Abstract
Childhood psychotic-like experiences (PLEs) are associated with a range of impairments; a subset of children experiencing PLEs will develop psychiatric disorders, including psychotic disorders. A potential distinguishing factor between benign PLEs versus PLEs that are clinically relevant is whether PLEs are distressing and/or persistent. The current study used three waves of Adolescent Brain Cognitive DevelopmentSM (ABCD) study PLEs assessments to examine the extent to which persistent and/or distressing PLEs were associated with relevant baseline risk factors (e.g., cognition) and functioning/mental health service utilization domains. Four groups varying in PLE persistence and distress endorsement were created based on all available data in ABCD Release 3.0, with group membership not contingent on complete data: persistent distressing PLEs (n=272), transient distressing PLEs (n=298), persistent non-distressing PLEs (n=221), and transient non-distressing PLEs (n=536) groups. Using hierarchical linear models, results indicated youth with distressing PLEs, whether transient or persistent, showed delayed developmental milestones (β=0.074, 95%CI:0.013,0.134) and altered structural MRI metrics (β=−0.0525, 95%CI:−0.100,−0.005). Importantly, distress interacted with PLEs persistence for the domains of functioning/mental health service utilization (β=0.079, 95%CI:0.016,0.141), other reported psychopathology (β=0.101, 95%CI:0.030,0.170), cognition (β=−0.052, 95%CI:0.−0.099,−0.002), and environmental adversity (β=0.045, 95%CI:0.003,0.0.86; although no family history effects), with the interaction characterized by greatest impairment in the persistent distressing PLEs group. These results have implications for disentangling the importance of distress and persistence for PLEs with regards to impairments, including functional, pathophysiological, and environmental outcomes. These novel longitudinal data underscore that it is often only in the context of distress that persistent PLEs were related to impairments.
Psychotic-like experiences (PLEs), or psychosis spectrum symptoms (e.g., perceptual abnormalities, mild delusional thoughts), are relatively common in school-age children.1–3 PLEs in childhood are associated with a range of impairments, including cognitive and functioning impairments.2,4 PLEs experienced with distress may be potential targets of therapeutic intervention.5,6 Furthermore, a subset of these children endorsing PLEs are at risk for developing psychotic disorders or other psychiatric disorders in adulthood.7,8Building upon clinical high-risk research examining factors distinguishing those that develop psychosis,9,10research has begun to examine factors distinguishing more benign PLEs versus those that may portend greater impairment and perhaps even transition to psychotic disorders, including whether they are persistent over years or distressing.11–13 Most studies examine cross-sectional estimates of PLEs, although research has examined persistence of PLEs.12,14–23 Previous research indicates that persistent PLEs are associated with subsequent onset of psychotic disorders.11,19 The level of distress elicited by PLEs may also distinguish clinically-relevant PLEs,13,24–27 including predicting transition from clinical high-risk to psychotic disorders.28 However, no studies have specifically worked to disentangle correlates of persistent and distressing PLEs, which is the goal of the current study using prospective longitudinal data.
PLEs are thought to arise due to a combination of genetic, environmental, and pathophysiological factors (e.g., disruptions in connectivity).29,30 Several large cross-sectional datasets over the past two decades have examined the correlates of PLEs, finding associations with other symptoms (e.g., internalizing, externalizing),31 developmental impairments (e.g., motor milestone delays),32 and cognitive impairments33(e.g., reading,34 working memory,35 processing speed36). Of studies examining trajectories of PLEs, individuals with persistent PLEs tended to score higher on internalizing and externalizing symptoms,19adverse childhood experiences (ACEs),21,22 developmental delays, 22 as well as functional impairments and treatment seeking.11
The Adolescent Brain Cognitive Development℠ (ABCD) Study has found associations between cross-sectional estimates of distressing PLEs and a range of risk factor domains for psychopathology such as psychosis, including family history, other symptoms (e.g., internalizing, externalizing), environmental adversity (e.g., ACEs, exposure to deprivation), cognitive impairments, developmental delays, resting-state functional connectivity (RSFC) impairments, and global structural MRI impairments.37–40 However, previous work has not examined the extent to which both persistence and distressing factors, or the interaction of the two factors, are associated with impairment across these key correlates, symptoms, and functioning/mental health service utilization; analyses which will enhance our understanding of childhood PLEs. The current study examined unique longitudinal data from the ABCD Study® in school-age youth. We test the hypothesis that while both distressing and persistent PLEs might be associated with deficits in the aforementioned domains and functioning/mental health service utilization, distressing PLEs that persist over time would be most strongly associated with impairments.
Methods
Participants
The ABCD Study is a large-scale study tracking 9–10-years-olds recruited from 21 research sites across the United States (Supplement for study-wide exclusion details). ABCD Data Release 3.0 (DOI 10.15154/1519007; see Acknowledgments; collected between September 1st, 2016 and October 15th, 2018) includes 3 waves of data (all of baseline and 1-year follow-up, ~60% of 2-year follow-up): baseline (N=11 878), 1-year follow-up (N=11 235), and 2-year follow-up (N=6 571). Four groups were created to separately examine persistence and distress (Table 1, Figure 1; Supplemental Table 1; group membership was not contingent on having data at all three waves): 1) a persistent distressing PLEs group that had a PQ-BC distress score Z>=1.96 (i.e., >=1.96 standard deviations (SDs) above the mean PQ-BC distress score;) for at least two waves of data (n=272), 2) a transient distressing PLEs group that had significantly elevated dPLEs (i.e., Z>=1.96) in 1 wave and did not have significantly elevated scores (i.e., PQ-BC distress score Z<=0.50) in the other waves (n=298, of which, n=221 had complete symptom data across all three waves), 3) a persistent non-distressing PLEs group that had Z>=1.96 for PLEs without distress for at least two waves of data (n=221), 4) a transient non-distressing PLEs group that had significantly elevated (i.e., Z>=1.96) PLEs without distress in 1 wave and did not have significantly elevated scores (i.e., PQ-BC distress score Z<=0.50) in the other waves (n=536, of which, n=270 had complete symptom data across all three waves).
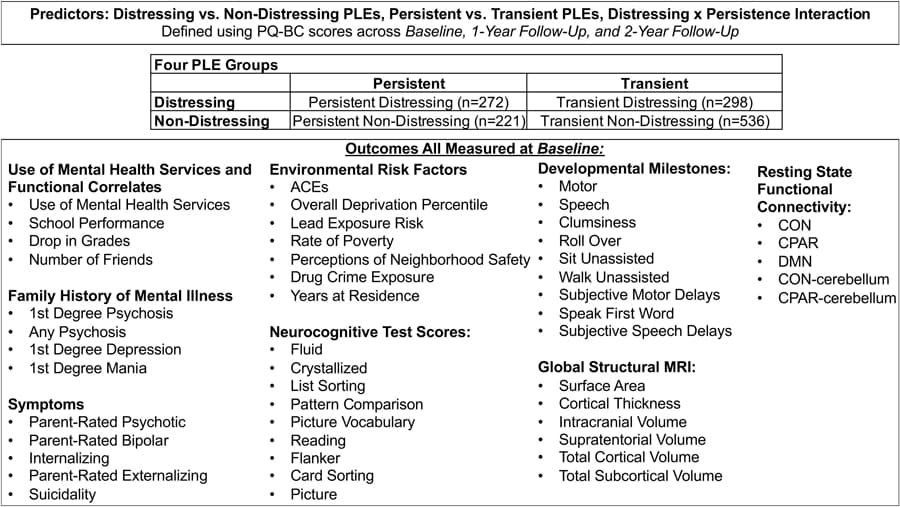
Figure 1
Overview of the groups, domains, and individuals components included in analyses. Abbreviations: PLEs=psychotic-like experiences; PQ-BC=Prodromal Questionnaire-Brief Child version; CON=cingulo-opercular; CPAR=cingulo-parietal; DMN=default mode; ICV=intracranial volume; ACE=adverse childhood events.
Table 1.
Group Characteristics
Characteristic | Whole Sample (n=11,872) | Persistent Distressing PLEs (SD; n=272) | Transient Distressing PLEs (TD: n=298) | Persistent Non-Distressing PLEs (PND; n=221) | Transient Non-Distressing PLEs (TND; n=536) | Test Statistic | df | p- value | Post-hoc
FDR-corrected Comparisons | |||||
n | % | n | % | n | % | n | % | n | % | χ
2 | ||||
Sex (% female) | 5681 | 47.9 | 131 | 48.2 | 164 | 55.0 | 75 | 34.1 | 231 | 43.1 | 24.50 | 3 | <.001 | PD=TD>PND<TND |
Race/Ethnicity, % | 16.99 | 12 | .15 | |||||||||||
White | 6174 | 52.0 | 102 | 37.5 | 112 | 37.6 | 82 | 37.1 | 231 | 43.1 | ||||
Black | 1779 | 15.0 | 63 | 23.2 | 66 | 22.1 | 63 | 28.5 | 124 | 23.1 | ||||
Asian | 252 | 2.1 | 1 | 0.4 | 3 | 1.0 | 5 | 2.3 | 9 | 1.7 | ||||
Multiracial/ Multiethnic | 1245 | 10.5 | 30 | 11.0 | 33 | 11.1 | 27 | 12.2 | 60 | 11.2 | ||||
Hispanic | 2407 | 20.3 | 76 | 27.9 | 84 | 28.2 | 44 | 19.9 | 112 | 20.9 | ||||
M | SE | M | SE | M | SE | M | SE | M | SE | F | p -value | |||
Age b | 9.473 | 0.005 | 9.401 | 0.030 | 9.440 | 0.029 | 9.475 | 0.034 | 9.411 | 0.021 | 1.20 | 3/1325 | .31 | |
Distressing PLEs | ||||||||||||||
Baseline | 6.320 | 0.097 | 35.390 | 1.141 | 23.410 | 1.109 | 17.670 | 0.768 | 9.430 | 0.428 | 197.40 | 3/1324 | <.001 | PD>(TD>PND>TND); TD>TND |
1-Year Follow-up | 4.610 | 0.089 | 35.320 | 1.126 | 8.400 | 0.763 | 14.530 | 0.611 | 8.560 | 0.504 | 276.48 | 3/1273 | <.001 | PD>(TD>PND>TND) |
2-Year Follow-up | 3.460 | 0.093 | 25.890 | 1.062 | 9.890 | 0.863 | 11.020 | 0.643 | 6.760 | 0.456 | 119.57 | 3/904 | <.001 | PD>(TD=PND>TND); TD>TND |
Non-Distressing PLEs | ||||||||||||||
Baseline | 1.316 | 0.018 | 3.540 | 0.165 | 2.591 | 0.144 | 6.208 | 0.198 | 2.864 | 0.135 | 83.81 | 3/1326 | <.001 | PND>(PD>TD=TND); PD>TND |
1-Year Follow-up | 0.915 | 0.016 | 3.559 | 0.172 | 1.148 | 0.100 | 5.851 | 0.203 | 2.295 | 0.129 | 140.78 | 3/1273 | <.001 | PND>(PD>TD<TND); PD>TND |
2-Year Follow-up | 0.445 | 0.011 | 2.610 | 0.186 | 1.369 | 0.123 | 3.253 | 0.184 | 1.392 | 0.082 | 45.18 | 3/904 | <.001 | PND>(PD>TD=TND); PD>TND |
Abbreviation: dPLE=distressing psychotic-like experiences; df=degrees of freedom; n=sample size; %=percentage; χ2=chi-square; M=Mean; SE=standard error; F=ANOVA statistic. aχ2 Tests were used to compare ordinal/binary variables across the four groups, otherwise ANOVAs were used (note, dfs for ANOVAs include the numerator/denominator). Follow-up FDR-corrected group comparisons were conducted for any models with p<.05.
Group thresholds were re-calculated at each wave, in order to partially account for re-testing effects. These thresholds were chosen based on research using this threshold on different psychosis risk questionnaires in college students.41 However, we re-ran group comparison analyses only using transient group members with complete data (note, data was not missing due to attrition, but because this data was not included in Data Release 3.0), with generally consistent results (Supplemental Table 2; see Table 3 notes for divergent findings, with three cognitive metric findings involving transient groups moving from FDRps<.05 to FDRps between .10 and .35, and several additional findings, mostly for cognitive metrics, moving from FDRps between .07 and .27 to FDRps<.05). All available data was utilized for measured risk factors (detailed below and in Figure 1), which were obtained at baseline. All procedures were approved by a central Institutional Review Board at the University of California, San Diego. All parents and children provided written informed consent and assent, respectively.
Table 3.
Descriptive Statistics and Group Comparisons for Each of the Domains and Individual Components
Persistent Distressing PLEs (PD; n=272) | Transient Distressing PLEs (TD; n=298) | Persistent Non-Distressing PLEs (PND; n=221) | Transient Non-Distressing PLEs (TND; n=536) | FDR-corrected Comparisons b | |||||
Mean | SE | Mean | SE | Mean | SE | Mean | SE | ||
Family History | |||||||||
Family History PCA | 0.135 | 0.065 | 0.156 | 0.063 | 0.209 | 0.070 | 0.063 | 0.054 | |
1 st
Degree Psychosis,% | 0.050 | 0.013 | 0.050 | 0.012 | 0.051 | 0.014 | 0.046 | 0.009 | |
Any Psychosis,% | 0.185 | 0.021 | 0.117 | 0.020 | 0.172 | 0.023 | 0.127 | 0.016 | |
1 st
Degree Depression,% | 0.311 | 0.034 | 0.297 | 0.033 | 0.360 | 0.036 | 0.317 | 0.028 | |
1 st
Degree Mania,% | 0.062 | 0.015 | 0.080 | 0.014 | 0.063 | 0.016 | 0.050 | 0.011 | |
Developmental Milestones | |||||||||
Developmental Milestones PCA | 0.140 | 0.071 | 0.177 | 0.067 | 0.023 | 0.077 | 0.008 | 0.052 | |
Motor | 0.497 | 0.051 | 0.496 | 0.048 | 0.370 | 0.055 | 0.388 | 0.037 | |
Speech | 0.354 | 0.041 | 0.320 | 0.039 | 0.277 | 0.044 | 0.298 | 0.031 | |
Structural Metrics | |||||||||
Structural Metrics PCA | −0.376 | 0.058 | −0.373 | 0.055 | −0.267 | 0.062 | −0.269 | 0.044 | |
Surface Area | 1.812E+05 | 1.029E+03 | 1.811E+05 | 9.840E+02 | 1.818E+05 | 1.114E+03 | 1.826E+05 | 7.920E+02 | |
Cortical Volume | 5.699E+05 | 3.259E+03 | 5.727E+05 | 3.112E+03 | 5.758E+05 | 3.533E+03 | 5.780E+05 | 2.479E+03 | |
Cortical Thickness | 2.730 | 0.008 | 2.742 | 0.008 | 2.747 | 0.008 | 2.746 | 0.006 | |
ICV | 1.441E+06 | 7.745E+03 | 1.442E+06 | 7.357E+03 | 1.451E+06 | 8.317E+03 | 1.450E+06 | 5.827E+03 | |
Supratentorial Volume | 1.043E+06 | 5.932E+03 | 1.043E+06 | 5.633E+03 | 1.052E+06 | 6.369E+03 | 1.053E+06 | 4.461E+03 | |
Subcortical Volume | 5.840E+04 | 3.220E+02 | 5.828E+04 | 3.060E+02 | 5.938E+04 | 3.430E+02 | 5.885E+04 | 2.490E+02 | |
RSFC Metrics | |||||||||
RSFC Metrics PCA | −0.265 | 0.106 | −0.268 | 0.102 | −0.201 | 0.110 | −0.173 | 0.094 | |
CON | 0.246 | 0.007 | 0.230 | 0.006 | 0.246 | 0.007 | 0.256 | 0.005 | TD<TND |
CPAR | 0.650 | 0.021 | 0.678 | 0.020 | 0.693 | 0.023 | 0.672 | 0.016 | |
DMN | 0.205 | 0.007 | 0.205 | 0.006 | 0.209 | 0.007 | 0.207 | 0.005 | |
CPAR-cerebellum | −0.024 | 0.013 | −0.030 | 0.012 | 0.005 | 0.013 | −0.015 | 0.010 | |
CON-cerebellum | 0.046 | 0.006 | 0.052 | 0.006 | 0.038 | 0.007 | 0.034 | 0.005 | |
Functioning Impairments/Mental Health Service Utilization | |||||||||
Functioning Impairment PCA | 0.441 | 0.086 | 0.215 | 0.082 | 0.148 | 0.094 | 0.172 | 0.069 | PD>(TD=PND=TND) |
Use of Mental Health Services,% | 0.274 | 0.028 | 0.221 | 0.026 | 0.214 | 0.030 | 0.166 | 0.022 | |
School Performance | 3.300 | 0.043 | 3.390 | 0.041 | 3.490 | 0.048 | 3.420 | 0.031 | |
Drop in Grades,% | 0.202 | 0.027 | 0.118 | 0.025 | 0.163 | 0.029 | 0.152 | 0.021 | |
Number of friends | 23.500 | 1.390 | 23.000 | 1.320 | 21.200 | 1.530 | 20.400 | 1.000 | |
Other Reported Psychopathology | |||||||||
Symptoms PCA | 0.489 | 0.089 | 0.157 | 0.081 | 0.067 | 0.094 | 0.156 | 0.065 | PD>(TD=PND=TND) |
Bipolar | 0.890 | 0.098 | 0.513 | 0.090 | 0.437 | 0.105 | 0.497 | 0.070 | PD>(TD=PND=TND) |
Suicidal Ideation | 0.695 | 0.0624 | 0.352 | 0.0586 | 0.406 | 0.0682 | 0.197 | 0.0447 | |
Suicidal Behavior | 0.2406 | 0.0402 | 0.1316 | 0.0378 | 0.1178 | 0.0437 | 0.0381 | 0.0296 | |
Externalizing | 6.430 | 0.547 | 4.330 | 0.505 | 4.040 | 0.586 | 4.170 | 0.393 | PD>(TD=PND=TND) |
Internalizing | 2.399 | 0.177 | 1.160 | 0.165 | 1.279 | 0.190 | 0.616 | 0.134 | PD>(TD=PND>TND);TD>TND |
Psychotic | 0.617 | 0.097 | 0.248 | 0.090 | 0.299 | 0.105 | 0.327 | 0.070 | |
Cognition | |||||||||
Cognition PCA | -0.505 | 0.060 | −0.442 | 0.056 | −0.194 | 0.065 | −0.342 | 0.044 | PD<(PND=TND);TD<PND c |
Fluid | 86.600 | 0.677 | 88.500 | 0.640 | 89.700 | 0.738 | 88.400 | 0.500 | PD<PND d |
Crystallized | 83.200 | 0.419 | 83.600 | 0.398 | 84.700 | 0.456 | 84.200 | 0.312 | |
List Sorting | 91.500 | 0.786 | 92.900 | 0.745 | 95.500 | 0.861 | 92.800 | 0.573 | (PD=TD)<PND>TND d,e |
Pattern Comparison | 84.700 | 0.952 | 86.600 | 0.902 | 85.200 | 1.037 | 85.400 | 0.705 | |
Picture Vocabulary | 80.600 | 0.471 | 81.300 | 0.448 | 83.100 | 0.513 | 81.900 | 0.357 | PD<(PND>TND);TD<PND c,f |
Reading | 88.700 | 0.463 | 88.900 | 0.441 | 89.200 | 0.502 | 89.400 | 0.348 | |
Flanker | 92.500 | 0.657 | 92.300 | 0.622 | 93.200 | 0.714 | 92.100 | 0.491 | |
Card Sorting | 88.700 | 0.678 | 90.600 | 0.644 | 91.700 | 0.737 | 90.700 | 0.506 | PD<(TD=PND=TND) |
Picture | 99.100 | 0.751 | 100.900 | 0.711 | 101.900 | 0.823 | 101.200 | 0.540 | |
Environmental Adversity | |||||||||
Environmental Adversity PCA | 0.520 | 0.107 | 0.276 | 0.105 | 0.388 | 0.111 | 0.330 | 0.100 | PD>(TD=TND) |
ACEs | 1.930 | 0.159 | 1.250 | 0.148 | 1.310 | 0.168 | 1.480 | 0.124 | PD>(TD=PND=TND) |
Overall Deprivation Percentile | 45.600 | 4.390 | 40.800 | 4.380 | 42.000 | 4.450 | 42.600 | 4.320 | PD>TD d |
Lead Exposure Risk | 5.800 | 0.394 | 5.640 | 0.395 | 5.770 | 0.398 | 5.750 | 0.391 | |
Rate of Poverty | 23.700 | 1.760 | 22.100 | 1.760 | 23.200 | 1.810 | 23.000 | 1.720 | |
Perceptions of Neighborhood Safety | 11.000 | 0.281 | 11.200 | 0.273 | 10.900 | 0.294 | 11.100 | 0.248 | |
Years at Residence | 5.130 | 0.240 | 5.360 | 0.240 | 4.770 | 0.267 | 5.190 | 0.212 | |
Drug Crime Exposure | 8.860E+03 | 2.959E+03 | 8.863E+03 | 2.959E+03 | 8.860E+03 | 2.959E+03 | 8.859E+03 | 2.959E+03 |
Measures
All measures are described in detail within the Supplement.
Prodromal Questionnaire-Brief Child Version (PQ-BC)
Participants completed the previously validated Prodromal Questionnaire-Brief Child Version (PQ-BC).42 Consistent with previous research,37,42 distress scores were calculated as the total number of 21 questions endorsed weighted by level of distress [i.e., 0=no, 1=yes (but no distress), 2–6=yes (1+score on distress scale); range: 0–126]. Distress scores were used to create the persistent and transient distressing PLE groups. A sum of the number of PLEs endorsed with no distress were used to create the persistent and transient non-distressing PLE groups.
Other Psychopathology and Functioning Measures
Summations of Kiddie-Structured Assessment for Affective Disorders and Schizophrenia (KSADS) for DSM-543 caregiver-rated psychotic symptoms,44current bipolar symptoms, and externalizing symptoms (i.e., current attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder symptom summations),44 youth-rated internalizing symptoms (i.e., current depression and generalized anxiety disorder symptom summations; Supplemental Table 3 for group comparisons of disorder prevalence), suicidal ideation (e.g., thinking of a suicidal plan), and suicidal behavior (i.e., suicide attempt) were examined.Use of mental health services was measured by asking whether the youth has ever received mental health services. School performance was measured using caregiver-rated KSADS questions regarding how well the youth does in school and whether there was a drop in grades over the past year. Social functioning was measured using youth-rated number of close friends.History of psychotic disorder, depression, and mania in first-degree relatives was assessed using the Family History Assessment Module Screener,45 with each scored as either present or absent. Any history of psychotic disorders was scored as present if the participant had any first- or second-degree relatives with a psychotic disorder history.
Neuropsychological Test Battery
The current study utilized uncorrected National Institutes of Health Toolbox Cognitive Battery scores from the 7 individual tests and fluid and crystallized composite scores.46
Developmental Milestones
The current study examined summations of parent-reported motor and speech developmental milestone delays.47
Environmental Adversity
Based on previous research finding associations with PLEs in the ABCD sample,40 we examined: caregiver-rated perception of neighborhood safety, adverse childhood experiences (ACEs), number of years at current residence, and based on primary address: drug crime exposure, overall deprivation, rate of poverty, and lead exposure risk estimates.
Structural MRI Measures
Structural neuroimaging processing was completed using FreeSurfer version 5.3.0 through standardized processing pipelines.48 For the current study, structural MRI measures include total volume (intracranial [ICV], supratentorial [STV], cortical, and subcortical),49 surface area,50 and cortical thickness.51 All data were acquired on a 3T scanner (Siemens, General Electric, or Phillips) with a 32-channel head coil and completed T1-weighted and T2-weighted structural scans (1mm isotropic).
Resting State Functional Connectivity (RSFC)
Participants completed four 5-minute resting-state BOLD scans, with their eyes open and fixated on a crosshair. Resting state images were acquired in the axial plane using an EPI sequence. Other resting-state image parameters varied by 3T scanner and have been previously detailed (https://abcdstudy.org/images/Protocol_Imaging_Sequences.pdf).52 The data analysis pipeline has also been detailed previously.39 Consistent with previous research using the ABCD sample to examine associations with PQ-BC scores,39 we examined cingulo-opercular (CON) within-network connectivity, cingulo-parietal (CPAR) within-network connectivity, default mode (DMN) within-network connectivity, CON-cerebellar connectivity, and CPAR-cerebellar connectivity.
Covariates
Every model included age, sex, race/ethnicity (i.e., White, Black, Hispanic, Asian, Multiracial/Multiethnic), and financial adversity (Supplement) as covariates. However, environmental adversity models did not include race/ethnicity as a covariate due to the fact that many of these factors (e.g., deprivation, reduced access to resources) disproportionately affecting racial and ethnic minorities due to structural racism. As such, if one includes race/ethnicity in these models and the overlap with environmental risk factors leads PLE factors to no longer be associated with environmental risk, it may be incorrectly interpreted as the absence of PLE factor associations. Lastly, imaging analyses included scanner type as a covariate, with RSFC analyses additionally including mean motion as a covariate.
Statistical Analyses
The analyses used hierarchical linear models (HLMs) conducted using the R lme4 package.53 All analyses modeled family unit and research site as random intercepts. HLMs analyzed main effects of distressing and persistent PLEs and a persistent x distressing interaction (Figure 1). To provide an overall summary of each domain, a principal component analysis (PCA) was conducted using each domain’s individual components and included the whole baseline ABCD sample (Figure 1), and the first component was retained for each domain (each first component explained >32% of the total variance; Supplemental Table 4 for associations between domains). Next, we examined each individual component within each domain (Figure 1). For each model, we visually examined homogeneity of variance and plotted the residuals to examine whether the residuals were normally distributed. If the assumption of normality appeared to be violated, metrics were log-transformed (e.g., developmental milestones, symptoms), with results remaining consistent. For any PCA domain or individual component with a persistence x distress interaction, follow-up analyses examined pair-wise comparisons to examine False Discovery Rate (FDR)-corrected differences across the four groups for each model using the lsmeans package.54
Results
Four groups varying in PLEs persistence and distress endorsement were created: persistent distressing PLEs (n=272; 2.3% of total sample), transient distressing PLEs (n=298; 2.1% of sample), persistent non-distressing PLEs (n=221; 1.9% of sample), and transient non-distressing PLEs (n=536; 4.6% of sample) groups (Figure 1; Table 1; Supplemental Table 5 for comparisons with a group with Zs<=0.50 for PLEs scores for all waves of data collection).
Family History
The family history domain did not show any significant main effects, although there was a trend towards an interaction (Table 2; Figure 2). For individual components, there was a main effect of persistence for any family history of psychosis, with higher rates among persistent groups.
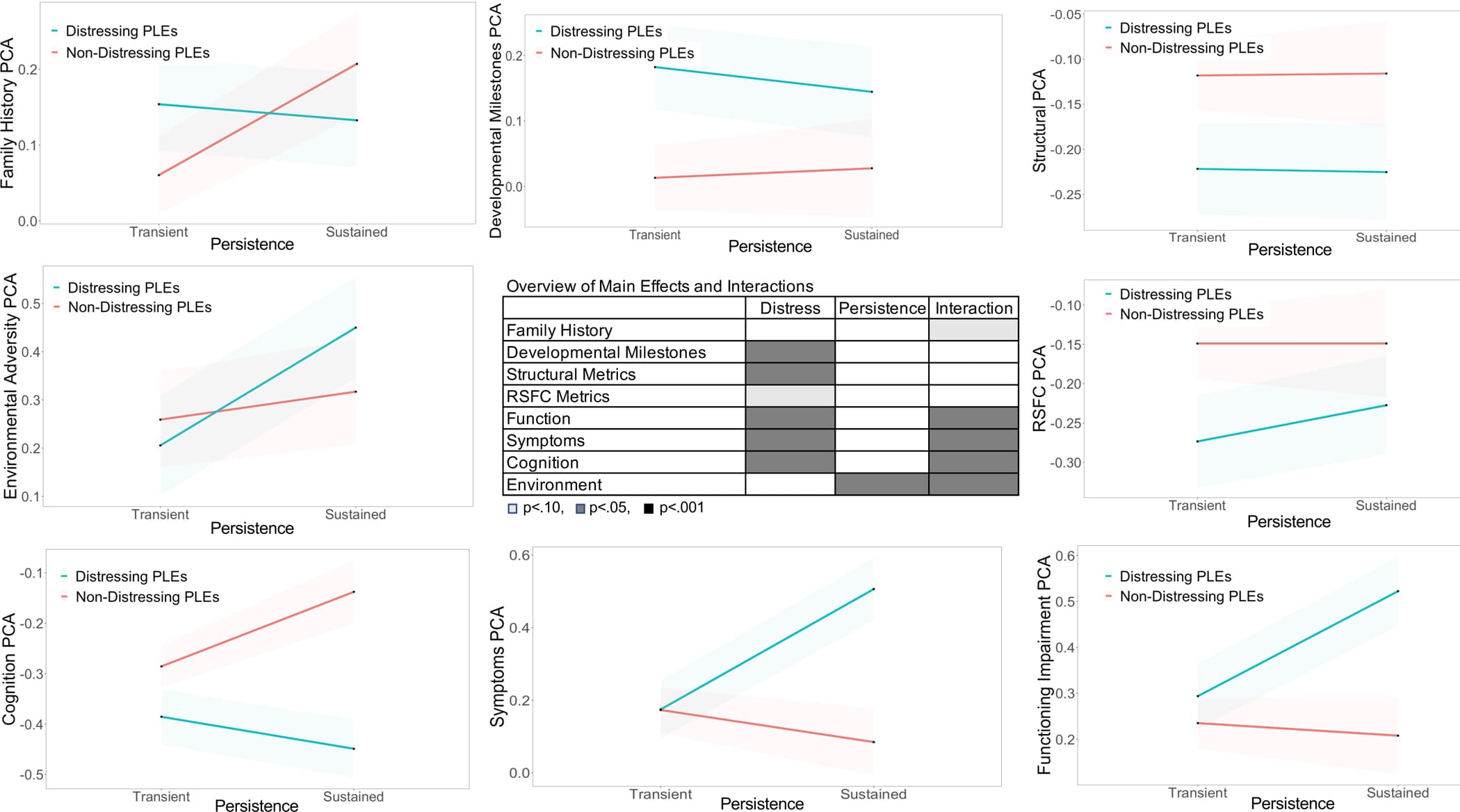
Figure 2
Depictions of mean score estimates and confidence intervals for each of the four groups (i.e., persistent distressing PLEs, transient distressing PLEs, persistent non-distressing PLEs, transient non-distressing PLEs) for each of the PCA-generated domains. The center of the figure depicts whether each PCA-generated domain showed a main effect of distress, main effect of persistence, and interaction effect. Abbreviations: RSFC=resting state functional connectivity.
Developmental Milestones
As a domain, there was a main effect of greater distressing PLEs associated with greater developmental milestones delays (Table 2; Figure 2). Consistent with the domain results, there was a main effect of greater distressing PLEs associated with greater motor delays.
Structural MRI Metrics
The structural MRI domain showed a main effect of distress, whereby youth with more distressing PLEs showed reduced structural brain metrics (Table 2; Figure 2). Consistent with the domain results, youth with more distressing PLEs showed lower cortical and subcortical volumes.
RSFC Metrics
The RSFC domain did not show main effects or an interaction (Table 2). There were several main effects of distress for individual components, including evidence that youth with more distressing PLEs showed lower CON-Cerebellum and higher CPAR-Cerebellum metrics. Furthermore, within-network CON RSFC showed an interaction between distress and persistence which, unlike all other interactions, was characterized by a stronger effect of distress for transient PLEs groups compared to persistent PLEs groups (Table 3), with the transient distressing PLEs group showing lower connectivity compared to transient non-distressing PLEs.
Functioning/Mental Health Service Utilization
In this domain, there was a distress x persistence interaction, characterized by a stronger effect of distress for the persistent PLEs groups compared to the transient PLEs groups, with the persistent distressing PLEs group showing the greatest functional impairments and greater mental health service utilization (Figure 2; Table 3). The individual components showed somewhat different results than the domain. There were several main effects of distress, with youth reporting greater distress also reporting greater mental health service utilization and worse school performance. There were also several main effects of persistence, with youth reporting persistent PLEs also reporting greater mental health service utilization and greater drop in grades.
Other Reported Psychopathology
For the overall symptoms domain, there was a distress x persistence interaction, characterized by a stronger effect of distress for the persistent groups compared to the transient groups, with the persistent distressing PLEs group showing the strongest effects (Figure 2; Table 3). Several of the individual symptom components showed significant interactions between distress and persistent PLEs, including bipolar symptoms, externalizing and internalizing symptoms, and a trend for caregiver-rated psychotic symptoms (Table 2), consistent with the domain results (Table 3). For suicidal ideation and behavior symptoms, there were main effects of distress and persistence, with youth endorsing more distressing PLEs, as well as more persistent PLEs, showing greater suicidal ideation and behavior.
Cognition
For the overall cognition domain, there was again a distress x persistence interaction (Table 2), characterized by a stronger effect of distress for the persistent PLEs groups compared to the transient groups, with the persistent distressing PLEs group showing the strongest effects (Table 3; Figure 2). A number of the individual cognition components also showed distress x persistence interactions, including fluid cognition, list sorting working memory, picture vocabulary, and card sorting, consistent with the domain results (Table 3). There was also a main effect of distress for the crystallized composite, whereby youth endorsing greater distress showed lower performance.
Environmental Adversity
For the overall environmental adversity domain, there was again a distress x persistence interaction, characterized by a stronger effect of distress for the persistent PLEs groups compared to the transient PLEs groups, with the persistent distressing PLEs group showing the strongest effects (Tables 2–3; Figure 2). In terms of individual components, both ACEs and overall deprivation scores showed distress x persistence interactions, consistent with the domain results. Lastly, there was a main effect of persistence for years at residence, whereby youth endorsing persistent PLEs showed fewer years at their residence.
Discussion
The current study examined whether both distressing and persistent PLEs were associated with important risk factors and functioning/mental health service utilization domains. Overall, there was evidence that youth endorsing greater distressing PLEs showed impairments on several domains, including developmental milestones and structural MRI metrics. There was evidence persistent PLEs were associated with individual components (e.g., family history of psychosis, fewer years at residence). Importantly, for a number of domains, including functioning/mental health service utilization, symptoms, cognition, and environmental adversity factors, the effect of distress was larger for the persistent compared to the transient PLE groups. Overall, the persistent distressing PLE group exhibited the greatest impairments across the domains.19,22 These findings provide some evidence that it is generally only in the context of distress that persistent PLEs are associated with a range of impairments.
There were several domains that showed greater impairments for distressing PLEs, irrespective of persistence. These correlates were generally in pathophysiology-related domains, including developmental milestone delays, especially motor milestone delays, and structural MRI metrics, including lower global brain volume.55,56 This evidence helps confirm clinical insights and empirical evidence that distressing PLEs, as opposed to non-bothersome PLEs, are associated with impairments.24,57 The possibility exists that perhaps early (e.g., prenatal, perinatal, or early developmental) insults and/or genetics may lead to both developmental milestone delays and neuroanatomical abnormalities that may in turn later lead to psychopathological symptoms, perhaps specifically distressing PLEs. Potentially consistent with this speculative explanation of early insults potentially contributing to later distressing PLEs, disrupted cerebellar connectivity and lower crystallized cognitive scores were additionally associated with distressing PLEs. Lastly, consistent with previous research, symptoms of suicidal ideation and behavior,58,59 and use of mental health services60,61 were associated with distressing PLEs, perhaps partially a consequence of the experience of distress.57
Few findings were associated with persistent PLEs irrespective of distress, with no domain-level findings. In terms of individual components, greater family history of psychosis and fewer years at residence were associated with increased persistent PLEs. The family history finding is at least somewhat consistent with family history of psychotic disorders being associated with later development of an array of psychosis spectrum disorders, including disorders not necessarily characterized by distress (e.g., schizotypal personal disorder).62 Unexpectedly, there were no significant effects for the family history domain (although there was a trend towards an interaction) or 1st degree family history of psychosis, although notably for all family history indices outside of depression, the transient non-distressing group numerically showed the lowest rates compared to the other three groups. The lack of robust family history effects may reflect large environmental and epigenetic influences on early PLEs. Finding fewer years at residence associated with persistent PLEs is consistent with findings that persistent PLEs are associated with greater residential mobility during childhood.63 Symptoms of suicidal ideation and behavior were both associated with persistent versus transient PLEs, which is an important indication that in addition to distress, persistence of PLEs are also associated with suicidal ideation and behavior.58,59,64 These analyses did not find stronger evidence for associations between suicidal behavior compared to ideation with PLEs, inconsistent with some previous work.65 The current study also found that persistent PLEs, in addition to distress, were associated with a drop in grades. Notably, these findings contribute to the inconsistent literature regarding associations between PLEs and school performance,61 perhaps indicating the importance of accounting for persistence in this domain.
For several domains, including functioning/mental health utilization, other symptoms, cognition, and environmental adversity domains, there was a stronger effect of distress for persistent versus transient PLEs, with persistent distressing PLEs showing the greatest impairment, perhaps in line with findings indicating early PLEs are associated with later functional impairment.66,67 One possible interpretation is that there are several subsets of PLE trajectories, including some that may indicate underlying vulnerability to psychosis spectrum disorders (e.g., persistent distressing PLEs), some that may be transdiagnostic (e.g., transient distressing PLEs, perhaps some of the non-distressing PLEs), and perhaps some that may be of lower clinical relevance (e.g., the majority of non-distressing PLEs, although transient non-distressing PLEs did show impairments on a variety of domains in comparison to a group endorsing minimal PLEs, Supplemental Table 5).27
For the symptom domains, the persistent distressing PLEs group showed higher levels of both caregiver-reported externalizing and bipolar as well as self-reported internalizing symptoms compared to the other groups, in line with previous work.19 It is likely these symptoms exacerbate PLEs (and/or vice versus). Finding higher caregiver-rated symptoms in the persistent distressing PLEs group is critical validation that this group is exhibiting more severe psychopathology, including greater caregiver symptom awareness. For the functioning/mental health service utilization domain,60,61 overall the persistent distressing group showed the greatest impairments in this domain. These data are consistent with the idea that clinicians may consider using persistence of distressing PLEs as a marker of identifying individuals most in need of evaluation and intervention.
For cognitive functioning, again, the persistent distressing PLEs group showing the greatest impairments. This group numerically showed the greatest impairments on several cognitive domains, including the fluid composite and tests of working memory (listing sorting), picture vocabulary, and executive functioning (card sorting). Interestingly, the only test in which the persistent distressing PLEs group showed significantly lower scores compared to all other groups was the executive functioning test, perhaps indicating this may be an important delimiting cognitive marker of PLE severity. Overall, these findings are consistent with previous work finding working memory,68 receptive language impairments,32,69 and executive functioning70 as potential important markers in the development of clinically-relevant psychosis spectrum symptoms. Neurocognition may partially account for presenting symptoms and problems and/or may reflect underlying anomalies in pathophysiology.
For environmental adversity, finding an interaction for factors including ACEs and overall deprivation is somewhat consistent with previous work finding that persistent PLEs were associated with increased traumatic experiences,21,22 although the current work finds that persistent PLEs are associated with increased ACEs only in the context of distress. This finding is in line with theories that exposure to additional environmental risks, such as ACEs, can interact with genetic vulnerabilities to contribute to subclinical psychosis spectrum symptoms becoming initially distressing and persistent.29,30 In terms of speculative mechanisms, previous work has theorized that increased chronic stressors cumulatively result in downstream neurobiological effects (e.g., dopamine sensitization, HPA axis dysfunction), potentially resulting in persistent distressing PLEs.12
The current study had several limitations and points to consider. The groups were created based on a priori(versus data driven) definitions of group membership, as we were specifically interested in examining contributions of persistence and distressing factors towards impairments in domains. Due to the structure of the data, persistence had to be measured in a discrete manner. The current study used thresholds to examine interactions between distress and persistence. These thresholds were used to be congruous with other psychosis risk research41 and to create similarly sized groups, although other thresholds could have been used. The choice to not require complete data may have led to the incorporation of individuals in the transient group that will later belong to the persistent group, which may have occluded findings related to persistent PLE effects. This notion is partially supported in finding that when only including complete transient data in analyses, several additional findings emerge for comparisons between the persistent distressing and transient not distressing groups (and between the transient distressing and non-distressing groups; see Supplemental Table 3). Future ABCD data waves can examine the extent to which group membership changes over time, incorporate data-driven modeling approaches, and eventually, predict psychosis spectrum disorder outcomes. Several measures had notable limitations, including limited psychometric validity data (e.g., number of friends, K-SADs symptom measures), reliance on retrospective recall (e.g., developmental milestones), and/or limitations in caregiver’s awareness of the events and willingness to report (ACEs measure).71 Included variables were chosen as best approximations based on available ABCD baseline data. Only group comparison analyses (Table 3) are multiple comparison corrected. We are unable to examine presence of psychotic disorders diagnoses, as this information is not available. It is also possible that some individuals in the persistent dPLEs group (or even other groups) may be currently experiencing psychotic symptoms. While the current study found evidence consistent with persistent distressing PLEs showing greatest impairments, since this group endorsed the greatest frequency of PLEs (Table 1), it is not possible to entirely rule out that greater PLEs endorsement in general is associated with greater impairments. More frequent PLEs are generally experienced as more distressing,24although distress is a stronger predictor of symptom severity.72
The current research furthers our understanding of associations between persistent and distressing PLEs with impairments in a number of domains, finding evidence in support of the notion that distressing PLEs that persist over time are indeed associated with greater impairments in symptoms, functioning/mental health service utilization, cognition, and greater endorsements of environmental adversity. These findings further highlight that persistent and distressing PLEs represent an important screening target, regardless of the percentage of these youth who go on to develop specific psychotic disorders.73 Additionally, it is possible that many of these effects will strengthen over time as these groups become enriched for those at risk for psychiatric disorders. It is also possible that impairments in several risk factors (e.g., neural impairments) may intensify over development, such as in adolescence. Future ABCD data releases will continue to examine risk factor trajectories of persistent distressing PLEs, including clinical and functional outcomes as these youth enter adolescence and young adulthood.