Abstract
Major depression disorder (MDD) and bipolar disorder (BD) are usual comorbidities in patients with substance use disorders (SUD), a condition known as dual disorder (DD). MDD, BD and SUD are associated with cognitive impairment, potentially leading to a greater functional impairment in the context of DD. Objectives: To review the existing data on the cognitive impairment in DD patients with comorbid MDD or BD, considering the influence of the depressive symptomatology. Methods: Following the PRISMA protocol 19 studies were selected from the last 17 years, 13 of which focused on BD, five on MDD and one included both diagnoses. Results: Studies based in BD+SUD showed that the most affected cognitive domains were attention and executive functions, but not all of them found a greater impairment due to the comorbidity. While fewer studies were found for depression, MDD+SUD works point to a similar impairment cognitive pattern. Furthermore, depression improvement could be associated to better cognitive performance. Limitations: More standardized research is needed regarding the influence of depression on cognitive performance of DD patients, especially on those with comorbid MDD. Factors such as main substance, abstinence, or MDD/BD-related variables should be considered. Unstudied factors, like gender or circadian rhythms, are proposed to improve knowledge in this area. Conclusions: Current studies suggest that DD could potentiate cognitive impairment in BD, MDD and SUD. However, additional research is needed to improve the understanding of comorbidity to apply more individualized therapies in the treatment of these patients, considering the interference of their neurocognitive functioning.
1. Introduction
The term dual disorder (DD) refers to the coexistence or concurrence of at least one substance use disorder (SUD) and another mental disorder in the same person (World Health Organization, 1994). Such comorbidity is associated with a worse prognosis and recovery if both conditions are not treated simultaneously (Hakobyan et al., 2020; Tirado-Muñoz et al., 2018). To establish the presence of a DD, the mental disorder must be independent and not a consequence of the SUD, meaning that the comorbid disorder must not be related to a significant increase or decrease in consumption (as in a SUD-induced episode), but must appear at a time of stable consumption, and must persist after a period of abstinence (Tirado-Muñoz et al., 2018). This is important because, given that the diagnosis is purely based on clinical criteria, it is usually difficult to differentiate both types of episodes, and an accurate diagnosis has a real impact on the election of an adequate pharmacologic and therapeutic treatment (Fonseca et al., 2022).
The estimated prevalence of DD is highly heterogeneous in the literature, depending on the type of population considered (outpatients, inpatients, homeless people…). Due to this, it is not easy to establish a stable prevalence for each of the comorbid mental disorders. Overall, major depression disorder (MDD) and bipolar disorder (BD) are usually the most reported comorbidities, with considerably higher rates of prevalence in comparison with anxiety disorders and even psychotic disorders (Maremmani et al., 2018). When compared to other anxiety and mood disorders, the diagnosis of MDD has been found to have the higher odds ratio of all in the SUD population (Lai et al., 2015). The prevalence of MDD+SUD was around 40%, while BD+SUD had a prevalence of 20%. Although it is a variable value, this proportion is usually maintained or may even be higher. For example, in an inpatient-based study, Gabriels et al. (2019) found a prevalence of more than 70% of MDD in patients with alcohol use disorder (AUD), while the prevalence of BD in this same population was of about 20%.
Overall, as seen in various studies and reviews published on the topic (Balanzá-Martínez et al., 2015; Davis et al., 2006; Duijkers et al., 2016; Gabriels et al., 2019), the prevalence of DD with comorbid MDD could be established, as a general value, in a range from 7% to 30%, depending on the assessed population, and around 20–30% for DD with comorbid BD. These data, both in MDD+SUD and BD+SUD, reach a lifetime prevalence of almost 60% when concurrent alcohol consumption is considered (González-Pinto et al., 2021). In relation to MDD+SUD, whose prevalence has been studied to a greater extent in the general population (Blanco et al., 2012), lifetime prevalence was around 6%, very close to the 7.5% prevalence of MDD without a SUD. In the context of DD, depressive symptomatology tends to be more severe, and depressive episodes tend to be more frequent than in MDD without an SUD. Moreover, Brière et al. (2014) carried out a longitudinal study in the general population, following individuals from adolescence to adulthood over a span of almost 15 years. Their results showed an overall lifetime prevalence of 20.5% for DD of MDD and AUD. This comorbidity was strongly associated to an increased number of suicide attempts and greater severity of AUD. However, in this case, it was not associated with the severity of MDD. Similarly, in an outpatient population study of MDD+AUD, a prevalence of 24.7% was reported, together with an increase in the problematic alcohol consumption predicting an increase in the intensity of depressive symptoms (Pavkovic et al., 2018).
Other studies have specifically analyzed the type and intensity of symptoms of depression in the presence of SUD. Carton et al. (2018) found that comorbidities of both MDD and BD are associated with greater severity of sleep problems, more thoughts of death and more suicide attempts. Lower overall quality of life and more relapses have also been associated with the coexistence of MDD and SUD compared to SUD without MDD (Marquez-Arrico et al., 2020). Moreover, it seems that the presence of SUD when initiating an antidepressant treatment in MDD patients is associated with a higher risk of treatment resistance (Brenner et al., 2020). In the same way, the use of pharmacotherapy in the treatment of depressive or manic symptomatology may be problematic due to the coexistence of a SUD (González-Pinto et al., 2021; Torrens et al., 2021).
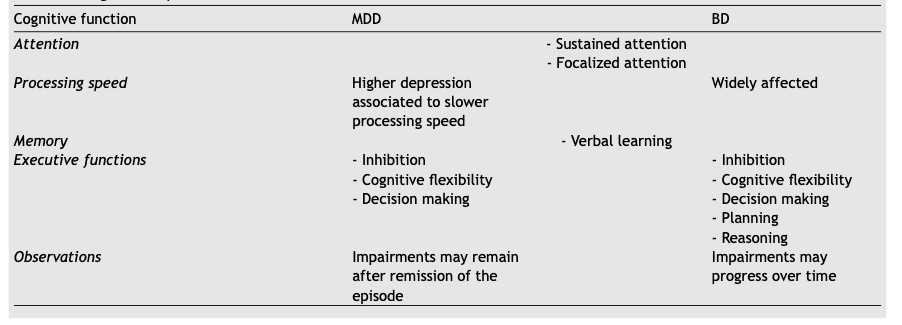
Among all the variables that contribute to the magnitude of comorbidity consequences, cognition plays a crucial role. Cognitive impairment can be found in almost any mental disorder as well as in SUD, although results may vary depending on various clinical (i.e. severity, type of medication, number of episodes) and methodological factors (i.e., moment of assessment, tasks used). The presence of a DD seems to intensify this impairment in a synergistic way, but studies in this line are frequently based on schizophrenia samples, with very little literature based on MDD. Although there is some more literature on BD, these studies rarely consider the influence of the depressive symptoms, sometimes even including the presence of depression as an exclusion criterion, which makes it difficult to explore the influence of these symptoms on the clinical phenotype and on the treatment selection of BD. A comparison of the cognitive findings in both BD and MDD, which are developed in the following sections, can be found in Table 1.
1.1. Neuropsychological profile of major depression
MDD is the second most frequent cause of disability worldwide and the major cause of disability among mental and neurological disorders (Mcintyre et al., 2018; Otte et al., 2016). The 12-month prevalence is around 6%, while the lifetime prevalence is estimated to be around 20%, with no significant differences between high-income and low-income countries (Otte et al., 2016). In patients with MDD, the loss of productivity in the workplace is probably one of the most important disability factors, along with the subsequent employment loss. Although often unexplored in the clinical setting, the literature shows that these consequences are largely associated with the cognitive dysfunction exhibited by MDD patients (Clark et al., 2016; Mcintyre et al., 2018).
The cognitive dysfunction found in MDD has been described and identified in multiple studies over the last decades. Recent reviews summarize such dysfunction as consisting of a fronto-subcortical profile with impairments in attention, verbal learning, and executive functions (Otte et al., 2016; Ponsoni et al., 2020). Depending on the severity of the depressive symptomatology, processing speed impairments may also be found, even in first episodes (Papakostas, 2014). In fact, this is one of the most addressed difficulties, usually described as “a feeling of slow thinking”. Dysfunction affecting sustained and focalized attention are common in MDD, making it difficult to focus or maintain concentration on a task, leading to problems in the workplace (Clark et al., 2016; Pan et al., 2019). Among the executive functions, which are those involved in goal-directed behaviour, MDD seems to affect particularly inhibition, cognitive flexibility and decision making (Clark et al., 2016; Papakostas, 2014; Ponsoni et al., 2020). In daily life, these types of impairments are also directly associated with a worse social functioning (Otte et al., 2016). In a therapeutic context, the neurocognitive impairment seems to be associated with more difficulties in achieving or maintaining remission (Papakostas, 2014). Furthermore, even when remission is achieved, attention, executive and learning impairments may remain as residual symptoms, although less severe than during the depressive episode (Clark et al., 2016; Mcintyre et al., 2018; Otte et al., 2016; Pan et al., 2019; Papakostas, 2014; Serra-Blasco et al., 2019).
1.2. Neuropsychological profile of bipolar disorder
BD has also been frequently presented as one of the most common causes of disability, and has been associated with a high suicide rate (Merikangas et al., 2011). In comparison with MDD, the prevalence of BD is slightly lower (with a lifetime prevalence of around 4%, and a 12-month prevalence of 0.4-0.6%).The neuropsychological profile found in BD shows impairments in verbal memory and executive functions, as in MDD, together with a slow processing speed that is more evident than in MDD across studies (Cardoso et al., 2015; Kapczinski et al., 2016). The memory-related impairments especially predict a worse functional outcome in a longitudinal follow-up, even in euthymic patients, although subclinical depressive symptomatology plays an important role in modulating this association (Bonnín et al., 2010, 2012). In the same line, a study found that the severity of depression is associated with worse social functioning and cognitive performance in all the domains analysed (Kapczinski et al., 2016).
BD is considered a chronic disease that alternates episodes of depression and manic symptoms with euthymic stages, which makes it difficult to reach a conclusion about which factor contributes more to the cognitive impairment, mainly due to the heterogeneity in study designs. Aiming to solve this difficulty, some longitudinal studies have proposed the theory of neuroprogression in BD, which would imply that cognition worsens along the progression of the disorder. In relation to this, a review summarized that all the domains affected in BD worsen over time in association with clinical variables such as number of episodes or the duration of illness (Cardoso et al., 2015).
1.3. An overview on the neuropsychology of substance use disorders
The cognitive profile described for SUD is generally similar to that described for MDD, BD and other mental disorders. Attention and verbal learning are frequently affected, and impairment in executive functions is particularly important in the addiction field. Depending on the main drug of consumption, the methodology used, and other disease-related factors, different patterns of cognitive impairment can be found. For example, cannabis seem to affect memory to a larger extent than other substances, as well as some executive functions (although research has not reached a clear consensus as yet) (Curran et al., 2016; Kroon et al., 2021); whereas cocaine seems to affect to a broader variety of functions, with executive functions such as impulsivity and decision making, attention, working memory, and processing speed being greatly affected (Lappin & Sara, 2019; Potvin et al., 2014). However, when considering executive functions, inhibition, cognitive flexibility, and specially reward-based decision making seem to be the most affected functions in this population, regardless of the substance of use. As a special case, alcohol is also known to affect visuoespatial functions in a way that no other substance does, due to the effect on the parietal lobe (Lees et al., 2020; Squeglia et al., 2014). As in MDD, although not frequently explored in clinical setting, this impairment has been linked to lower adherence to treatment and an increased probability of relapse (Perry & Lawrence, 2017; Verdejo-Garcia et al., 2019).
A recent review (Gogia et al., 2022) has already assessed the influence of BD+SUD on cognition, concluding that most studies tend to indicate a potentiation of the impairment when both disorders are present, but the literature focusing on cognitive performance of the comorbid diagnosis of MDD is, as for now, very limited, despite being highly prevalent among patients with SUD.
Therefore, the objective of this review is to analyse the influence of depressive symptomatology on the cognitive performance and prognosis in DD subjects with either MDD (MDD+SUD) or BD (BD+SUD). Furthermore, considering that SUD, MDD and BD are characterized by different alterations in executive functions, memory, attention, and processing speed, it could be hypothesized that in DD there is a synergistic potentiation of cognitive dysfunction, leading to a worse prognosis in patients with comorbidity.
2. Experimental procedures
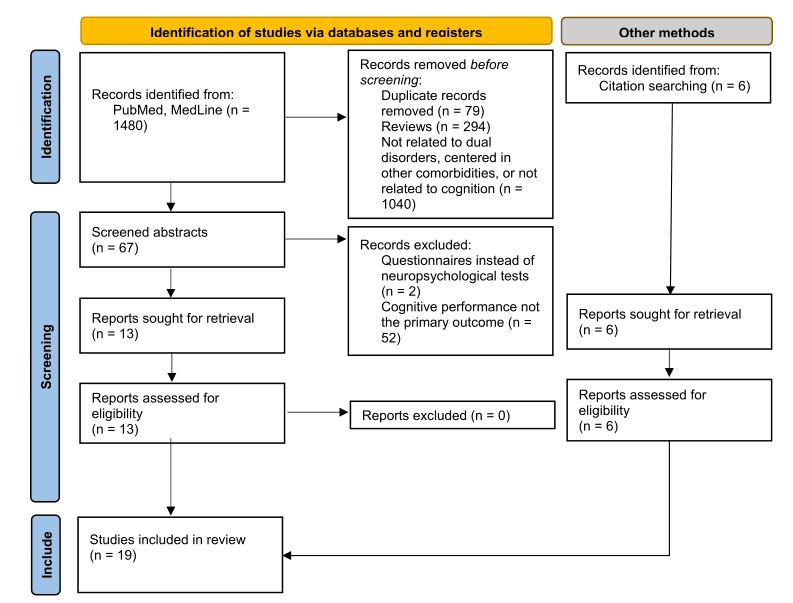
The search and selection of relevant studies was performed and reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Page et al., 2021). The search was conducted through the databases MEDLINE and PubMed, using different combinations of the keywords “dual disorders” or “substance use disorder” with “depressi*” and/or “bipolar disorder” and “cognition” or “neuropsych*”. Due to the nature of the research on these substances, “cannabis” and “alcohol” terms were used to find literature on their coexistence with MDD and BD. During the selection process, a secondary search was made among the bibliography of the selected studies, and additional research was carried out to obtain relevant information for the introductory part of the review.
The inclusion criteria for the articles were that they were written in English with full text available on-line, that cognitive performance was the main outcome, and that this performance was not measured with questionnaires but by validated objective tests. Studies were selected over a span of 17 years (from 2006 to May of 2023), since there was little information to be found over 5- or 10- years period. Studies were accepted whether the MDD+SUD and/or BD+SUD samples had been assessed independently, or in comparison with other samples such as control groups (CG) or groups with only one of the mental disorders.
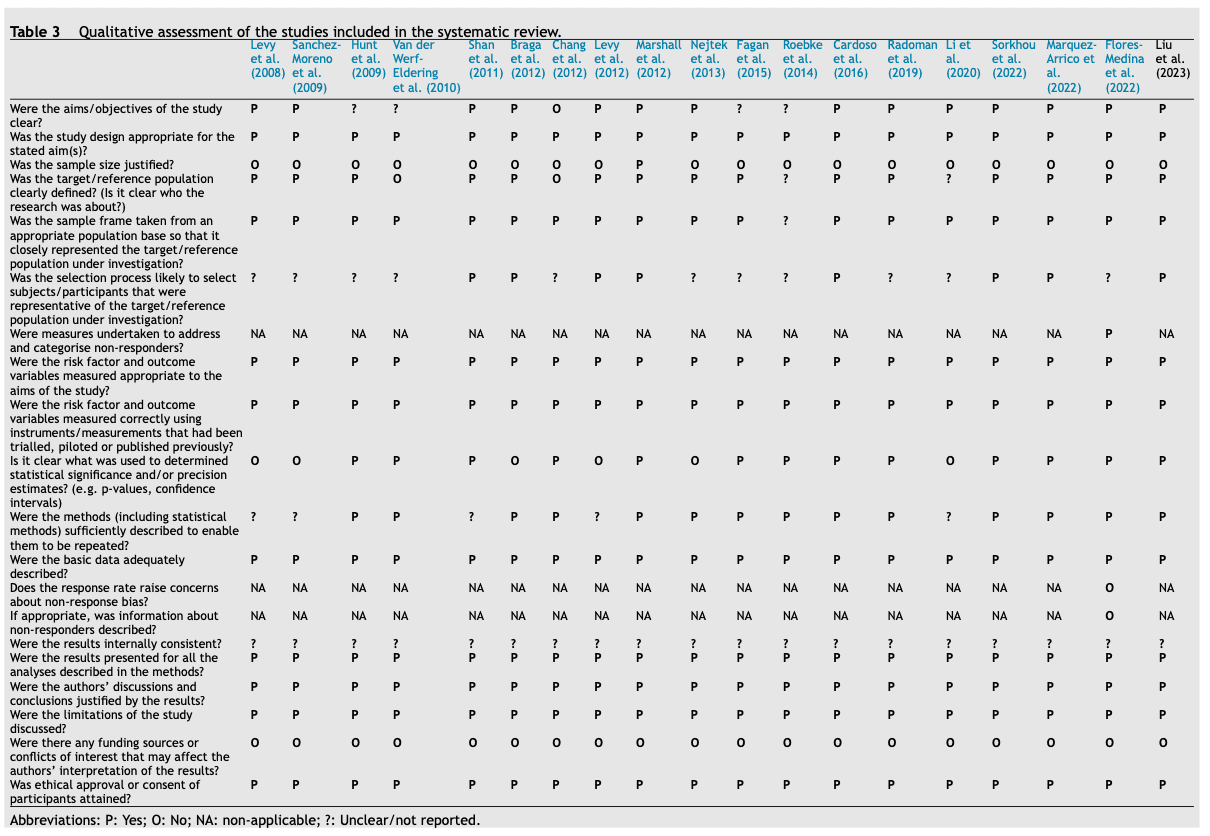
Two of the authors searched and selected the articles independently, and discrepancies were discussed between both authors. In this case, it was not considered relevant to assess the risk of bias because, due to the scarce information that can be found, no paper was excluded for quality reasons; therefore, this review primarily aims to describe the state of the research on this topic and to evidence the findings despite the limitations of the literature so far. All the studies included in the review were qualitative assessed according to the Appraisal tool for Cross-Sectional Studies (AXIS tool) from Downes et al. (2016). We did not perform a meta-analysis due to the high heterogeneity found across the studies in key methodological aspects such as age, sex, main substance, or assessed population, among others. This review was not previously pre-registered.
3. Results
As shown in the article selection flowchart (Fig. 1), 19 studies were finally elected for review according to our criteria. Among them, 13 assessed BD+SUD patients, five assessed patients filling the criteria for MDD+SUD and one included both diagnoses. The main substance of consumption was alcohol in ten studies (together with cocaine in one of them), cannabis in four studies, cocaine in two studies, and amphetamines in one study (together with cocaine). Three of the studies accepted any substance. All but five of these studies accepted polyconsumption of multiple illicit substances and three of them accepted alcohol consumption. A summary of all the chosen studies is presented in Table 2.
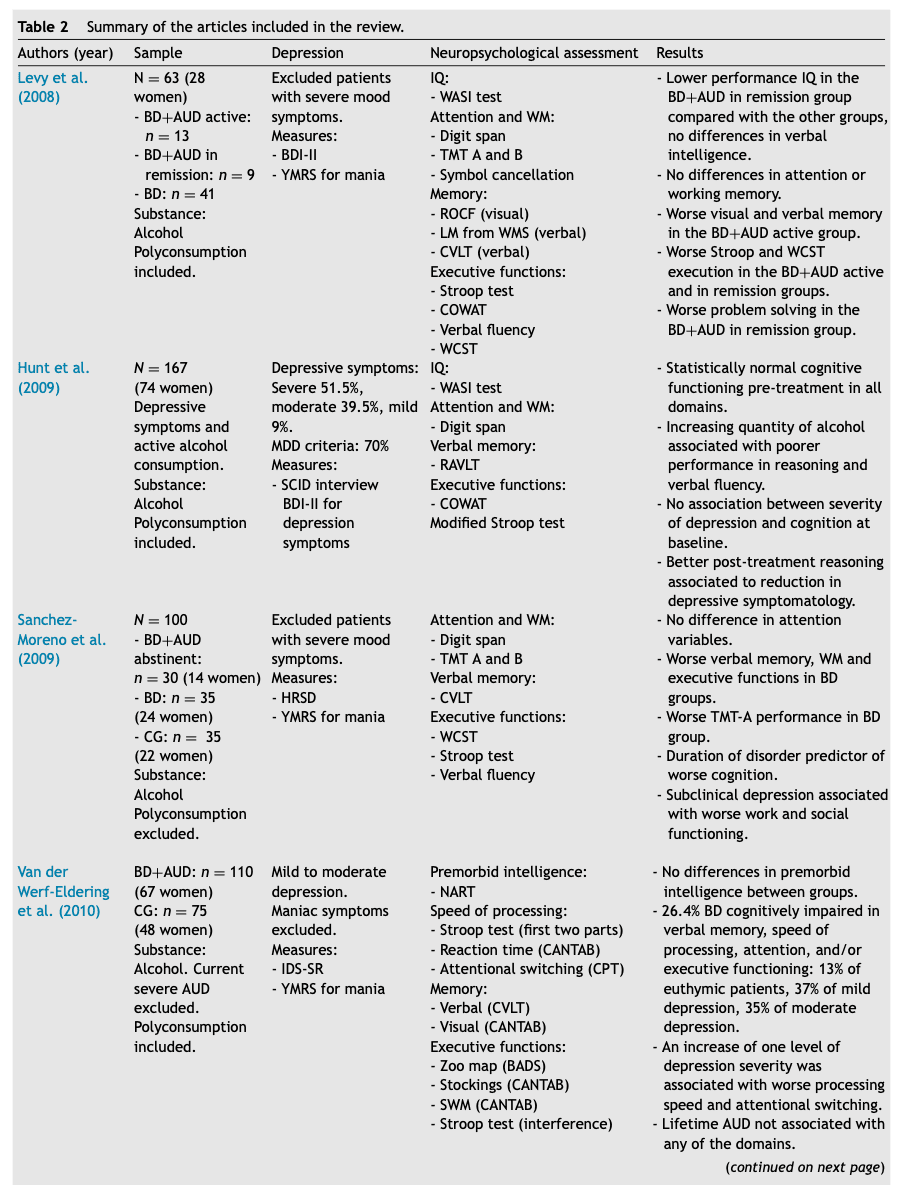
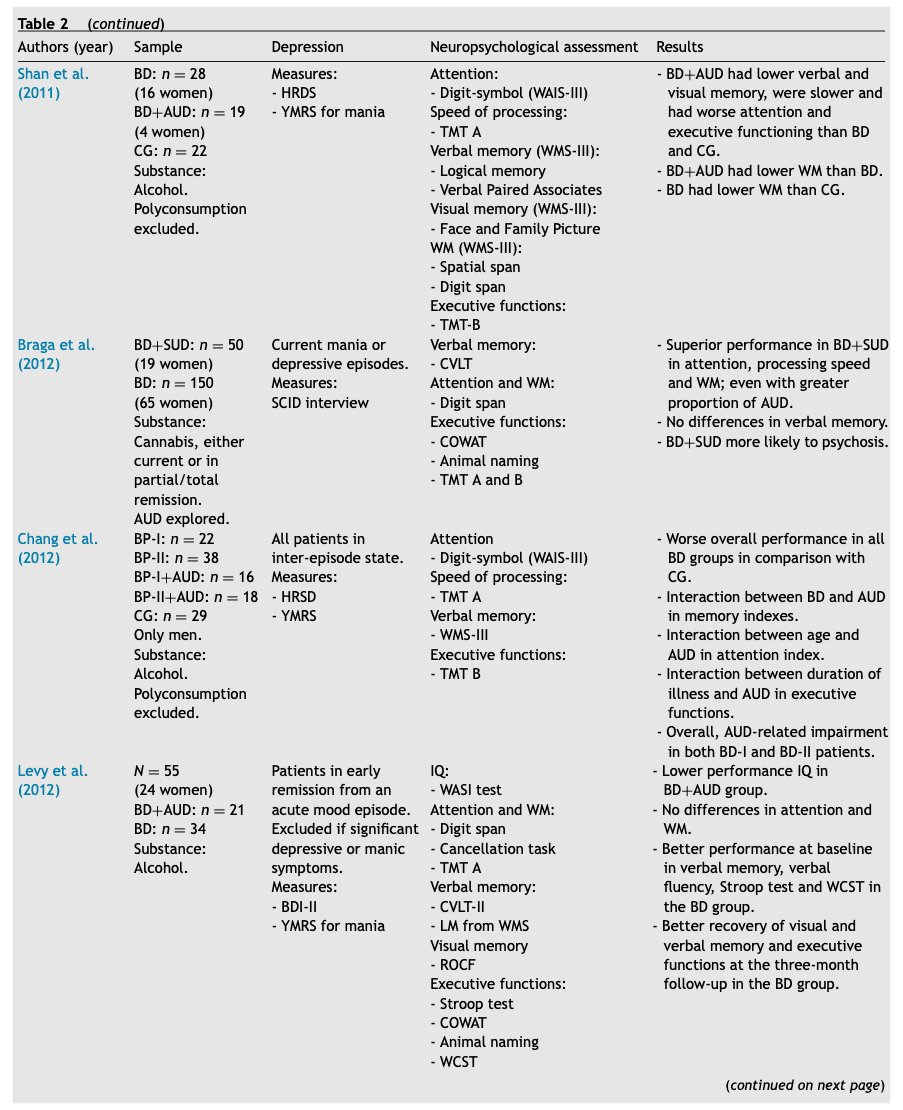
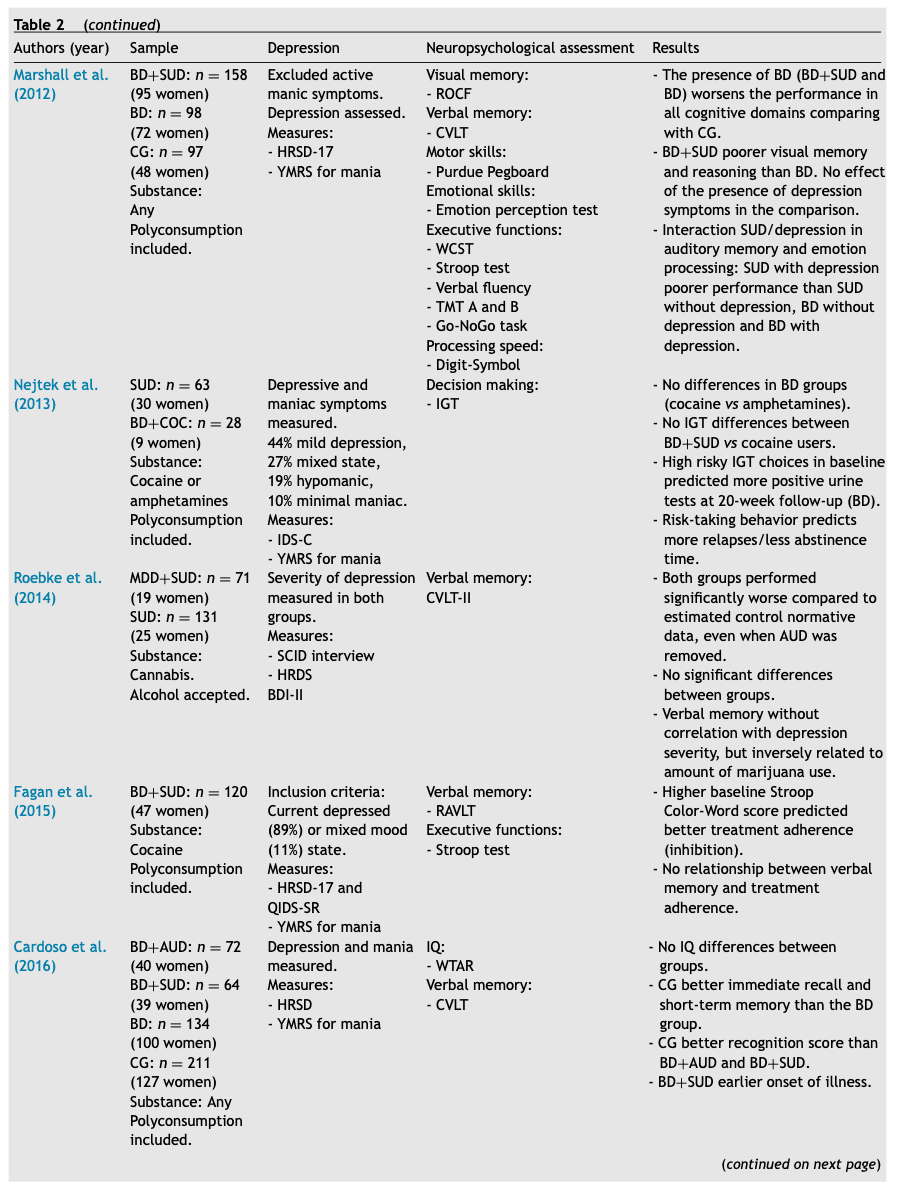
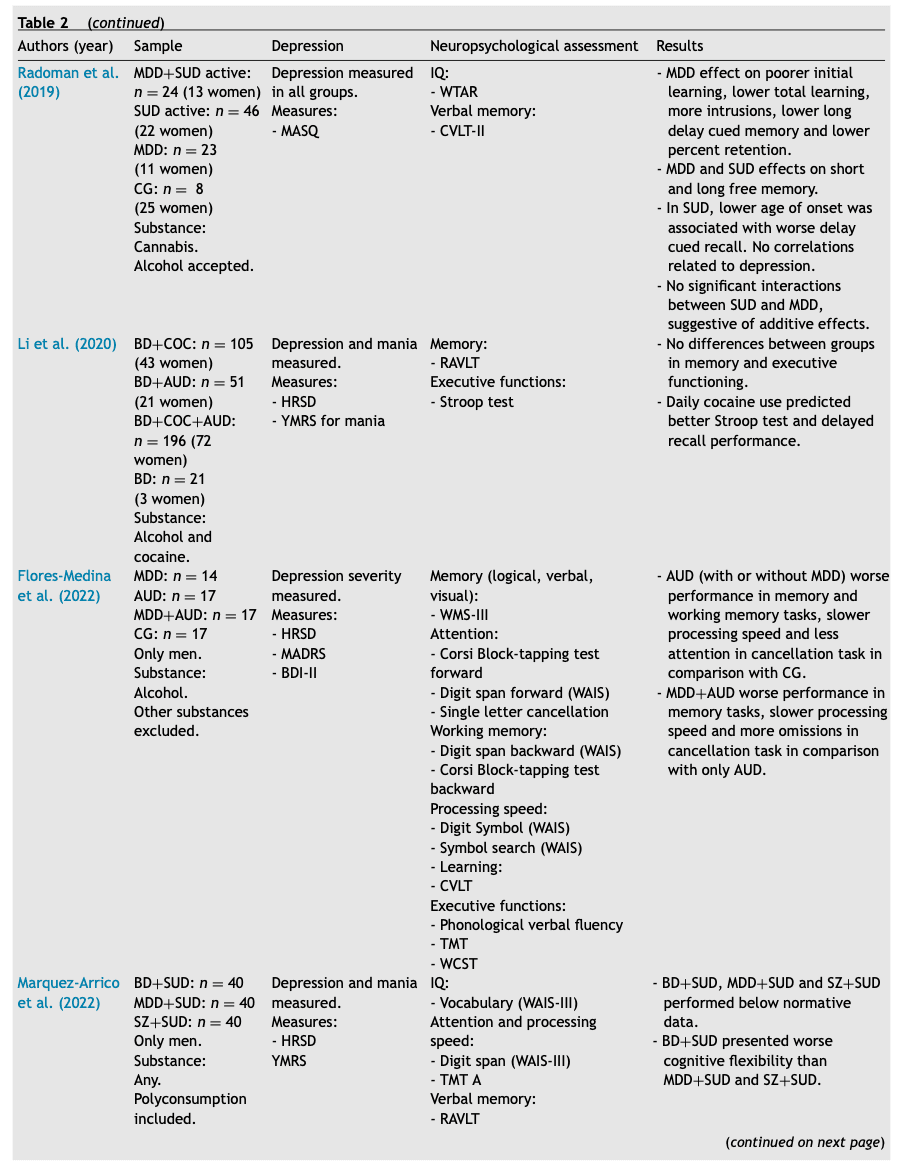
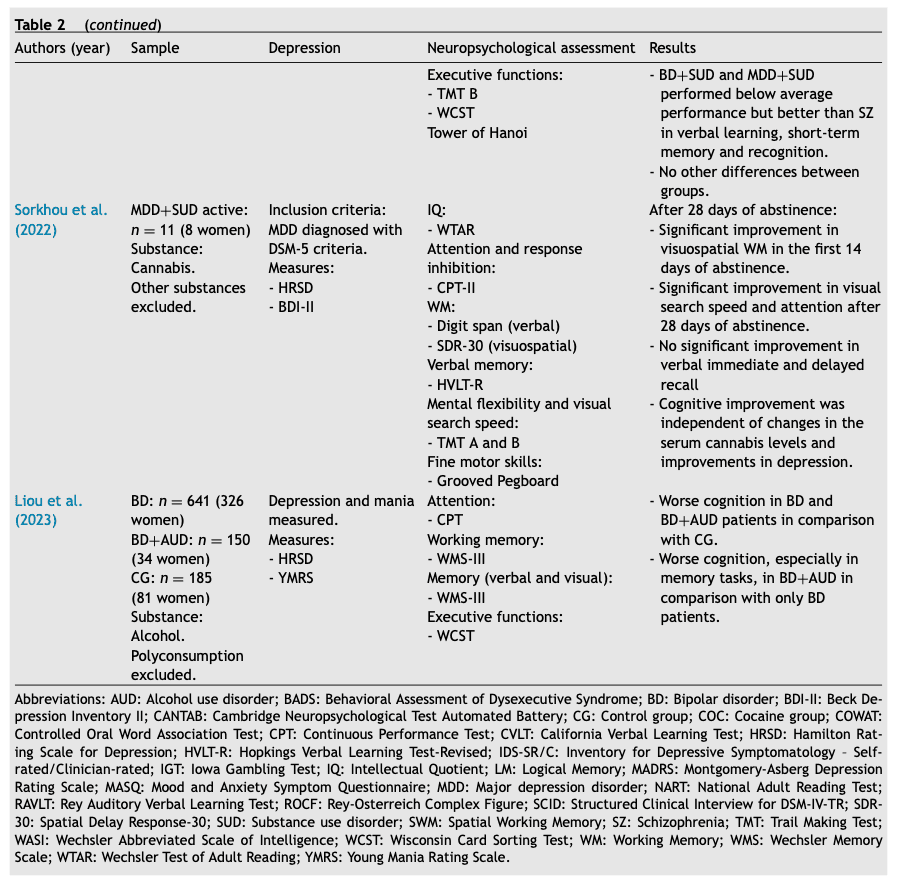
Due to the heterogeneity in the neuropsychological assessment and in the clinical variables analyzed, cognitive performance was divided into three categories to better understand the results: attention and processing speed, memory, and executive functions. Moreover, although not systematically, the assessement of the premorbid intelligence quotient (IQ) was also considered, and these data are presented in the first section. There were only four studies focusing on the effect of the MDD+SUD comorbidity, three of them with cannabis consumption, and in a large number of the BD+SUD articles the presence of depression was an exclusion criterion. However, depressive symptomatology was often measured, and the relation between its intensity and the cognitive impairment was also analyzed.
The qualitative assessment is presented in Table 3. Although none of the studies justified their size sample despite the fact all of them examined representative groups of their reference population. Furthermore, only one of the studies (Flores-Medina et al., 2022) worked with patients who were under a specific intervention (psychopharmacological) and had pre- and post- treatment measures. The majority of the reviewed studies described their methods sufficiently as to be repeated, but five of them presented their procedures in a very summarized form (Levy et al., 2008, 2012; Li et al., 2020; Sanchez-Moreno et al., 2009; Shan et al., 2011). Finally, none of the reviewed studies described the internal consistency of their results and they did not report sources of conflict of interest.
3.1. Premorbid intelligence quotient
In most cases, premorbid IQ was based on the Wechsler Abbreviated Scale of Intelligence (WASI), a short battery with 4 tests to measure fluid and crystallized intelligence through 3 indices: performance IQ, verbal IQ and full-test IQ. Some studies used different measures, such as the National Adult Reading Test (NART) or the Wechsler Test of Adult Reading (WTAR). Both tests assess vocabulary, a capability that is thought to resist many types of brain damage.
Among the studies that applied the WASI test, two of them found differences in premorbid IQ, with worse scores on performance IQ (considered a measure of fluid intelligence) in a group with BD+AUD compared to a group with BD-only (Levy et al., 2012), and in BD+SUD group in full remission compared to a currently active BD+SUD (alcohol as primary substance) and a BD group (Levy et al., 2008). Despite this difference, the score of the BD+SUD patients in remission was not below normality. A longitudinal study with women with depressive symptoms and active alcohol consumption found a normal premorbid IQ in these patients. However, it should be noted that patients who completed the study had a significantly higher premorbid IQ than those who did not complete it (Hunt et al., 2009).
One study using the NART test found no difference in premorbid IQ when comparing a BD+AUD group with a CG (van der Werf-Eldering et al., 2010). Moreover, a study using the WTAR test also found no difference either when comparing BD+SUD patients with BD patients and a CG (Cardoso et al., 2016), but another one found that MDD and MDD+SUD patients (cannabis with or without comorbid alcohol consumption) had a lower IQ than only SUD patients and a CG (Radoman et al., 2019).
3.2. Attention and processing speed
From all the studies, ten of them evaluated attention and/or processing speed in BD and four of them in MDD or other degrees of depression. Attention is frequently measured with the digit span subtest of the Wechsler Adult Intelligence Scale (WAIS) and, to a lesser extent, with the Continuous Performance Test. Only three of the studies, which compared BD+AUD groups with only BD and CG, found worse attentional performance in DD patients (Chang et al., 2012; Shan et al., 2011, Liou et al., 2023). Moreover, a study that evaluated cannabis consumers found that BD+SUD patients performed better than BD patients on the digit span test (Braga et al., 2012).
The tests used to assess processing speed vary across studies, and they are sometimes not specific to isolate this function, so the results may be overshadowed by possible impairments in other domains. For example, the TMT (Trail Making test) A and B or the Stroop test are usually considered measures of executive function, but sometimes they are also used to assess processing speed, so that only a specific part of each test is interpreted. In some cases, processing speed is not even measured, which seems surprising considering that, as previously mentioned, this is a domain that has been widely reported as impaired in BD and MDD patients. This heterogeneity is probably one of the reasons why the results in this domain are less consistent than in the others. Furthermore, just as in attention, only the studies carried out by Shan et al. (2011) and Chang et al. (2012) found that DD patients were slower than BD patients and CG. In fact, similarly to the attention results, the study with BD+SUD cannabis consumers found better processing speed compared to BD only (Braga et al., 2012), although the study by Sorkhou et al. (2022), also with cannabis consumers, seems to point towards an improvement in visual searching speed with 28 days of abstinence.
When considering depressive symptoms, one study found that increasing level of depression severity was associated with worse performance on processing speed and attention- switching tasks in BD+AUD patients (van der Werf-Eldering et al., 2010). Similar results were found in Flores-Medina et al. (2022), where MDD+AUD group performed worse on attention and working memory tasks, and was slower than a CG and an AUD only group. However, in a study with MDD+SUD using cannabis, abstinence was found to significantly improve sustained attention and visoespatial working memory with no assotiation with changes in depressive symptoms, suggesting that these aspects of attention were more conditioned by cannabis consume than by the presence of depression (Sorkhou et al., 2022).
3.3. Memory
Thirteen studies evaluated memory in BD, and six of them in MDD (often in both visual and verbal modalities). The memory domain is usually measured with the California Verbal Learning Test (CVLT), the Rey Auditory Verbal Learning Test (RAVLT), different tests of the Wechsler Memory Scale III (WMS-III) and the Rey-Osterreich Complex Figure for visual memory (ROCF). Most studies with BD+SUD patients observed a greater affectation of both visual and verbal memory in this group when compared to the CG or BD alone group, but not all the studies obtained these findings. Related to MDD, studies are mostly done with cannabis users.
Only two of the studies found worse verbal memory in BD patients compared with the CG, with no significant differences between the group with a history of SUD (mostly alcohol consumers) and those without it in one of them (Sanchez-Moreno et al., 2009) and with even worse performance in the BD+SUD (also alcohol consumers) in two of the studies (Chang et al., 2012, Liou et al., 2023). In the research carried out by Sanchez-Moreno et al. (2009), the BD+SUD group was already abstinent, and this may be the reason why no differences were found between both BD groups (with and without SUD). In this line, a study comparing cognitive performance in BD+SUD (mostly alcohol consumers, active and in remission) and in BD patients observed that only the group with an active SUD performed significantly worse than the other two in both verbal and visual memory (Levy et al., 2008). However, in another study it was observed that BD+SUD abstinent patients performed significantly worse on visual memory tasks compared to BD patients (Marshall et al., 2012). In the same study, when depression was considered, BD+SUD patients with a current depressive episode performed significantly worse on auditory memory compared to non-depressed BD+SUD and depressed SUD patients.
Nevertheless, there are some studies that found no differences in memory performance between BD+SUD and BD, or even obtained counter-intuitive results. For example, Braga et al. (2012) found that there were no significant differences in verbal memory, although it should be noted that the BD+SUD patients (cannabis consumers) were in partial or full remission, and the main substance was cannabis. Similarly, Li et al. (2020)found that there were no differences between alcohol- and cocaine-consuming groups and the BD group. Moreover, and unexpectedly, an increased frequency of cocaine use was associated to a better delayed recall in verbal memory tasks.
As previously mentioned, studies with MDD have mostly been found with concomitant cannabis use. In this case, studies did not yield clear results, but in general they point to some influence of depression on cannabis-related cognitive impairment when MDD is also present. One study found that verbal memory is only associated to the amount of cannabis consumed, but not to depression severity, when comparing an MDD+SUD group with a SUD-only group (Roebke et al., 2014). Another one found that both MDD and cannabis affect memory independently (learning, short term memory and long term memory), but found no interactions between SUD and MDD, suggesting a possible additive effect of these two disorders (Radoman et al., 2019). Finally, a study focusing on the effect of one month abstinence in a group of MDD+SUD (cannabis users) found that abstinence did not improve immediate and delayed verbal recall, suggesting that these aspects could be influenced by the presence of MDD (Sorkhou et al., 2022).
One of the studies (Flores-Medina et al., 2022) evaluated memory in MDD+AUD patients. In this case, this group performed worse on all memory tasks (verbal, visual and logical) in comparison with a control group and an AUD-only group. As an exception, one study measured verbal learning in all types of consumers with MDD+SUD (Marquez-Arrico et al., 2022). In this paper, performance on different cognitive tasks is measured comparing MDD+SUD, BD+SUD and SZ+SUD (comorbid schizophrenia). SZ+SUD patients performed worse than MDD and BD patients, but all three of them appeared to have a performance below expectations, according to normative data.
Finally, considering the different types of memory, Cardoso et al. (2016) found that the BD+SUD group performed worse than the CG in recognition and immediate recall task. No differences were observed between BD+SUD and CG in short memory tasks, in which only the BD group performed worse than the CG.
3.4. Executive functions
Twelve studies evaluated executive functions in BD, and four of them in MDD or other degrees of depression. Executive functions are classically defined as “the capabilities that are considered essential for performing efficacious, creative and socially acceptable behavior” (Lezak, 1976). They englobe multiple abilities in which the frontal lobe plays a significant role and, because they do not usually act independently one of each another, they frequently overlap. As a result, there is no single way of evaluate evaluating the executive functions, so the studies vary depending on the assessed capabilities and the neuropsychological tests selected. Some studies reported a general worse performance in executive functions-related tasks in BD groups, both with and without SUD (Marshall et al., 2012; Sanchez-Moreno et al., 2009). Similar results were obtained when comparing a sample of BD+AUD patients, where 72% of the sample had significant depressive symptoms (37% mild depression, 35% moderate depression), with a CG (van der Werf-Eldering et al., 2010). More specifically, one study found worse general executive functioning (with measures of working memory and cognitive flexibility) in BD+AUD patients (Shan et al., 2011).
However, when analyzing different capabilities independently, some studies found specific impairments in the DD groups. Response inhibition, measured with the Stroop test, is one of the executive functions most frequently assessed in the field of addictions. In relation to this, one of the studies (Levy et al., 2008) found a worse overall performance in the BD+AUD group (polyconsume included) with active consumption and in remission. However, it is not mentioned in which Stroop subtest they performed worse, so this performance might also be attributed to impaired processing speed. The same author, in another study comparing a BD group with a BD+SUD group (cannabis with or without alcohol consumption) in early remission of a mood episode (Levy et al., 2012) found that response inhibition was worse at the moment of hospital discharge in the BD+SUD group, and that they also had worse recovery of this function at the 3-month follow-up. On the other hand, another study obtained that, in a group with BD+SUD cocaine consumers (polyconsume included), a higher baseline score on the Stroop interference subtest predicted better treatment adherence, suggesting that a lack of response inhibition could interfere with treatment prognosis (Fagan et al., 2015). Another frequently measured executive function is cognitive flexibility, usually with the Wisconsin Card Sorting Test (WCST). In this line, worse cognitive flexibility was found in the BD+SUD patients with active consumption and in remission (Levy et al., 2008) and in BD+AUD patients (Liou et al., 2023) when compared to BD-only patients. Finally, BD+SUD patients compared to MDD+SUD patients, with more than three months of abstinence and mostly polyconsumers, showed worse cognitive flexibility (Marquez-Arrico et al., 2022).
In the field of addiction, it is also common to assess the risk-taking and decision-making behaviors with the Iowa Gambling Test (IGT). However, only one study assessed this domain in the articles included in this review (Nejtek et al., 2013), where it was found that a higher risk-taking behavior at baseline predicted more relapses at a 20-week follow-up in BD+SUD (cocaine) patients, but not in SUD-only patients.
Finally, although not as clearly as in the previously described functions, reasoning (measured with one of the subtests of the WASI test) also appeared to be impaired in DD. Specifically, in a cohort of depressed patients with active alcohol consumption (where 70% of the sample met the criteria for a MDD diagnosis), there was no association between severity of depression and cognition, but a decrease in symptomatology was associated to a better post-treatment performance in this capability (Hunt et al., 2009).
4. Discussion
Our review suggests that MDD+SUD or BD+SUD may independently enhance the cognitive impairment found in each comorbid disorder. This finding is not surprising considering the significant neurobiological overlap between SUD, MDD and BD. When SUD begins to develop, the frequent drug consumption provokes a dysregulation of glutamatergic, GABAergic and dopaminergic networks in the prefrontal cortex (PFC), which mainly controls executive functions (Koob and Volkow, 2016, Uhl et al., 2019).
In the case of MDD, when a stressor becomes chronic, cortisol levels increase and this can cause an impairment in areas such as the hippocampus, amygdala and PFC. Moreover, the presence of depression has been associated with reduced gray matter volume in the latter area (Dean and Keshavan, 2017, Li et al., 2020). Similarly, studies in BD have found morphological abnormalities in dorsolateral PFC and a moderate dysfunction in this area when executing tasks related to it (tests involving problem solving, decision making) (Scaini et al., 2020, Young and Juruena, 2021). The functions more sensitive to this enhancement are immediate and short-term memory (both visual and verbal), as well as executive functions such as response inhibition, cognitive flexibility, and risk-taking behavior. Specifically, and although contradictory results are found in almost all areas, BD could worsen attention, processing and speed and executive functions (cognitive flexibility, response inhibition and decision-making); whereas depression could affect attention, processing speed, memory and executive functions such as reasoning.
These results are in concordance with those suggested in previous BD+SUD reviews (Gogia et al., 2022), but which are new in the context of MDD+SUD. Particularly, the impairment in executive functions may lead to an affectation of treatment-related variables, such as less adherence or more relapses. Some results, on the contrary, may suggest a lower vulnerability in dual patients, at least in the context of cannabis consumption, although this finding is not systematically replicated in all cannabis studies and further research is required.
This review also evidences the lack of literature on MDD and depressive symptomatology regarding cognitive functioning in DD, despite the high prevalence of MDD+SUD comorbidity and the widely known cognitive impairment related to both disorders. Furthermore, even when only BD is considered, the presence of a depressive episode is frequently a cause for exclusion, which makes it difficult to explore the potential impact that these symptoms may have on the functionality of the patient. Due to the potential disability that MDD and depressive episodes or the symptomatology of BD can produce, this field should be explored in future research to further describe the profile of these patients and provide insight on the best way to manage clinical interventions.
Although some studies show evidence of the potentiating effect of depression on SUD, it is difficult to draw generalizable conclusions. One of the most important limitations of the research made to date is the lack of a unified standardized protocol used for cognitive assessment. Firstly, regarding the neuropsychological exploration, there is a high variability in the explored domains and, even in studies in which the same domains are explored, the chosen tests may be different or are interpreted differently. Moreover, there are some cognitive domains that may be relevant to evaluate in the light of new evidence, such as social cognition in DD or visuospatial skills in AUD (Ros-Cucurull et al., 2018), as they can potentially interfere with recovery and treatment (Lewis et al., 2020; Ramey & Regier, 2019; Winters et al., 2021).
It is important to consider the variables related to the treatment and the disorder are not always controlled and this can affect the interpretation of the results. For example, a study (Li et al., 2020) found a better cognitive performance in cocaine consumers, but two aspects of the sample selection have to be taken into account. The first is that some subjects might have recently consumed cocaine, and the second is that BD patients were not necessarily euthymic and therefor they could present some grade of depressive or manic symptoms. These two aspects could make it difficult to isolate the effects of substance consumption or those of BD symptomatology.
An important and not always controlled factor is whether subjects are assessed while in active drug use or abstinent. In this second case, abstinence is not systematically described when selecting patients for the sample. Only one study (Levy et al., 2008) specifically compared a group of DD with active consumption with another in remission, but even in this study the period of abstinence was not considered. Among the SUD-related literature, there is a great evidence of the influence of abstinence time on the cognitive functioning of subjects. Most studies have observed that a longer time of abstinence predicts, at least, a mild improvement in cognitive functioning in cocaine, cannabis, alcohol, and amphetamine consumers. These effects, overall, may not be seen at early abstinence, but start to be evident at approximately 3-5 months of abstinence (Almeida et al., 2017; Potvin et al., 2014; Ros-Cucurull et al., 2018; Schulte et al., 2014; Tang et al., 2019), with different results depending on the type of substance. On the other hand, executive functions frequently remain impaired even after 6 months of abstinence in SUD, and this has been linked to a worsening in clinical variables such as treatment adherence and the number of relapses (Rezapour et al., 2021; Verdejo-Garcia et al., 2019). Assessment of the cognitive profile both at baseline and at a long-term follow-up could be helpful in providing information on how to personalize the intervention (Duijkers et al., 2016). The influence of abstinence time (days, months…) in the cognitive performance of patients with DD is an unexplored field that should be considered, taking into account that these patients are potentially more impaired than those with SUD-only.
The lack of analysis of disorder-related variables was another source of heterogeneity among the reviewed studies. It is known that an early onset of a SUD or a MDD/BD is associated with a worse prognosis of the disease (Blanco et al., 2012; Cichon et al., 2020; Herzog et al., 2021; Wolter, 2018), but this factor was not considered in the reviewed studies, and this may have masked some differences among the groups. There is an exception in the study by Sanchez-Moreno et al. (2009), who observed that the duration of the disorder was the best predictor of an impairment in the cognitive functioning of the BD+SUD patients. Additionally, whenever possible, the main substance of consumption should also be considered in the assessment and interpretation of cognitive results. However, the most common pattern is polyconsumption. Therefore, future studies should take this variable into account, since it has been found that there are different cognitive profiles affected when different substances are compared, even among polyconsumers, depending on different clinical variables (Capella et al., 2015). In fact, this is an additional evidence of the lack of heterogeneity in the MDD+SUD literature, as all the studies in the review that specifically addressed this comorbidity were in association with cannabis consumption.
There are also other unexplored factors that should be of interest to complete the profile of cognitive functioning in DD. Among these, there is a growing need to introduce the gender perspective and the influence of circadian rhythms, not only as potentially confounding factors of the existing data, but also as variables to be considered for the improvement of the clinical management of DD patients in the future.
Sex is a demographical variable always collected but not frequently analyzed independently in the literature on SUD and DD until a few years ago. Regarding SUD characteristics for female population, multiple sociocultural factors make SUD women less prone to seek treatment and more susceptible to the negative consequences of addiction, such as homelessness, social exclusion and a lower quality of life(Greenfield et al., 2007; McHugh et al., 2018). The BD-related literature points to an increased number of depressive episodes (Arnold, 2003; Pillai et al., 2021) with greater severity, as well as more relapses and more treatment resistance in women (Hyde & Mezulis, 2020; Otte et al., 2016). In the context of DD, the comorbidity of MDD+SUD has also been found to be twice more frequent in women than in men (Tirado Muñoz et al., 2017). In this regard, Gabriels et al. (2019) refer that in their sample DD is more common in women, and more associated with suicidal ideation, than in men. Another study finds a stronger association between harmful AUD and an increase in the severity of depression, but only in women (Pavkovic et al., 2018). Considering all this and the fact that none of the reviewed studies analyzed or described sex differences regarding cognitive performance, even if in almost all cases patients of both sexes were included, there is a broad field yet to be explored in this context.
Another novel approach in DD is the study of circadian rhythms. The disruption in circadian rhythms has been observed in BD, MDD, SUD and even DD (Daut & Fonken, 2019; Hashemzadeh et al., 2021; Melo et al., 2017; Serrano-Serrano et al., 2021), suggesting a worse functional prognosis in patients with greater circadian disruption. Similarly, it is known that irregular habits, less exposure to light or the presence of sleep disturbances worsen cognitive performance or accelerate cognitive decline (Diago et al., 2018; Law & Clow, 2020; Zimmet et al., 2019). Therefore, it may be interesting to go a step further and explore how circadian rhythms can affect cognition in patients with DD across their recovery, considering both early and late remission.
In conclusion, research points to worse memory and executive performances in DD patients with comorbid BD and/or depressive symptomatology, when compared to CG, SUD, BD and MDD patients. These may also be involved in the impairment of attentional and processing speed functions, although contradictory results have been found in these areas. Therefore, it seems necessary to develop future studies to overcome the current limitations and to consider additional key factors, such as abstinence, type of substance or years of addiction, that seem to be related to the cognitive affectation found in BD+SUD and MDD+SUD patients. Such further research would contribute to increase our theoretical knowledge, as well as to improve the personalized clinical approach in the treatment of these patients, including the possibility of cognitive rehabilitation in those who need it. Given the association of cognitive deficits in SUD patients with the lack of treatment adherence and incresing relapses, research in this line would help to alleviate the effects of a possible increase in this impairment in DD patients, thus contributing to a better treatment prognosis in this population.