Abstract
This study aimed to 1) describe the prevalence of Adverse Childhood Experiences (ACE) in relation to the type of substance used (alcohol or cannabis) among adults seeking treatment for Substance Use Disorder (SUD) in Greenland, and 2) examine whether an association exists between ACE and the type of substance used (alcohol and/or cannabis). The analysis was conducted using register data from individuals receiving SUD treatment in Greenland between 1 June 2020 to 31 December 2022 (N = 1037). The results showed a higher prevalence and a greater variety of ACE among women compared to men. Among men, no significant associations were found between ACE and the substance categories. However, among women, unstable conditions in the childhood home were associated with high use of either alcohol or cannabis. Additionally, high cannabis use was significantly associated with parent(s) with cannabis use and physical abuse for women. No cumulative effect of the number of ACE, and any type of substance use was found. Growing up with parents with alcohol problems emerged as the most frequently reported ACE for both sexes (reported by 74.6% of women and 62.7% of men).
Introduction
Adverse Childhood Experiences (ACE) refer to circumstances in childhood that may negatively affect physical and mental health later in life. ACE include direct harm (such as physical abuse, emotional abuse, and sexual abuse) and indirect harm through environmental factors (such as neglect, substance use, and mental illness within the household). Numerous studies across diverse populations have documented that ACE are linked to a broad range of health issues extending into adulthood, including mood and anxiety disorders, self-harming behaviours, frailty, and communicable and non-communicable diseases. Furthermore, ACE are closely associated with the development of Substance Use Disorder (SUD). Studies of Alcohol Use Disorder (AUD) have even suggested a dose–response relationship between the number of different ACE and the risk of developing AUD later in life. Research, particularly from North America, has found that Indigenous populations are more likely to experience ACE and to be exposed to multiple ACE compared to non-Indigenous populations. In Greenland, only 16.7% of school children aged 15–17 reported having experienced no ACE, while 56.1% reported having experienced two or more of the ten ACE studied. Childhood exposure to parents’ AUD, particularly in combination with sexual abuse, has been linked to AUD in adulthood, homelessness, suicidal thoughts, and mental health challenges.
Previous research has indicated that ACE are stronger predictors of Cannabis Use Disorder (CUD) than AUD. Cannabis, as a drug, shares many of its effects with substances such as alcohol, tranquilisers, opiates, and hallucinogens. Its effects include anxiolytic, sedative, analgesic, and psychedelic properties, as well as stimulation of appetite. Furthermore, cannabis has numerous systemic effects including muscle relaxation. Given these attributes, the mood-altering effects of cannabis may support the hypothesis that individuals who have suffered traumatic events, such as sexual abuse, may prefer cannabis over alcohol.
Cannabis, along with other drugs not prescribed by a doctor, is illegal in Greenland. Both alcohol and cannabis are present all over Greenland. Annually, 1–2% of the adult population in Greenland receives treatment for SUD. AUD is the most prevalent SUD encountered in treatment, followed by CUD. Although the incidence of CUD is increasing, other drugs remain rare in the treatment institutions.
To our knowledge, no studies have described the prevalence of ACE among Arctic Indigenous individuals seeking treatment for SUD nor have any studies explored the associations between ACE and the type of substance used. This study aims to 1) describe the prevalence of ACE in relation to the type of substance used (alcohol or cannabis) among adults seeking treatment for SUD in Greenland and 2) examine whether an association exists between ACE and the type of substance used (alcohol and cannabis).
Materials and methods
Study sample
Greenland has a population of approximately 56,000, residing in 16 small towns and around 60 villages along nearly 2,000 kilometres of coastline. The largest town is Nuuk, the capital, with approximately 20,000 inhabitants. Due to the absence of roads between settlements, access is typical via boat or plane. Since 2016, the government has provided free SUD treatment. Currently, outpatient treatment clinics operate in the largest town of each of the five municipalities, allowing 62% of the population immediate treatment access. Individuals from smaller towns and settlements are either treated by travelling counsellors or in Nuuk.
Since 2016, all individuals commencing with SUD treatment have been registered in the National Database on Substance Abuse Treatment. Data in the database are collected at the point of referral to treatment and initiation of treatment (baseline interview). The baseline interview incorporates a slightly modified version of the Addiction Severity Index (KN-ASI), which includes data on ACE and socioeconomic covariates. These interviews are a part of the routine assessment conducted at the beginning of treatment and in planning further treatment; participants complete the questionnaire alongside a therapist.
In Greenland, around 90% of the population is Inuit, while the remaining 10% are primarily of European descent. In Greenland, ethnicity of the population is not registered. It is assumed that the study sample mainly consists of Greenlandic individuals because the mother tongue of 99% of the individuals in treatment is Greenlandic.
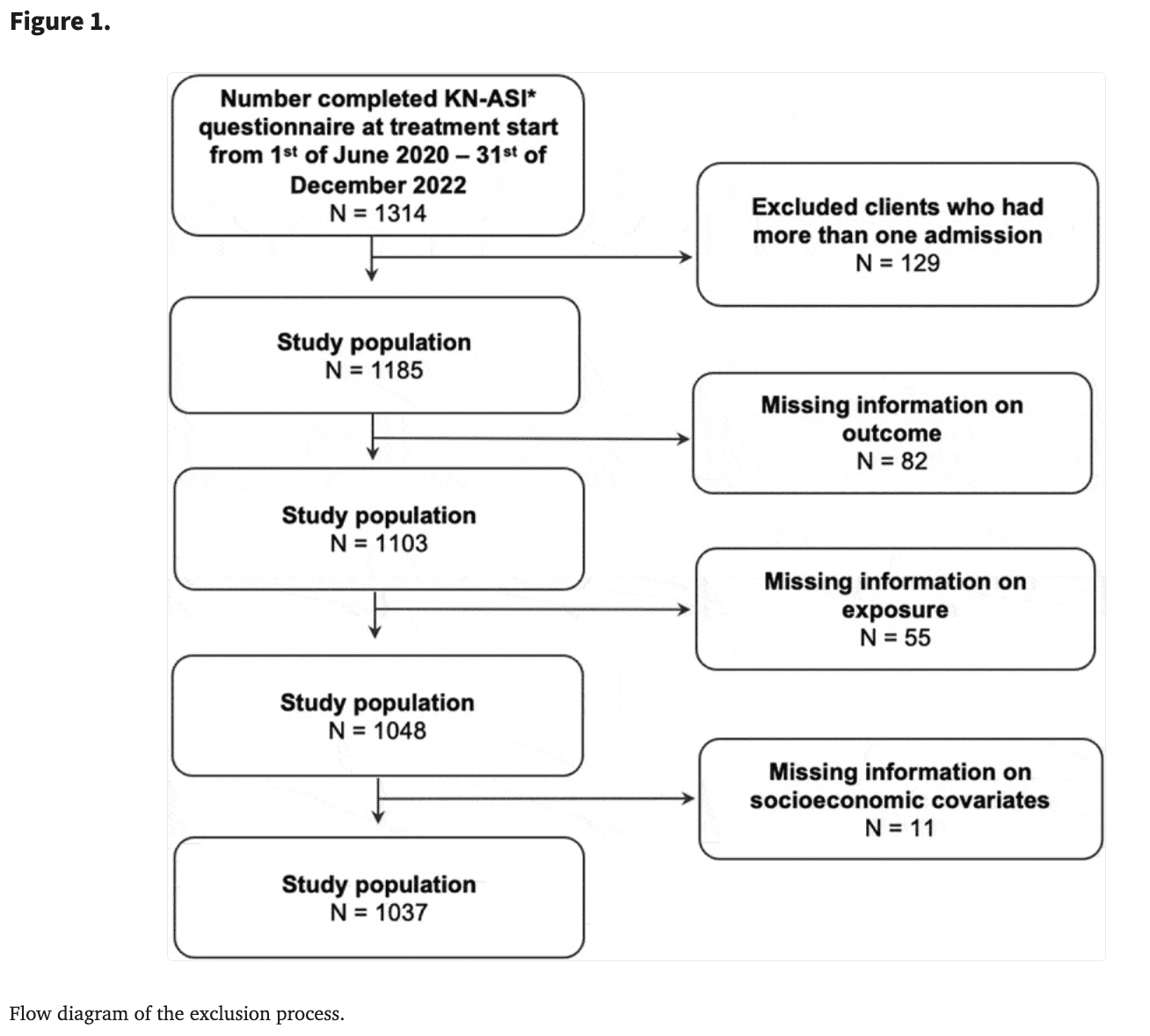
In this study, data from all individuals treated between 1 June 2020 and 31 December 2022, were extracted from the database. 1 June 2020 marks the introduction of the KN-ASI questionnaire. The dataset included information from 1,314 treatment courses. Individuals with more than one treatment course (N = 129), missing data on SUD (N = 82), ACE (N = 55), or socioeconomic covariates (N = 11) were excluded, leaving data from 1,037 individuals for analysis. The exclusion process is illustrated in Figure 1.
Substance use disorder
AUD categorisation is defined based on the widely used and reliable Alcohol Use Disorders Identification Test (AUDIT) developed by WHO. Screening with AUDIT has proven useful for both individual and national treatment planning in Greenland. AUDIT comprises 10 items scored from 0 to 4, yielding a maximum score of 40. The domains of AUDIT pertain to recent alcohol use, symptoms of alcohol dependence, and alcohol-related problems. A score between 0 and 7 indicates a low probability of alcohol-related problems, while scores from 8 to 15 indicate hazardous drinking, scores from 16 to 19 denote harmful use, and scores above 19 suggest further diagnostic evaluation for alcohol dependence. In this study, alcohol use was dichotomised into “low alcohol use” (low probability of alcohol-related problems and hazardous drinking) and “high alcohol use” (harmful use and probable dependency).
Cannabis use was assessed using the question “How often do you smoke cannabis?” with reference to the last 6 months. Answers were dichotomised into “high cannabis use” (daily and more than once a week) and “low cannabis use” (less frequently than once a week and no use).
A category for “high use” was aggregated from the two high use categories. Individuals were categorised as having “high use” if they had either “high alcohol use” or “high cannabis use”. If they did not have either “high alcohol use” or “high cannabis use” they were categorised as having “low use”.
ACE
Data on seven categories of ACE were collected and analysed in this study: alcohol use in either mother or father, cannabis use in either mother or father, mental health problems in either mother or father, having had unstable conditions in childhood home, have been sexually abused, have been emotionally abused, and have been physically abused. SUD or mental health problems in either mother or father were assessed through the questions: “Has any of your biological parents had what you would consider to be notable alcohol/cannabis/mental health problems that needed treatment?”. Answers were collected about both mother and father (no, yes, not relevant/don’t know) and were combined to create variables for parental alcohol use, parental cannabis use, and parental mental health problems. One ACE was assigned to an individual if either one or both parents were considered to have alcohol, cannabis, or mental health problems. The conditions in the childhood home were dichotomised into stable or unstable conditions in the childhood home. Stable conditions were categorised from the answer “good parental care present” while unstable conditions were categorised from the answers “insufficient parental care” and “great lack of care”. Information about childhood abuse was also included using responses to three questions: “Has anyone emotionally, physically, or sexually abused you before you turned 18?”. The answer “yes” was categorised as an ACE for each kind of abuse.
Studies have shown that 0–1 ACE is common especially in Arctic populations. Therefore, with inspiration from Felitti, ACE was categorised into 0–1 adverse experiences, 2–4 adverse experiences and 5+ adverse experiences.
Socioeconomic covariates
Socioeconomic covariates (age, sex, education, affiliation to labour market, chronic physical conditions and treatment for a psychiatric disease) were included in the analysis. Sex was divided into male and female. Age was divided into three groups: less than 30 years, 30–44 years, and 45 years and older. Education was divided into two groups: no secondary education and secondary education (short vocational, long vocational and university). Regular employment over the past three years was divided into two groups: affiliation with the labour market and no affiliation with the labour market. Affiliation with the labour market included full-time work, part-time work or self-employed (fisher, hunter or other). No affiliation with the labour market included student allowance, pension, welfare, stay-at-home, and other. Chronic physical conditions or diseases impacting daily life were divided into two groups: chronic physical conditions and no chronic physical conditions. Prior psychiatric treatment is divided into two groups: prior psychiatric treatment and no prior psychiatric treatment.
Statistical analysis
All statistical analyses were conducted using the SPSS version 25. For descriptive analysis of the socioeconomic covariates and ACE, Pearson’s χ2-test with a two-sided significance level of 5% was applied. A logistic regression model was employed to evaluate the odds ratio (OR) of high alcohol use or high cannabis use, adjusting for socioeconomic covariates in a second model. The results are presented as ORs or adjusted odds ratios (AOR) with 95% confidence intervals. A significance level of p-value <0.05 was employed. The association between ACE categories and the number of ACE was examined for “high use”, “high alcohol use”, and “high cannabis use”, stratified by sex, in both unadjusted and adjusted models. Adjustments were made for age, education, affiliation with the labour market, mental illness, physical illness, and high alcohol/cannabis use, respectively.
Results
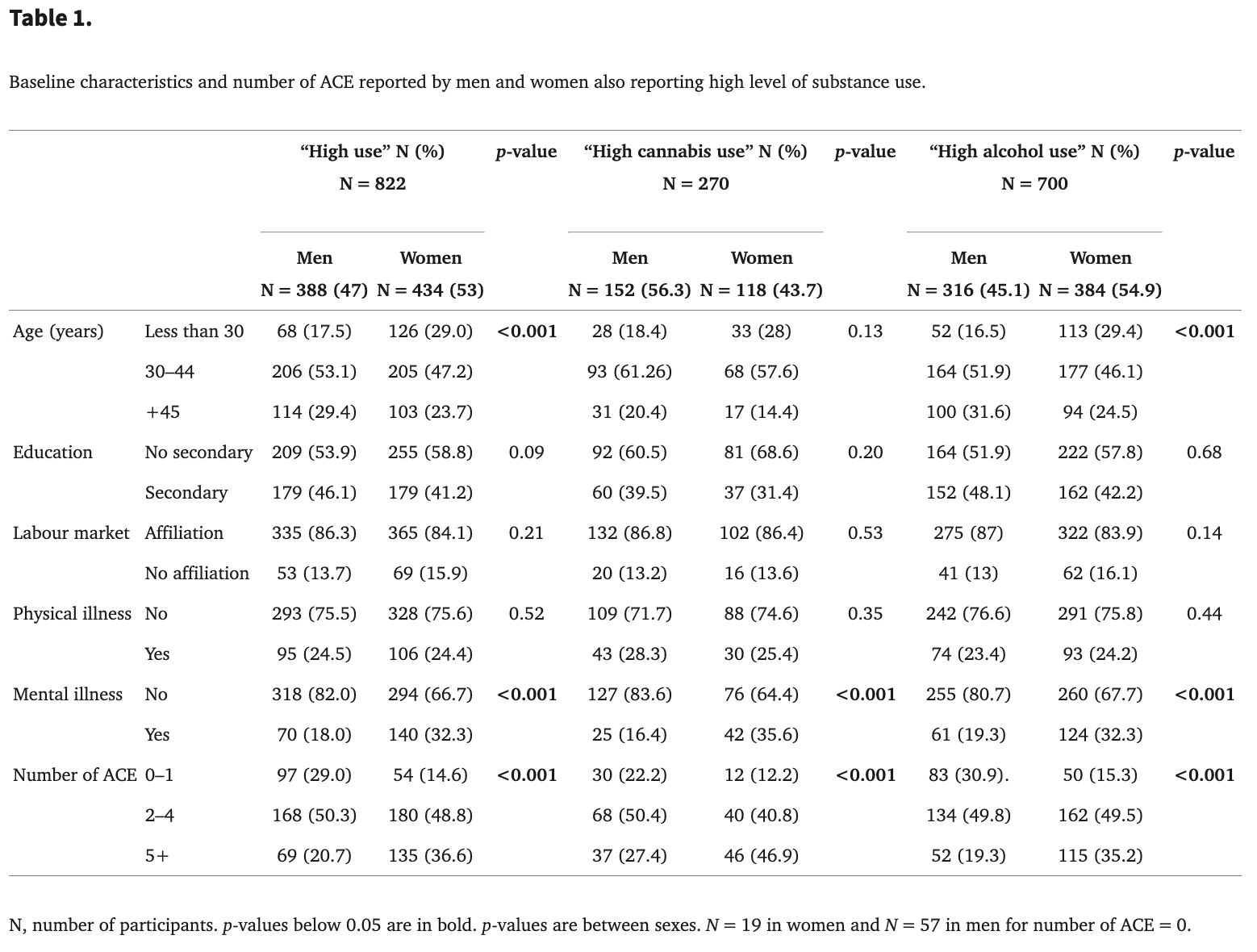
Demographic and socioeconomic covariates are displayed in Table 1 for men and women categorised by “high use” (high use of either alcohol or cannabis use), “high alcohol use”, and “high cannabis use”. More women (29.0%) than men (17.5%) were aged “less than 30”, whereas more men (29.4%) than women (23.7%) were “45 years or older” (p < 0.001). Among those with “high cannabis use”, more men (39.5%) than women (31.4%) possessed a secondary education (p = 0.045). Across all three categories (“high use”, “high cannabis use” and “high alcohol use”), women reported a higher prevalence of mental illness (32.3%–35.6%) compared to men (16.4%–19.3%) (p < 0.001). Women reported five or more ACE more frequently than men in all three categories of high use (20.7% of men compared to 36.6% of women in “high use”, 27.4% of men compared to 46.9% of women in “high cannabis use”, and 19.3% of men compared to 35.2% of women in “high alcohol use”). An increase in “high use” with more ACE was found for “high cannabis use” in both men (p = 0.011) and women (p = 0.017), although no such association was evident for “high use” or “high alcohol use”. A non-responder analysis showed no significant differences between responders and non-responders regarding age, sex, education, or employment status.
Prevalence of ACE among individuals reporting high use of alcohol or cannabis
The prevalence of each ACE is presented in Table 2 for men and women with “high use”, “high alcohol use”, and “high cannabis use”. In terms of “high use” and “high alcohol use” significantly more women than men reported six of the seven ACE investigated. For “high cannabis use” significantly more women than men reported five of the seven ACE investigated. A difference between sexes for physical abuse was not found.
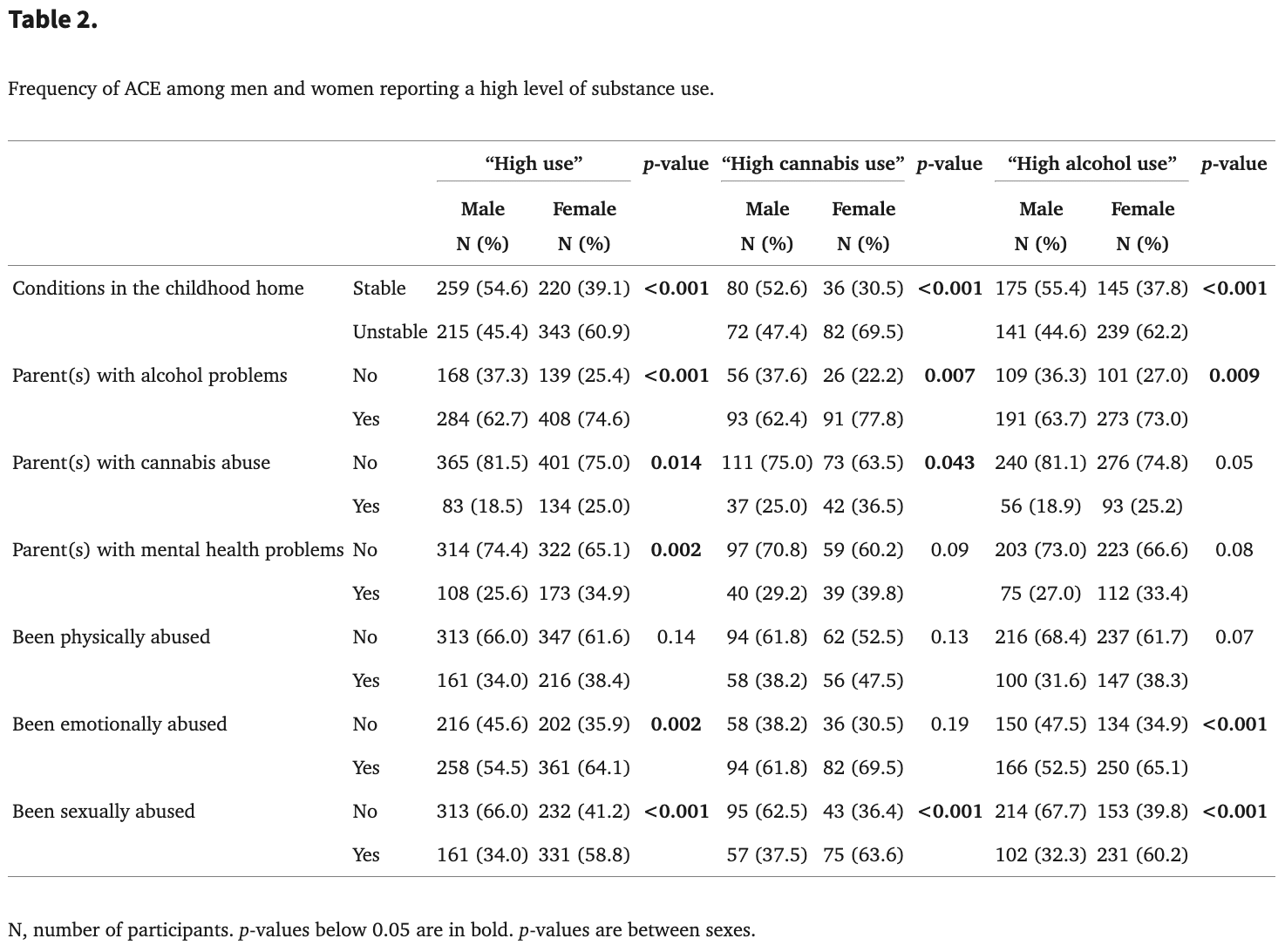
For “high cannabis use”, a significant difference between men and women regarding ACE was found for all ACE except physical abuse and having had parent(s) with mental health problems. More women with “high cannabis use” reported unstable conditions in childhood (69.5% of women and 44.6% of men) (p < 0.001), parent(s) with alcohol use (73% of women and 63.7% of men) (p = 0.007), and having been sexually abused (63.9% in women and 37.5% in men) (p < 0.001).
In relation to “high alcohol use”, a significant difference between men and women regarding ACE was found for all ACE except for physical abuse (p = 0.068), parent(s) with mental health problems (p = 0.084), and parent(s) with excessive cannabis use (p = 0.053).
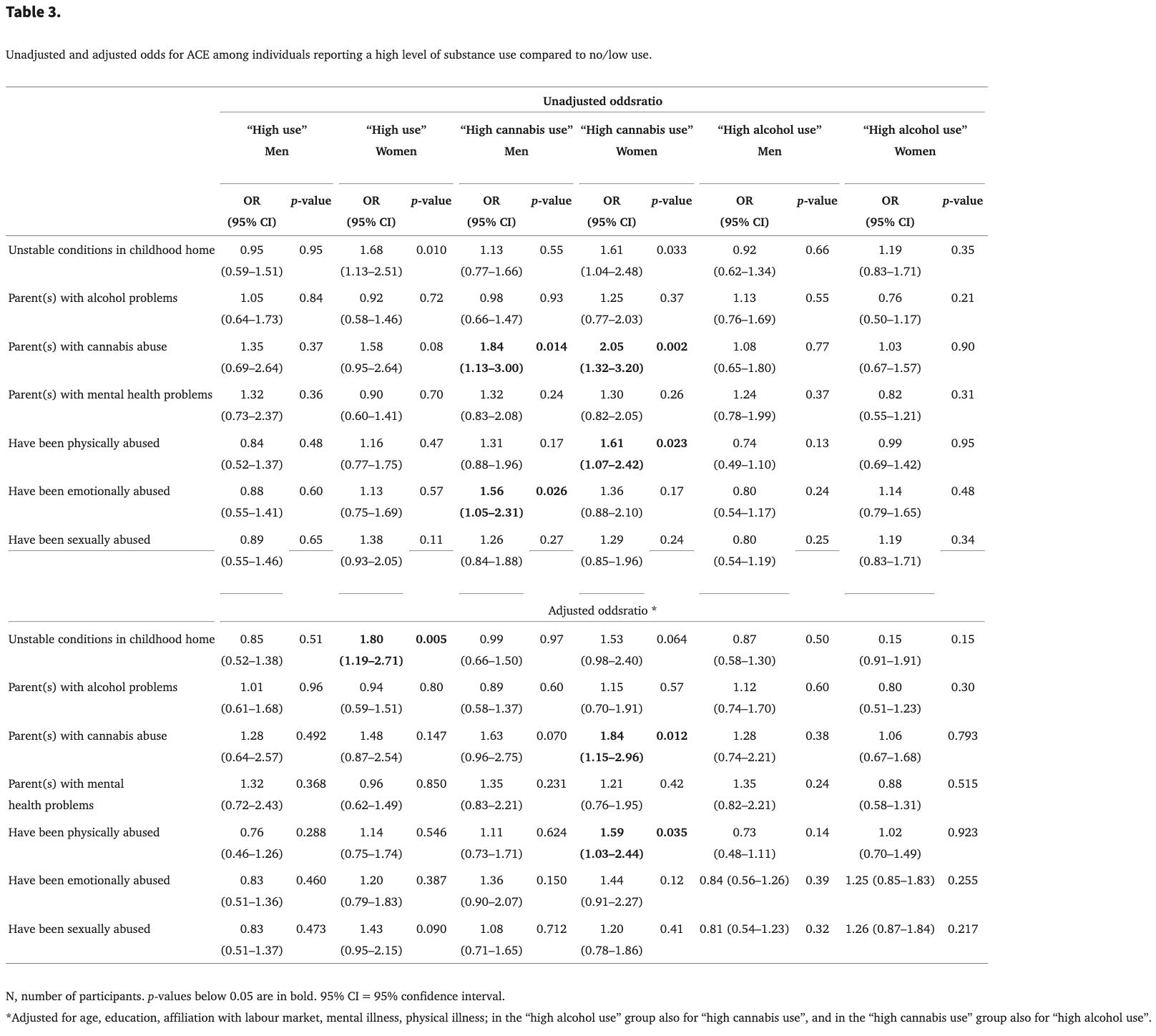
Unadjusted and adjusted ORs for ACE among individuals with high use of alcohol or cannabis
The relationship between “high use”, “high alcohol use” and “high cannabis use” and ACE categories is seen in Table 3 for men and women. Unstable conditions in the childhood home were associated with “high use” for women in both unadjusted (OR 1.68 [95% CI: 1.13–2.51], p = 0.01) and adjusted analysis (AOR 1.80 [95% CI: 1.19–2.71], p = 0.005). “high cannabis use” among women was significantly associated with three ACE categories in unadjusted analysis: having parent(s) with excessive cannabis use (OR 2.05 [95% CI: 1.32–3.20], p = 0.002), being physically abused (OR 1.61 [95% CI: 1.07–2.42], p = 0.023), and experiencing unstable conditions in childhood (OR 1.61 [95% CI: 1.04–2.48], p = 0.033). In adjusted analysis, significant associations were observed only for having parent(s) with excessive cannabis use (AOR 1.84 [95% CI: 1.15–2.96], p = 0.012) and for being physically abused (AOR 1.59 [95% CI: 1.03–2.44], p = 0.035). For men, “high cannabis use” was significant associated with having parent(s) with excessive cannabis use (OR 1.84 [95% CI: 1.13–3.00], p = 0.014) and for being emotionally abused (OR 1.56 [95% CI: 1.05–2.31], p = 0.026) in unadjusted models although no associations were found in adjusted analysis. For either men or women, no associations were detected between ACE categories and “high alcohol use” in unadjusted or adjusted analysis.
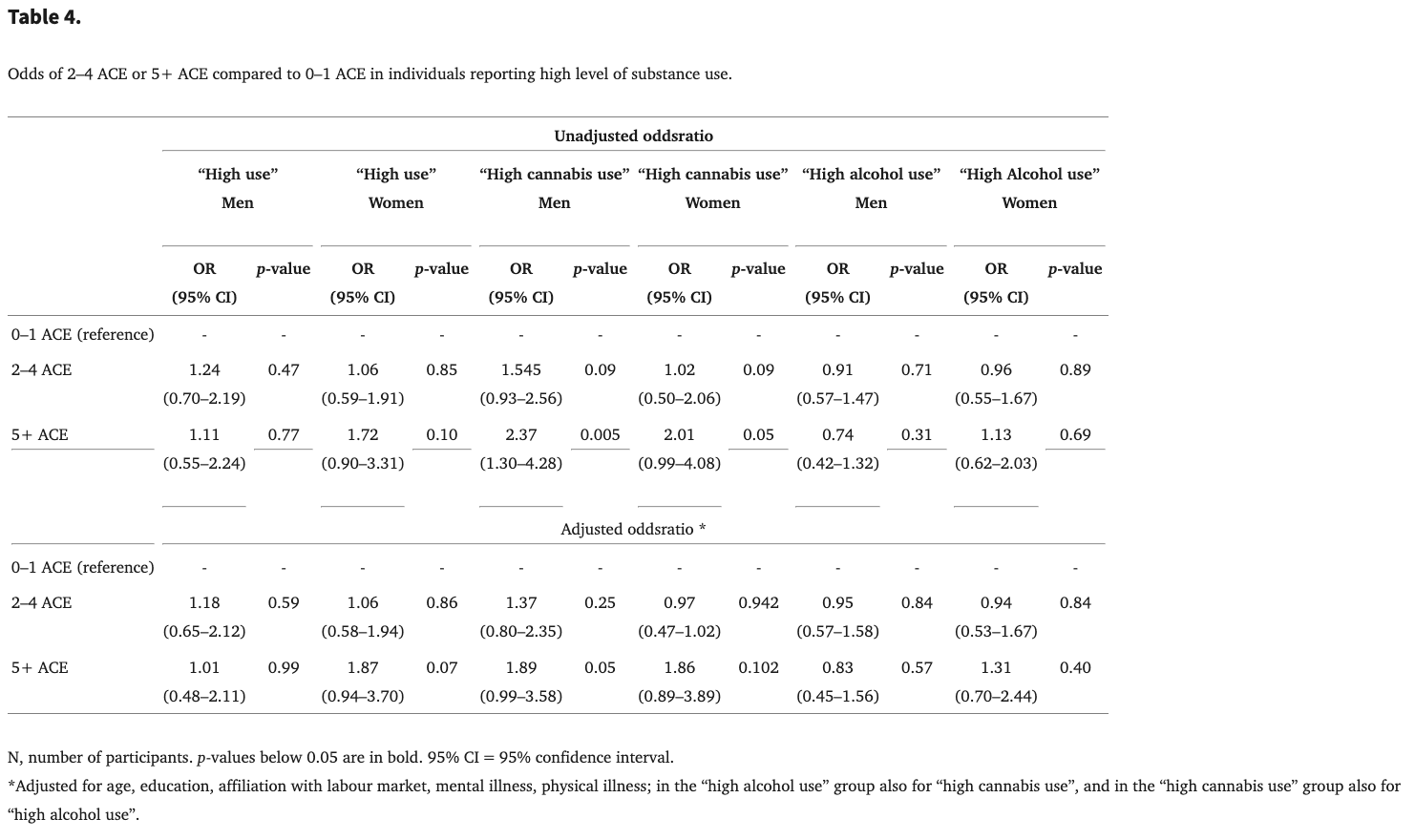
Association between type of use and number of ACE
Table 4 illustrates the association between the different categories of high use and the frequency of ACE. For both sexes, no association in the unadjusted or adjusted analysis for either “high use” or “high alcohol use” and the number of ACE was found. “High cannabis use” was associated with having experienced five or more ACE for men (OR 2.37 [95% CI: 1.30–4.28], p = 0.005) in the unadjusted analysis. However, in the adjusted analysis no association was found (AOR 1.89 [95% CI: 0.99–3.58], p = 0.05). For women, no association between ACE and “high cannabis use” was found.
Discussion
The majority of individuals seeking treatment for SUD in Greenland reported experiencing more than one of the seven ACE examined. Approximately half of the study sample experienced between 2 and 4 ACE, while 34% of women and 21% of men reported experiencing between 5 and 7 ACE. Only 15% of women and 30% of men reported having experienced none or just one ACE. Growing up with parents with alcohol problems was the most common individual ACE and was reported by about two-thirds of both sexes. The second frequently experienced ACE was emotional abuse, followed by unstable childhood conditions. The high proportion of individuals who have experienced the three most common ACE suggests an association between ACE and SUD among Greenland’s population.
Women reported having experienced six of the seven ACE more frequently than men did, with physical abuse being the only exception. The higher prevalence of ACE among women compared to men is consistent with findings from other studies. The most significant difference between the sexes was observed in relation to sexual abuse, which was reported by twice as many women as men (Table 2). The higher prevalence of ACE in women might be explained by the higher rate of sexual abuse. Additionally, the latest national population health survey from 2018 found that more young women than men are heavy alcohol users and that more women than men seek treatment for SUD. A study among Canadian Aboriginals found that women who reported more ACE simultaneously reported more unhealthy clinical symptoms, such as depression, suggesting more extensive health evaluation may be necessary for women in SUD treatment. The high prevalence of ACE among treatment seekers, particularly women, underlines the necessity for focused early interventions within families experiencing challenges due to SUD. Preventing children’s exposure to ACE is crucial for improving individual health, public health, and societal well-being.
ACE have in other studies been found highly interrelated, and a cumulative effect has been revealed. Despite most individuals in treatment reporting more than one ACE, no cumulative effects between the number of ACE experienced and high use of alcohol or cannabis were observed for either sex. The association was non-significant for “high use” and “high alcohol use” in both the unadjusted and adjusted models. However, unadjusted analysis between “high cannabis use” and having experienced five or more ACE was significant for men with OR 2.37 (95% CI: 1.30–4.28, p = 0.005) and appear to be approaching significance for women, with OR 2.01 (95% CI: 0.99–4.08, p = 0.05). In adjusted analysis, the association was not significant for women and for men the association changed from significant to approaching significance with an AOR 1.89 (95% CI: 0.99–3.58, p = 0.05) (Table 4). This study suggested that there was an association, but the association cannot be demonstrated probably due to the small study sample. A larger study sample may be helpful in determining significance, especially for “high cannabis use”.
Our findings indicate some alignment with the hypothesis that cannabis may be preferred over alcohol among individuals with a history of ACE. In the adjusted model, women who experienced physical abuse (AOR 1.59 [95% CI: 1.03–2.44], p = 0.035) or who had parent(s) with excessive cannabis use (AOR 1.84 [95% CI 1.15–2.96], p = 0.012) were significantly associated with “high cannabis use”. Other research has affirmed that physical abuse is a strong predictor of SUD among both sexes. Although sexual abuse is widely recognised as one of the strongest predictors of later SUD, no associations were found between experiencing sexual abuse and the three categories of high use in this study (Table 3).
The pervasive and disruptive effects of growing up in a home affected by AUD are well documented in Greenland; however, less is known and understood about the consequences of the high general consumption of cannabis within the population. Experiences of ACE, especially sexual abuse, are closely associated with mental health issues both within the general population and among those seeking SUD treatment. In Greenland, a cultural transition from a traditional hunting lifestyle to a Western social structure, combined with historical issues such as widespread alcohol consumption during the 1970s and 1980s, has resulted in intergenerational trauma and ACE that are closely intertwined. Data from the National Public Health Survey in 2018 also indicate that young individuals who have experienced ACE demonstrate significantly poorer mental health outcomes compared to their peers who have strong ties to Inuit culture and have not experienced ACE.
Strengths and limitations
The literature describes a range of items and questionnaires for measuring ACE. This study included seven ACE categories, whereas other studies have explored ten or more different ACE. A systematic review identified physical abuse, emotional abuse, sexual abuse, household mental illness, and household SUD as the most studied ACE items. All of these are included in this study though an additional important ACE – to have witnessed physical violence at home – was not. Our measure of stability in the home aims to partially capture this category.
A critical limitation of the study lies in the reliance on self-reported data for both exposure and outcome measures, which increases the risk of recall bias. Research suggests that recall bias often results in the underreporting of ACE, and thus the associations observed in the study may be underestimated. The fact that the individuals completed the questionnaire alongside a therapist may have reduced the likelihood of misclassification. Given the cross-sectional design of the study, it is not possible to infer causal relationships between ACE and substance use. Additionally, selection bias may have occurred in terms of both exposure and outcomes, as those who do not seek treatment may have experienced a higher prevalence of ACE compared to those who do seek treatment.
A strength of this study is the inclusion of all citizens in Greenland receiving SUD treatment during the study period and the relatively low rate of exclusions. Another significant advantage is the use of the AUDIT questionnaire, which is widely recognised for identifying AUD and has been deemed reliable within the Greenlandic treatment context even though it has not undergone rigorous scientific evaluation. Moreover, the AUDIT questionnaire takes into account the social harm caused by drinking behaviours. The study’s measurement of the ACE items, however, does not provide insights into the frequency or severity of the ACE. The association between ACE and substance use, however, is inherently difficult to assess due to challenges associated with recall and ethical considerations. Nevertheless, this study’s ability to examine the cumulative effects of various traumatic childhood experiences represents a notable strength, as previous studies have indicated that these experiences are closely related to SUD.
Conclusion
This study shows a significant association between ACE and substance use among the Greenlandic population seeking treatment for SUD, thereby corroborating findings from other studies. Although no cumulative effect of experiencing ACE on “high alcohol use” was observed, the study suggests an association between having experienced five or more ACE and “high cannabis use”, but this needs to be investigated in future studies with a larger sample size. Growing up with parents with alcohol problems was the most frequently reported ACE for both sexes.
Ethics approval
The study was approved by the National Ethical Committee for Scientific Research in Greenland (ref. no. 2024–17590). The data used are from a register survey. The National Ethical Committee for Scientific Research in Greenland approved that data were analysed with the aim of evaluating problems that may stand in the way of treatment, and which may therefore provide the opportunity for further differentiation of the treatment offered to the target group. Person-sensitive data were handled in accordance with the Data Protection Act for Greenland, and each informant was assigned a unique identification number.