declaration of competing interest
No conflicts of interest to report.