Abstract
Untreated addiction is often associated with criminal justice involvement. Pre-arrest diversion programs are increasingly popular, despite limited evidence. We implemented Madison Addiction Recovery Initiative (MARI), a law enforcement-led diversion-to-treatment program, for adults with eligible, drug use-related crime, and evaluated MARI’s impact on health outcomes. One-hundred-sixty participants completed clinical assessments at baseline, with 100 completing the six-month program (“Completers”) and clinical assessments, and 60 not completing the program (“Non-Completers”). One-way ANOVA and chi-square tests compared baseline characteristics between Completers and Non-Completers, with differing characteristics entered into a logistic regression model assessing the baseline predictors of program completion. At baseline, 75.0% reported opioid use, and 34.9% were involved in addiction treatment. Compared to baseline, Completers reduced depression, anxiety, and addiction severity scores, and increased their rate of treatment with medications for opioid use disorder (p < 0.001). Significant predictors of program completion (p < 0.05) included treatment engagement, and higher depression and lower anxiety symptom scores at baseline, fewer incarceration episodes within 12 months pre-enrollment, and shorter “lifetime” maximum sobriety duration. These findings suggest pre-arrest diversion programs can effectively connect adults who committed drug-use related crimes to addiction treatment, and improve health outcomes among engaged participants.
Background
In the U.S., nearly 85% of incarcerated people have a substance use disorder (SUD) or are incarcerated for a drug use-related crime (NIDA, 2020). Without treatment, people with SUD are at an increased risk of crime recidivism and overdose death following incarceration. The risk of dying from an overdose can be 12.7 times higher in the first two weeks after a release from prison compared to the general population (Binswanger et al., 2013). Those arrested or in contact with the police for a drug use-related crime are also more likely to be arrested again and incarcerated for longer periods in the future in the absence of SUD treatment (Zhang et al., 2022). On the other hand, addiction treatment has documented benefits for reducing both crime recidivism and overdose fatalities (Wakeman & Rich, 2015). For incarcerated people with an opioid use disorder (OUD), treatment with medications for addiction (MAT) can reduce post-release mortality by 60% to 85% (Green et al., 2018; Marsden et al., 2017).
Evidence shows a high burden of SUD among persons interacting with the criminal justice system and underscores the importance of facilitating SUD treatment during contact with law enforcement or the criminal justice system. As a result, there is a growing movement to implement interventions that are alternatives to incarceration to improve outcomes. In 2022, a Stanford-Lancet Commission on the North American Opioid Crisis recommended avoiding incarceration for possession of drug use-related equipment or illicit opioids for personal use as a means of minimizing SUD-related harms (Humphreys et al., 2022). Strategies such as depenalization and/or decriminalization of drug use (Bratberg et al., 2023; Russoniello et al., 2023), post-overdose outreach programs (Formica et al., 2018), law enforcement-led treatment referrals (Donnelly et al., 2023; Schiff et al., 2017) or pre-arrest diversion-to-treatment programs (Bureau of Justice Assistance, 2021) have been implemented as alternatives to incarceration for drug use-related crimes. However, the existing alternative approaches have applied heterogeneous eligibility criteria and methods, and little is known about their effectiveness and who is most likely to successfully complete and benefit from these programs.
Pre-arrest diversion programs are usually led by law enforcement and strive to “divert” individuals with SUD to addiction treatment. Early evaluation outcomes from pre-arrest diversion programs have been promising with respect to reducing crime recidivism. The Law Enforcement Assisted Diversion (LEAD) program in Seattle, Washington diverted eligible individuals to case management and community-based treatment services in lieu of arrest and prosecution, and found that program participants had lower odds of being arrested or charged with a felony both at 6 months and a 2-year follow-up after program enrollment (Collins et al., 2017); of note, treatment engagement was neither required nor incentivized by the LEAD program. Other programs reported similar outcomes, with reduced crime recidivism after program completion (McSweeney et al., 2016). Although diversion programs have shown benefits for reducing crime recidivism and hold promise for improving health-related outcomes, research addressing clinical outcomes and the impact of pre-arrest diversion programs on these outcomes is sparse. One model found that diversion programs could improve quality of life and quality-adjusted life years, reduce fatal overdoses, and provide overall benefits to health systems (Bernard et al., 2020).
The Madison Addiction Recovery Initiative (MARI) is an example of a law enforcement-led, pre-arrest diversion program implemented and evaluated in Madison, Wisconsin, USA from 2017 to 2022 (Zgierska et al., 2021). MARI was offered by the police officers to adults who committed a non-violent, drug use-related eligible crime in lieu of arrest and prosecution, which, at the time, constituted the “standard” pathway for individuals with drug use-related crime. MARI, developed with input and involvement of key community partners (Zgierska et al., 2021; Zhang et al., 2024), consisted of 6 months of active monitoring, followed by additional 6 months of “passive” follow-up. Eligible adults who consented to participate in MARI were enrolled into the program “at the point of crime” by police officers and referred for a clinical assessment to a partnering addiction treatment program; their criminal charges were held in abeyance. Following the standardized clinical assessment, MARI participants were referred to individually-tailored addiction treatment, and offered peer recovery support. Participants were closely followed up regarding their treatment engagement and new crime events during the six-month program. Upon successful completion of MARI’s six-months of active monitoring, participants had their initial charges “voided,” allowing the program completers to have a criminal background untarnished by the crime that brought them to MARI. Those who had enrolled in MARI but did not complete the six-month program (e.g., due to treatment disengagement or crime recidivism) had their initial criminal charges referred for prosecution. After the active six months of MARI programming, participants’ crime and arrest outcomes were “passively” tracked for additional six months, so the entire follow-up spanned 12 months after MARI enrollment. The evaluation of crime and overdose death events showed that MARI completers (N = 100) were less likely to be arrested or incarcerated, and had lower rates of overdose deaths at 6 and 12 months post-enrollment compared to those who did not engage at all (N = 103) or started but did not complete the six-month program (N = 60) (Nyland et al., 2024; White et al., 2021).
Given gaps in the current understanding of pre-arrest diversion programs’ impact on health-related outcomes and who might benefit most from these programs, we evaluated (1) clinical profile of the MARI participants upon their program entry; (2) program participation impact on clinical outcomes among the program completers; and (3) participants’ baseline characteristics as potential predictors of successful program completion.
Methods
Program Details and Study Design
MARI’s protocol (Zgierska et al., 2021) and implementation details (Zhang et al., 2024) are described elsewhere. The crime and overdose death-related MARI outcomes were also published (Nyland et al., 2024; White et al., 2021).
Briefly, the aim of MARI as a pre-arrest diversion program was to reduce crime recidivism and fatal overdoses in Madison, a medium-sized city in Wisconsin, U.S., by offering addiction treatment in lieu of arrest and prosecution to adults who committed an eligible, drug use-related crime. MARI was implemented as a city-wide “quality improvement” initiative and involved all Madison Police Department (MPD) districts and police officers. Its implementation was led by the MPD, in partnership with community, public health, and academic partners, and local leaders, including the Mayor, District and City Attorneys, the Sheriff, and the Wisconsin Department of Health Services. The University of Wisconsin-Madison Institutional Review Board deemed this project as not constituting human subjects research, as defined under 45 CFR 46.102(d).
Planning for MARI started in 2015, with grant funding secured in 2016 from U.S. Department of Justice Bureau of Justice Assistance under the Smart Policing Initiatives program. Participant enrollment started on September 1, 2017 and ended on August 31, 2020. At the time, the standard law enforcement protocol included arrest, prosecution and potential incarceration for drug use-related offenses when there was probable cause for arrest. Under MARI, adults apprehended by MPD officers for an eligible crime (e.g., possession of drugs or drug paraphernalia for personal use; burglary, retail, or auto theft related to drug use) were invited to participate in the six-month MARI program instead of the traditional law enforcement pathway. All MPD commissioned officers were trained in the MARI approach so that they could determine MARI’s eligibility and offer the program participation “at the point of crime” to eligible adults. Regular monitoring by the MARI team aimed at ensuring fidelity to the program’s approach, and equity and fairness for potential participants to access the program (Zhang et al., 2024).
Individuals who enrolled in MARI were asked to contact the MARI’s Assessment Hub, a partnering local addiction treatment program, within 72 h of enrollment to get connected to recovery peer support and schedule their clinical assessment. The clinical assessment, completed by the Hub’s clinical team, evaluated the scope and severity of SUD, co-occurring conditions, and relapse risk, allowing for individualized determination of the needed level of addiction care (Gastfriend & Mee-Lee, 2004). Participants were then provided a “warm handoff” to individually-tailored treatment, and assisted with any health insurance coverage needs. Addiction treatment, guided by each participant’s clinician, could comprise different modalities, including MAT and behavioral care as well as case management. The Hub’s staff then monitored each participant’s treatment engagement by staying in touch with each participant’s clinician to answer a “Yes/No” question on participant treatment engagement; of note, relapse to substance use per sewas not grounds for dismissal from the program. The MPD staff also monitored for any new criminal activity recorded in the MPD’s database or incarceration in the local county jail. Participants who stayed engaged in treatment and did not reoffend during the six-month program were considered program Completers and had their criminal charges (that brought them to MARI) “voided.” Those who had initiated but did not complete the program due to lack of treatment engagement or crime recidivism were considered program Non-Completers; Non-Completers were directed to the District or City Attorney’s offices for prosecution. The crime/arrest, incarceration and fatal overdose data were available for all participants throughout the six-month MARI and then during the additional six months of follow-up. Completers and Non-Completers both completed the clinical assessment at baseline;only Completers provided clinical data at 6 months post-enrollment.
The MARI team, comprising police and clinical Hub representatives, met at least weekly during the program to monitor progress among participants and troubleshoot any problems, including difficulties with participant engagement. To facilitate participation, MARI implemented several approaches. The Hub’s staff strived to reach participants who had not initiated the contact. Participants were offered bus passes and cell phones with paid plans for those with transportation or phone-contact barriers to participation. The Mobile Outreach Team was created to conduct in-person follow-up with participants who failed to connect with the Assessment Hub (Zhang et al., 2024).
Participant Eligibility
Eligible individuals met the following criteria: 1) were apprehended by an MPD officer for an eligible, drug use-related crime between September 1, 2017 and August 31, 2020; 2) were at least 18 years old; and 3) lived in Dane County. The eligible crimes included non-violent drug use-related crimes: possession of drugs or drug paraphernalia for personal use; prostitution, retail theft, or auto theft; or burglary, or theft where family members were the victims. Exclusion criteria included: presence of an active arrest warrant; being on parole or probation; a history of violent felony conviction in the past 3 years; being registered as a sex offender; or presenting a danger to the program staff.
Outcome Measures
The outcome measures assessed the scope and severity of SUD and related problems, with a focus on mental health conditions, as evaluated with the American Society of Addiction Medicine (ASAM) Placement Criteria (Gastfriend & Mee-Lee, 2004) and the Brief Addiction Monitor (BAM) questionnaire (Cacciola et al., 2013). The ASAM Placement Criteria assess the SUD severity and risk for relapse across six domains: 1) acute intoxication and/or potential for withdrawal; 2) co-occurring biomedical conditions and complications; 3) co-occurring emotional, behavioral, cognitive conditions and complications; 4) readiness to change; 5) potential for relapse, continued use or problems; and 6) recovery/living environment (Gastfriend & Mee-Lee, 2004). Information gathered through the ASAM Placement Criteria is routinely used in clinical settings to determine the optimal level of SUD care for individuals. Variables derived from the ASAM Placement Criteria for the analysis included: the presence of intoxication or withdrawal at the time of assessment; access to routine medical care; acknowledged problematic substance use; prior attempts at recovery; maximum sobriety duration; awareness of relapse triggers; presence of relapse prevention coping skills; family and/or roommate support for recovery; housing availability; and financial security/employment. All variables were structured as “yes/no” responses and applied to the current status, except maximum sobriety duration, which was defined as the number of years during a lifetime. The BAM questionnaire includes 17 items comprising three domains: 1) extent of substance use (score range: 0-12; score ≥1 indicates substance use, and higher scores indicate more extensive use); 2) risk factors for relapse, continued drug use, or worsening addiction (score range: 0-24; score ≥12 indicates increased risk); and 3) protective factors that facilitate initiation and maintenance of recovery (score range: 0-24; score ≥12 indicates better protection against relapse) (Cacciola et al., 2013). Mental health was assessed with the nine-item Patient Health Questionnaire (PHQ-9) for severity of depression symptoms (Kroenke et al., 2001), and the seven-item Generalized Anxiety Disorder (GAD-7) questionnaire for severity of anxiety symptoms (Spitzer et al., 2006). Each item on the PHQ-9 and GAD-7 is scored from 0-3 (0 = no symptoms), with a maximum score of 27 on the PHQ-9 and 21 on the GAD-7. Higher PHQ-9 or GAD-7 scores indicate higher symptom severity, and scores ≥10 represent a “positive” screen for depression and anxiety, respectively.
Following the Hub’s routine clinical assessment approach, participants were also asked to name their primary and secondary substances used; whether they had received an addiction treatment (“yes/no” to past and current treatment) or MAT (“yes/no” to current MAT; type of MAT); and their overdose history (“yes/no”; and total number of prior overdose events).
Demographics and baseline arrest and incarceration (past 12 months) data were available for all participants from the MPD’s database.
Statistical Analysis
Descriptive statistics were used for sample characterization at baseline (Completers and Non-Completers) and follow-up (Completers only). One-way ANOVA and chi-square analyses were used for continuous and categorical data, respectively, for between-group comparisons at baseline. Paired t-tests and paired samples proportions tests were used to compare pre-post program changes among Completers. Logistic regression, which incorporated relevant baseline characteristics that differed between the Completer and Non-Completer groups and sex (binary variable: male versus female), was used to identify potential predictors of the six-month program completion. Statistical significance level was set at a two-tailed p < 0.05. The IBM SPSS Statistics (Version 28) software was used for statistical analysis.
Results
Among 263 MARI participants, 160 completed the clinical assessment at baseline and formed the study sample. By the end of the MARI six-month program, these 160 participants formed two groups: Completers (N = 100) and Non-Completers (N = 60). The reasons for program non-completion during the six months of post-enrollment follow-up included: lack of treatment engagement (N = 52), crime recidivism (N = 6); and a fatal overdose (N = 2).
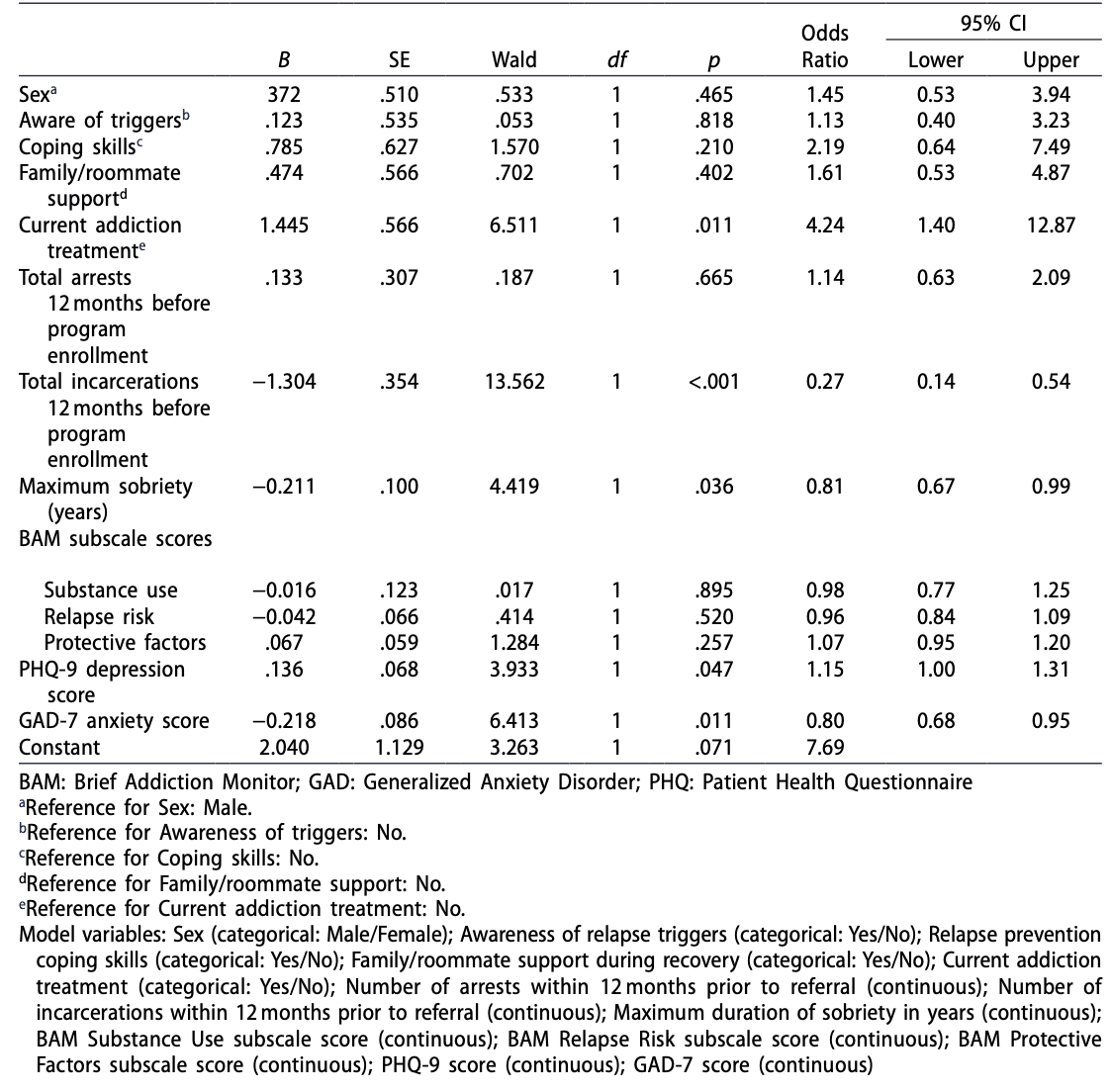
Baseline Characteristics (Table 1)
Among 160 participants, the majority identified as male (68.1%), white (80.6%), and residing in Madison, WI (68.1%). They were, on average, 34.3 (SD 10.2) years old. One-half of the participants (50.6%) were unemployed and 5.6% reported a lack of residence. These demographic characteristics did not statistically differ between the Completer and Non-Completer groups.
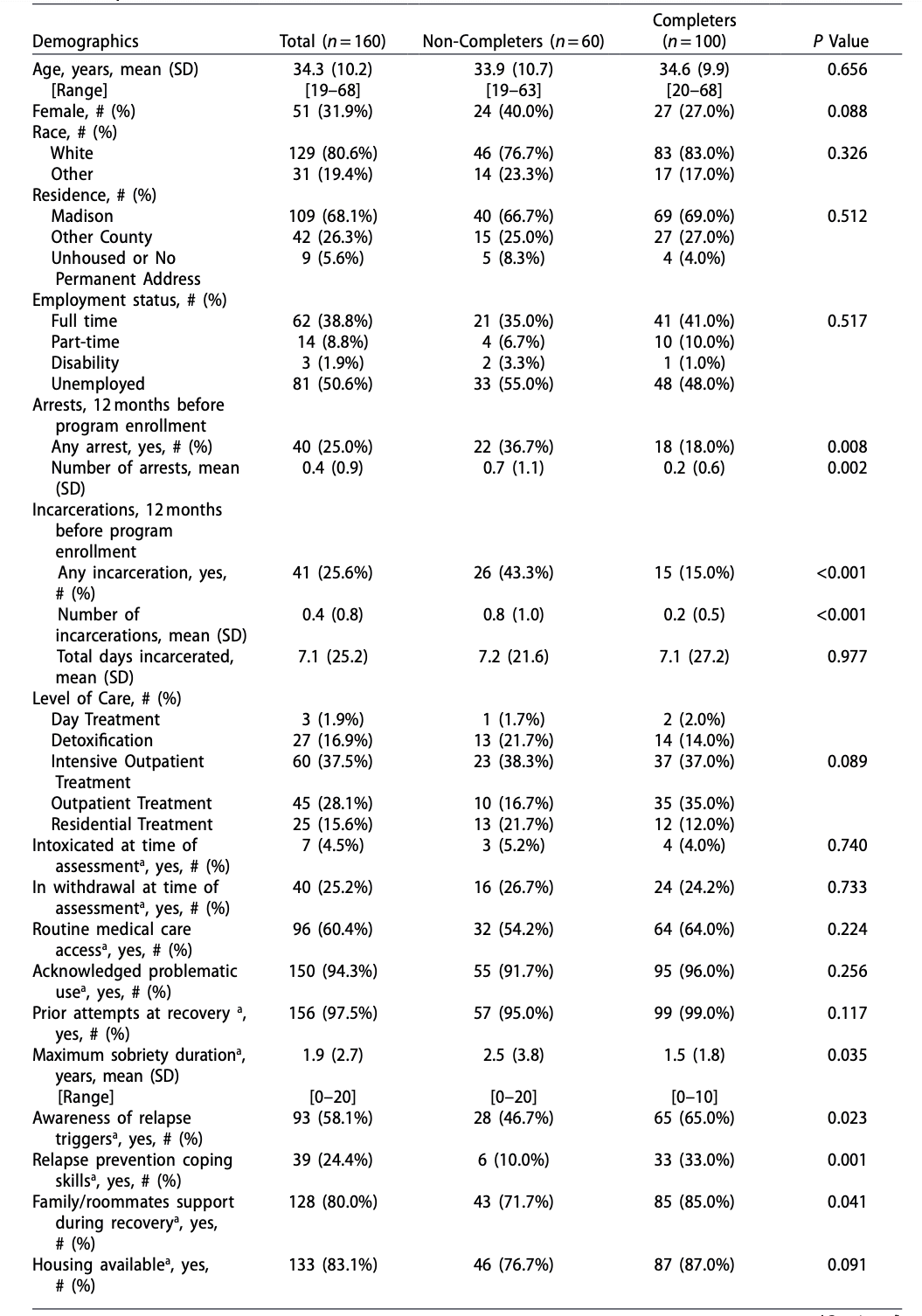
During 12 months pre-enrollment, approximately one-quarter of the sample had been arrested (25.0%) or incarcerated (25.6%). Completers, compared to Non-Completers, were less likely to have a history of an arrest (18.0% vs 36.7%, respectively, p = 0.008) or incarceration (15.0% vs 43.3%, respectively, p < 0.001), and had a lower number of arrest (p = 0.002) and incarceration (p < 0.001) episodes; the groups did not significantly differ in the total number of days spent incarcerated.
At baseline, 25.2% of participants were in acute withdrawal and 4.5% displayed signs of intoxication. Over one-half reported having access to routine medical care (60.4%) and financial support/employment (53.1%), with most reporting having family/roommate support (80.0%) and housing available (83.1%). Opioids were the primary reported substance used (75.0%), with cannabis being the most common secondary substance (28.3%). The majority acknowledged problematic substance use (94.3%), prior attempts at recovery (97.5%), and past involvement with addiction treatment (86.1%), with a maximum prior sobriety duration of 1.9 (SD 2.7) years, on average. Although 34.9% reported involvement in some form of addiction treatment upon enrollment, only 13.8% reported treatment with MAT for OUD. The majority reported at least one overdose in their lifetime (81.6%), averaging 2.9 (SD 3.2) overdose episodes. Based on the clinical assessment and the ASAM Placement Criteria, the majority (N = 105) were recommended outpatient treatment (37.5% intensive, 28.1% less-intensive outpatient treatment). Completers, compared to Non-Completers, reported a shorter maximum duration of prior sobriety (p = 0.035), and better family/roommate support (85.0% vs. 71.7%, respectively, p = 0.041), presence of relapse prevention coping skills (33.0% vs. 10.0%, respectively, p = 0.001), and awareness of relapse triggers (65.0% vs. 46.7%, respectively, p = 0.023), and were more likely to be receiving addiction treatment at baseline (41.8% vs. 24.1%, respectively, p = 0.028).
The BAM’s scores across the three domains indicated the presence of substance use, increased relapse risk and reduced protection against relapse at baseline. Participants also had elevated depression and anxiety scores, with 35.1% screening positive for depression and 40.9% screening positive for anxiety. The baseline scores of depression, anxiety, and BAM’s substance use and relapse risk domains did not significantly differ between the Completer and Non-Completer groups. However, Completers scored higher (i.e., more favorably) than Non-Completers on recovery protective factors (p = 0.008).
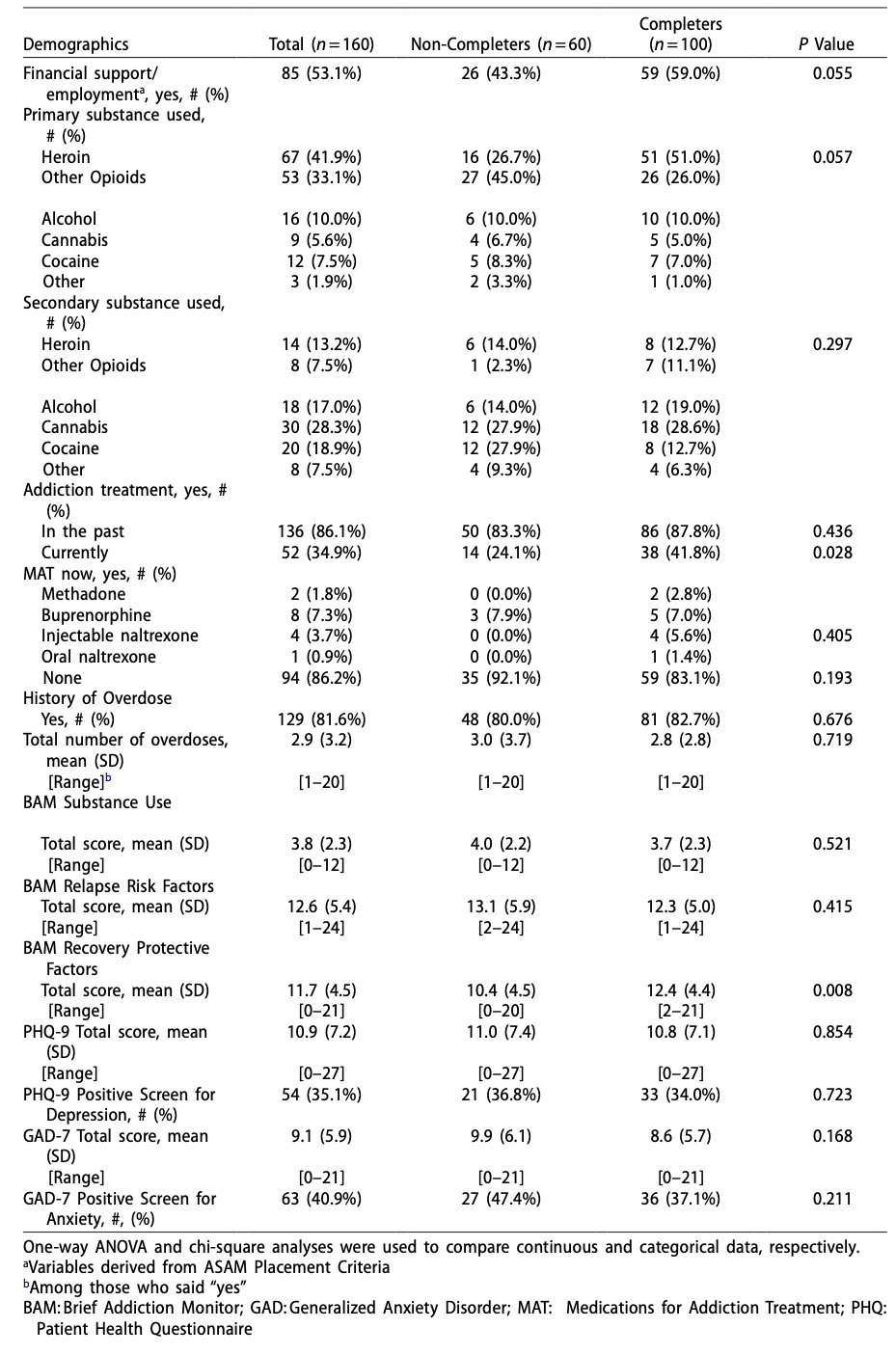
Change in Clinical Outcomes among Program Completers (Table 2)
Compared to baseline, at six months post-enrollment, the Completer group (N = 100) significantly reduced their depression and anxiety scores, with fewer participants screening positive for depression (34.0% vs 9.7%, respectively, p < 0.001) and anxiety (37.1% vs 17.2%, respectively, p < 0.001). The BAM scores of substance use and relapse risk domains also significantly decreased, while the scores of recovery protective factors increased, indicating a positive change. The frequency of treatment with MAT increased at follow-up compared to baseline (p < 0.001), with the majority reporting MAT at 2 months (87.9%) and 6 months (56.8%) post-enrollment.
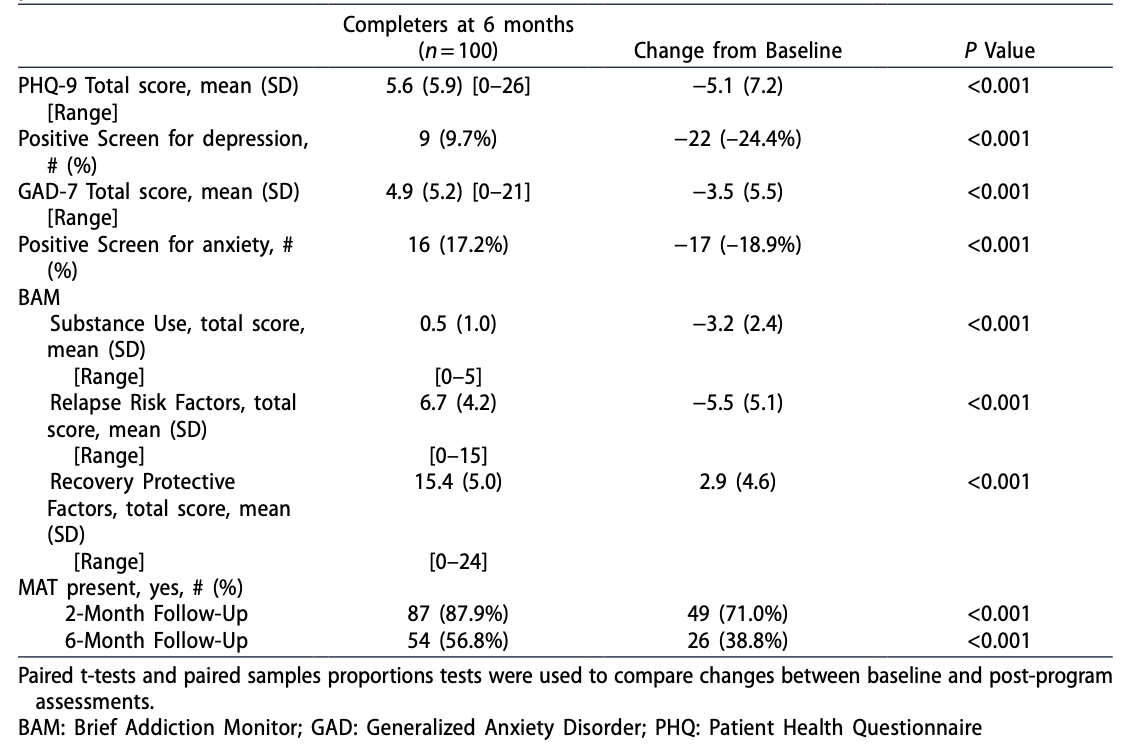
Baseline Predictors of Program Completion (Table 3)
The logistic regression model included sex, additional variables that significantly differed between the Completer and Non-Completer groups (number of arrests and incarceration episodes prior to enrollment; maximum lifetime sobriety duration; awareness of relapse triggers; presence of relapse prevention coping skills; family/roommate support; and current addiction treatment), and BAM, PHQ-9 and GAD-7 scores collected at baseline. The model was statistically significant (χ2(12) = 51.7, p < 0.001), explained 44.0% of the variance in program completion, and correctly classified 75.0% of cases, with 60.8% sensitivity, 84.0% specificity, positive predictive value of 77.3%, and negative predictive value of 70.5%.
The logistic regression analysis, with Non-Completers as a reference group, identified five statistically significant variables: currently receiving addiction treatment (OR = 4.24, 95% CI [1.40, 12.87]), number of pre-enrollment incarceration episodes (OR = 0.27, 95% CI [0.14, 0.54]), maximum lifetime duration of sobriety (OR = 0.81, 95% CI [0.67, 0.99]), and depression (OR = 1.15, 95% CI [1.00, 1.31]) and anxiety (OR = 0.80, 95% CI [0.68, 0.95]) symptom severity scores.
Discussion
The evaluation of a pragmatically-implemented, city-wide, law enforcement-led, pre-arrest diversion-to-treatment initiative suggests that this six-month program can be effective for some adults who committed drug use-related “minor” crime. MARI-facilitated linkages to addiction treatment, including MAT, likely led to reductions in mental health symptoms and relapse risk, thus increasing chances for successful SUD recovery. These health benefits paralleled the previously described reductions in crime recidivism, arrest, incarceration, and fatal overdoses through 12 months of follow-up (Nyland et al., 2024; White et al., 2021). In addition, our results indicated the odds of completing the MARI program improved with the baseline presence of addiction treatment and higher depression scores, and worsened with an increased number of prior incarceration episodes, higher anxiety scores, and a greater duration of prior sobriety.
Although approximately 25% of the MARI participants had been involved with the criminal justice system in the 12 months prior to their program enrollment, the Completers, compared to Non-Completers, had a less extensive history of prior arrests and incarceration, along with an overall more favorable profile of mental health and recovery-promoting “protective factors” (such as better social support, engagement in addiction treatment, and presence of relapse prevention-relevant skills). Interestingly, Completers and Non-Completers did not differ with respect to their self-reported access to routine medical care, or housing, financial and employment status. Ongoing support during one’s recovery, with special attention to these socioeconomic factors (e.g., housing stability, employment, etc.), is critical for the prevention of relapse and future involvement with the criminal justice system (Vail et al., 2021). Of note, during MARI’s implementation (Zhang et al., 2024), we employed deliberate efforts to recognize and address potential socioeconomic barriers to program participation and treatment engagement; these efforts included a Mobile Outreach Team to follow up in-person with non-engaged individuals by visiting them at their recorded residence, assistance with transportation difficulties, and cell phone plans for those without reliable telephone access. Given the early successes and lessons learned through MARI, the MPD subsequently applied these experiences to further build the program and create a more robust MARI outreach team tasked with engaging both those eligible for pre-arrest diversion and individuals who survived an overdose to help connect them to addiction treatment.
Our results offer support for MARI as an effective pre-arrest diversion program that could positively impact participants’ health and recovery outcomes. At the end of their six-month program, Completers reported significant reductions in mental health symptoms and relapse risk and increases in the recovery protective factors, with fewer screening positive for depression and anxiety compared to their baseline. Further, many were receiving MAT for OUD at the 2 and 6-month follow-up, which is important given that mental health conditions commonly co-occur with SUD (Jones & McCance-Katz, 2019) and have been linked to an increased risk of overdose among individuals with SUD (Campbell et al., 2018), and that MAT reduces the harms of OUD, including overdose mortality (Connery, 2015; Ma et al., 2019).
Our findings on the baseline predictors of program completion indicated that prior higher involvement with the criminal justice system, lack of treatment engagement at enrollment, and higher baseline severity of anxiety symptoms were associated with reduced likelihood of program completion. Thus, this particular iteration of the MARI program may be most helpful to individuals relatively naïve to the criminal justice system who have less severe anxiety symptoms and are already engaged in treatment, but had a setback in their recovery journey and committed a minor, drug use-related crime. The MARI program, by providing additional support and positive incentives (i.e., treatment instead of punishment), may have helped them continue along their path toward recovery. These findings align with those from other pre-arrest diversion programs. An evaluation of a pre-arrest diversion program in Florida found those with more severe behavioral health problems and higher severity of SUD at baseline were less likely to complete the outpatient-based diversion program (Kopak & Frost, 2017). Similarly, a systematic review of diversion programs for people with SUD found that those with more frequent drug use, lower educational level, and/or lack of social stability were less likely to benefit from diversion programs (Lindquist-Grantz et al., 2021). More intensive support in pre-arrest diversion programs or oversight provided by drug court-mandated treatment-based programs may be more beneficial for those with more severe SUD, more complex mental health problems, and higher relapse risk.
Interestingly, those with higher severity of depressive symptoms were more likely to complete the program while the inverse was found for anxiety symptoms. Anxiety and depression frequently co-occur with SUD and OUD (Langdon et al., 2019; Rogers et al., 2021; Tormohlen et al., 2021). However, their impact on treatment, co-morbid health conditions, and directionality of their associations remain nuanced. For example, one study found depressive symptoms were mostly related to opioid use during early treatment among those who used opioids to cope with their symptoms or had more risk-taking behaviors (Ellis et al., 2023). Another study found a greater association between treatment dropout and anxiety symptoms, while the opposite was found for depression symptoms (Benningfield et al., 2012). In addition, worsened anxiety-type symptoms may be caused by acute substance withdrawal, which, in turn, can increase the risk of relapse and may lead to program dropout (Baxley et al., 2019; Lejuez et al., 2008). Thus, while PHQ-9 and GAD-7 scores offer a snapshot of depressive and anxiety symptoms, additional research is needed to understand how mental health may interplay with pre-arrest diversion program completion. Trauma is another factor that can impact SUD-related outcomes (Hassan et al., 2017; Keyser-Marcus et al., 2015). MARI, relaying on the clinical evaluation routinely administered at the partnering treatment program, did not have information on trauma and its impact; future studies should incorporate trauma-based measurements.
Completers were more likely to have a lower baseline arrest and incarceration rates (12 months pre-enrollment) compared to Non-Completers, with fewer total incarcerations being predictive of MARI completion. While crime recidivism and incarceration outcomes were the focus of our other analyses (Nyland et al., 2024; White et al., 2021), it is important to consider who the optimal candidates are for pre-arrest diversion programs when implementing such programs in the community to ensure the “right” program is available for individuals with SUD. MARI differed from other pre-arrest diversion programs at the time in that it “voided” the individual’s criminal charge for a crime, which had brought them to the program. Given that Completers were less likely to have prior arrests or incarcerations than Non-Completers, voiding the criminal charge could have had a substantial and meaningful impact on their ability to have a “clean” criminal record, with significant downstream effects on their ability to find employment and housing, and participate in other social assistance programs (Lundgren et al., 2010).
Finally, our analyses suggested that a shorter duration of lifetime “maximum sobriety” period at enrollment was predictive of program completion. It may be that those with shorter prior sobriety duration had different internal motivations (i.e., more motivation given their relatively more recent relapse or setback in recovery) compared to those with longer prior duration, thus influencing their ability to complete the program. The duration of sobriety may have different meanings for individuals (Cyders et al., 2023); future mixed methods research may help elucidate motivations that can support completing a pre-arrest diversion program.
Limitations
MARI was a law enforcement-led program and had substantial support from the city and MPD. However, other communities may need additional buy-in from their police department and community to implement and sustain such a program. Many of the drug use-related crimes eligible for MARI enrollment were related to overdose, despite the eligibility criteria encompassing a wide variety of drug use-related crimes; thus, it is unknown whether our findings apply to individuals committing other minor drug use-related crimes. The program was conducted in a single, medium-sized city and limited diversity of our sample may limit the generalizability of our results to other locations and populations. The majority of participants were white, which may be in part reflective of the MARI’s exclusionary criteria, which did not allow enrollment of those who were on parole or probation; this also precluded our analysis by racial/ethnic minorities due to small sample size. Furthermore, we did not have data on sexual orientation or trauma experiences, which would be valuable in future analyses.
Future Steps
Our evaluation of Completers’ clinical outcomes was based on the measures used in routine clinical practice and focused on the scope and severity of SUD, its mental health comorbidities, and engagement in treatment. Future studies could examine additional comorbid conditions (e.g., other chronic conditions or human immunodeficiency or hepatitis C virus infections) as well as the impact on healthcare and other costs (Bernard et al., 2020) of pre-arrest diversion programs. Long-term follow-up evaluations could help determine the impact of such programs on an individual’s continued recovery trajectory and engagement with society (e.g., obtaining stable housing, employment, and necessary SUD services). Additional research is also needed to better understand predictors of completion of pre-arrest diversion programs with differing eligibility criteria and program requirements.
Conclusion
A law enforcement-led, pre-arrest diversion program may help those who committed a drug use-related minor crime engage in addiction treatment and improve their mental health and SUD outcomes. The MARI program, as implemented, may be most beneficial to those with less extensive past criminal history and lower relapse risk.