Abstract
Intro: In recent years, there has been a dramatic increase in overdose deaths involving illicitly manufactured fentanyl. The risk of death due to fentanyl exposure is far higher for people without adequate tolerance, such as those being released from incarceration. However, little is known about knowledge and perceptions of fentanyl among people who are incarcerated. Methods: We conducted 40 semi-structured qualitative interviews with people who were incarcerated at the Rhode Island Department of Corrections (RIDOC). We explored the impressions of, preferences for and experiences with fentanyl among these people. Analysis employed a general, inductive approach using NVivo 12. Results: We found that a majority of the participants were familiar with fentanyl, sought to avoid it and utilized harm reduction techniques when using drugs and taking treatment with medication for opioid use disorder (MOUD) to reduce their risk of overdose. Discussion: Our findings suggest that broad access to MOUD, especially for incarcerated people, is increasingly necessary in the era of fentanyl, both to aid people seeking recovery due to the increased overdose risk of drug use and to reduce overdose morbidity for people who use drugs.
1. Introduction
The opioid overdose crisis led to the death of over 93,000 people in the United States (US) in 2020 alone (Ahmad et al., 2021). From 2019 to 2020, provisional data indicate that overdose deaths increased by more than 20% across the US (Ahmad et al,. 2021).
The increased lethality of the illicit drug supply has been a key driver of the increased overdose risk (Ahmad et al., 2020). From 2013 to 2019, overdose deaths involving synthetic opioids (primarily, illicitly manufactured fentanyl and fentanyl analogues) increased nearly 12-fold, and in 2019, over half of all overdose deaths involved synthetic opioids such as fentanyl (Mattson et al., 2021). Rhode Island has been especially hard hit by the opioid crisis, particularly due to fentanyl (Drug Overdose Deaths, Rhode Island Department of Health). In 2018, over 70% of Rhode Island’s 308 overdose deaths involved fentanyl (Drug Overdose Deaths, Rhode Island Department of Health), on par with the national trend for that year, and 2020 had the highest overdose deaths to date, most involving fentanyl (Ahmad et al., 2021, Wilson et al., 2020).
People involved in the criminal legal system are among those most impacted by the opioid crisis (Binswanger et al., 2007, Gan et al., 2021, Macmadu et al., 2020, Merrall et al., 2010, Victor et al., 2021). In 2014 and 2015, before establishment of the comprehensive MOUD program in the Rhode Island Department of Corrections, over 21% of people who experienced a fatal overdose in Rhode Island had been incarcerated in the two years prior to death (Brinkley-Rubinstein et al., 2018). Additionally, it is estimated that over a third of all people with opioid use disorder experience involvement in the criminal legal system during their lifetime and those with recent or repeated involvement are at a greater risk of fatal overdose upon re-entry (Binswanger et al., 2007, Binswanger et al., 2016, Merrall et al., 2010, Saloner et al., 2020, Victor et al., 2021).
In response to the worsening opioid crisis and its disproportioned burden on people in the criminal legal system, in 2016 the Rhode Island Department of Corrections (RIDOC) implemented the first state-wide program to provide access to all three Food and Drug Administration-approved medications for opioid use disorder (MOUD; including methadone, buprenorphine, and naltrexone) to all people incarcerated with opioid use disorder (Clarke et al., 2018). MOUD are considered the gold standard of care for people with opioid use disorder (National Academies of Sciences & Medicine, 2019). Despite extensive documentation that MOUD dramatically reduces mortality among people who use illicit opioids, it is rarely available in correctional settings (“JPOP” 2021, Nunn et al., 2009). Preliminary evaluation of the MOUD program at the RIDOC revealed a reduction in overdose deaths among people who were released from incarceration (Green et al. 2018).
Although illicitly manufactured fentanyl and fentanyl analogues have contributed to rising rates of overdose death across the country, there are few studies that explore perceptions of and preferences for fentanyl among people most directly impacted by the crisis. Previous studies have explored perceptions of fentanyl among street-recruited people who inject drugs, among youth, and among people receiving methadone in the community (Afrken et al., 2017, Arunogiri et al., 2020, Buresh et al., 2019., Daniulaityte et al., 2019, Macmadu et al. 2017, Stone et al. 2020, Morales et al. 2019, McLean et al. 2019). However, to our knowledge, no previous study has explicitly explored the experiences and perceptions of fentanyl among people incarcerated. Previous literature has not always controlled for criminal legal involvement, thus previous research may include findings from individuals with similar incarceration histories to those represented in our study. However, given our participants current status as incarcerated, they may not have the same awareness of changes in the drug market and protection tactics as people in the community. Fentanyl, and other illicit substances, have been identified in prison and jails, and even though the extent and access to drugs is still limited, they are at an increased risk of fatality from OUD due to the increasing lethality of the opioid market (Binswanger et al., 2020; Kaplowitz et al., 2021).
2. Methods
2.1. Participant Recruitment
We conducted 40 semi-structured, qualitative interviews with incarcerated persons at the RIDOC between July and August 2018. The RIDOC is located on a central campus in RI and is a unified system that is comprised of a statewide jail as well as several buildings of varying security levels on the same campus. Eligible participants were 1) over the age of 18, 2) able to read and write in English, and 3) enrolled in the MOUD program at the RIDOC. More detailed methods have previously been published (Brinkley-Rubenstein 2018).
Participants were recruited from jail (n=10), minimum (n=9), medium (n=9), and women’s (services pre-trial and sentenced women, n=12) prison facilities at group addiction counseling sessions, which are required for continued enrollment in the RIDOC MOUD program. During these group counseling sessions, the study was introduced and described by two research assistants. Participants were able to sign up confidentially and were later contacted for an hour-long interview in person. Both interviewers had prior training in qualitative interviewing, experience conducting interviews in a criminal legal setting and were well versed gaining rapport and working with people who are incarcerated.
2.2. Data Collection
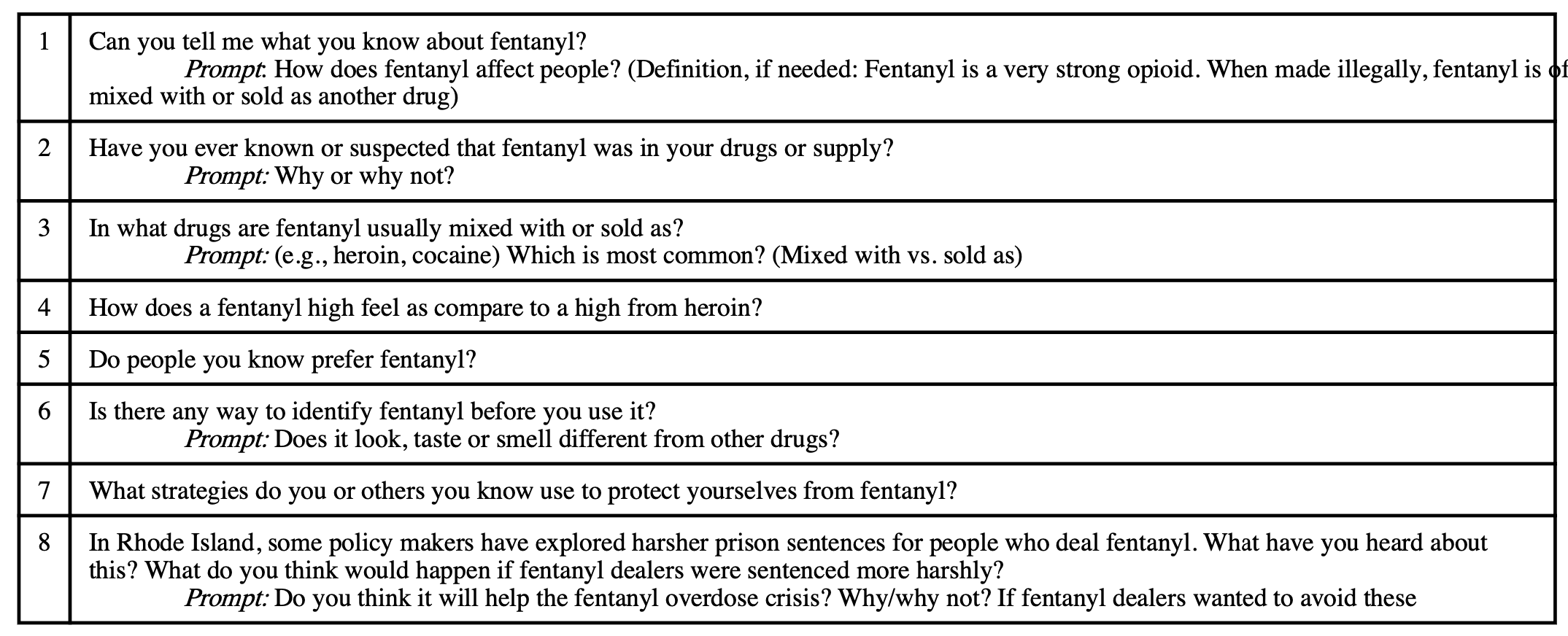
The interviews were conducted in a private room, without correctional officers present. The interviews were semi-structured and explored a range of topics including participants’ experiences with and attitudes toward illicitly manufactured fentanyl and impressions of MOUD. See Table 1 with the relevant interview questions. The full protocol is available upon request to the corresponding author. The interviews averaged an hour in length and were digitally recorded. The recordings were later professionally transcribed. Study participants received $25 for their participation that was deposited directly into their commissary account. The study was approved by the Miriam Hospital’s Institutional Review Board, the Office for Human Research Protection (OHRP), and the RIDOC Medical Research Advisory Group.
2.3. Data analysis
Analyses employed a general inductive approach, and the research was divided into codes aligned with both the research objectives and interview questions (Thomas, 2006). The coding team consisted of five people trained in qualitative research analysis who developed and utilized a codebook that corresponded with our study objectives. To ensure coder agreement and consistency, four interviews were cross coded by all the team members to further refine and add to the codebook. Text segments could be double coded if they included data relevant to multiple codes. Once the codebook was finalized, three team members coded the remaining transcripts. Each transcript was coded independently by two coders, examined for agreement and discrepancies resolved by a third coder. Final coding was completed in NVivo 12 (Brinkley-Rubenstein et al., 2019). Coding queries were used to build content themes around fentanyl impression and preferences. The present manuscript explores the following codes: fentanyl, fentanyl overdoses experience, safer fentanyl use, fentanyl prevalence, fentanyl preferences, fentanyl knowledge, fentanyl identification. The major themes deduced from these codes are identified as headings in the succeeding results.
3. Results
3.1. Participant Characteristics
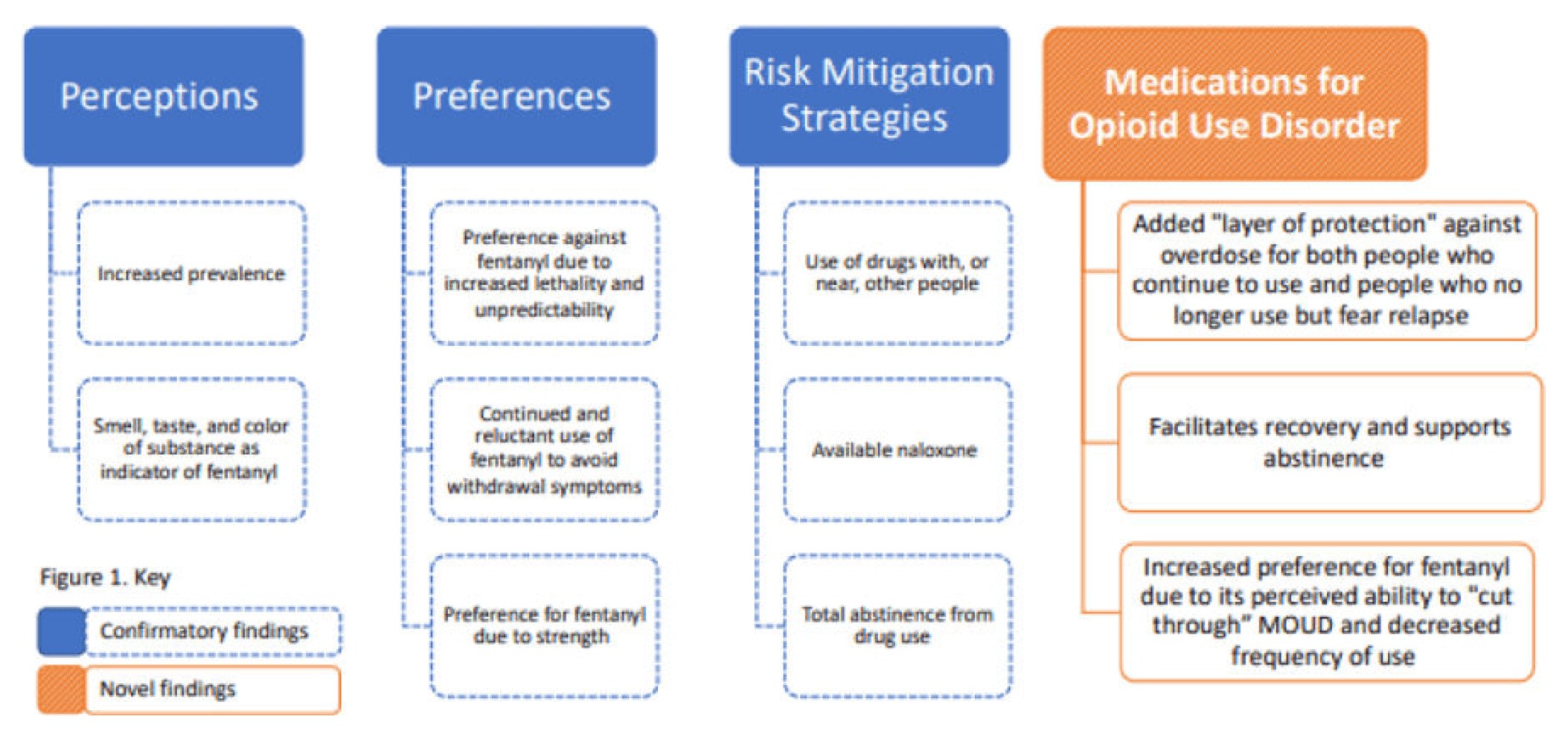
Participants were representative of the demographic makeup of the RIDOC. The participants ranged from 22 to 66 years old, with a mean age of 37. The majority of the participants were male (70%; n = 28) and white (83%; n = 33), and only 5% (n = 2) were Black, 13% (n = 7) identified as belonging to an “other” racial group, and 10% (n = 4) were Hispanic. The majority of participants (95%; n=38) reported using heroin prior to their incarceration and 75% (n = 30) reported using prescription opioids non-medically. More detailed participant characteristics have been previously reported (Brinkley-Rubinstein et al., 2019). Figure 1 summarizes the key findings (Figure 1)
3.2. Fentanyl Perceptions
The vast majority (98%; n=39) of participants expressed having some prior awareness of illicit fentanyl, either from personal experience, friends or media coverage. While the participants broadly concurred on the risks and morbidity associated with illicit fentanyl use, there were notable variations in participants’ attitudes, characterizations, and experiences with illicit fentanyl.
Out of the 40 total participants, 26 (65%) used “dangerous” (or a synonym such as “deadly” or “risky”) when describing fentanyl. A 36-year-old male, “Mark,” described fentanyl as “much stronger than heroin and very dangerous.” Like Mark, the majority of participants (n=24) utilized comparisons with other opioids to describe the uniquely high potency of illicit fentanyl.
3.2.1. Prevalence
Most participants believed that illicit fentanyl was becoming more prevalent and increasingly mixed or “cut” into other substances. While participants noted that fentanyl was most often found in heroin, many suggested that it could be found in many other illicit drugs. “Kate,” a 29-year-old female, articulated this sentiment succinctly, “usually, it’s mixed with heroin. Now, they put it inside Percs, [illicitly manufactured counterfeit oxycodone (Percocet) pills] and people are making it and they’re putting it inside the crack. It’s in everything.”
Mark suggested that the influx of fentanyl has made it increasingly difficult to avoid: “nowadays I think it’s almost impossible to get heroin without fentanyl.” Some participants even declared it impossible to access ‘pure’ drugs that did not contain fentanyl. “Robert,” a 41-year-old male who typically uses heroin shared, “There’s no true heroin out there anymore. Everything is tainted with that fentanyl shit…I think it’s in everything. It’s a scary prospect.”
Increased experiences, both personal and witnessed, with overdoses were attributed to an increase in the prevalence of fentanyl. While some spoke about the relationship between fentanyl and overdose generally, others, like Sarah, a 30-year-old female who typically uses heroin and cocaine, shared her personal experience, “they’re just like putting fentanyl in everything so I’ve been overdosing a lot.”
3.2.2. Identification
Participants utilized a variety of strategies to identify fentanyl. These strategies included examining the drug’s appearance and taste. Some participants shared how they used the color of the heroin to determine if it was fentanyl contaminated: “usually in the dope it’s – the dope’s a lot lighter because the fentanyl is like a whitish. So, it makes the dope a lot lighter. Usually dope’s like a tan color,” (“Steve,” a 31-year-old male who used heroin). Because of fentanyl’s white coloring, some believed that they were able to identify fentanyl-contaminated heroin when the drug appeared a lighter shade of tan.
Some participants shared how the scent and flavor of the substance could also be used to determine if fentanyl was present. “Daniel,” a 28-year-old male who used cocaine, for example, tasted his cocaine:
If you smelled it and it smells like a sweetness smell –its [fentanyl’s] sweet. I don’t know how it got that taste to it, but it’s sweet; so, it gives you a sweetness taste, then you know fentanyl’s in it.
While many employed these identification strategies to predict the presence of fentanyl, there was generally an accompanying acknowledgement that these precautions were not foolproof: “There’s really no way [to be sure] because the amount of fentanyl it takes for you to get high or even kill you is so small that you can’t even see it,” (“John,” a 26-year-old-male). Many participants agreed that there was no definite way to know if fentanyl was present in one’s drug supply using these methods.
In fact, despite utilizing these identification strategies, numerous participants recounted prior fentanyl-related overdoses. In many cases, the fentanyl was only identified retrospectively. For example, “Betty,” a 52-year-old female shared:
I went out to buy a Percocet 30 and I got a laced [counterfeit pill with fentanyl] Percocet and the doctor identified it with that. He said ‘how long have you been taking fentanyl?’ and I said never. He said ‘well, you’ve got fentanyl in your body.’ That’s what I took. I overdosed on fentanyl and never knew it. He said ‘It’s like 100 times greater than the other drugs and nobody knows that.’ I said I didn’t know it either.
It was common for people to be unaware of fentanyl in their drug supply unless notified by a clinician or through community supervision and toxicology screening, long after having used the substance. “Andrew,” a 36-year-old male shared his experience:
I wouldn’t have known. I didn’t know until it came out on the UA [urinalysis]. ‘You know you have fentanyl in your system.’ How did that happen?
3.3. Use preferences
Participants’ preferences regarding fentanyl were highly polarized, with most expressing dislike of fentanyl and a desire to avoid it. Specifically, people whose drug of preference was heroin often disliked the shorter duration of drug effects associated with fentanyl, which induced faster withdrawals and led to more frequent use.
Despite dislike of fentanyl, people continued to use it to avoid withdrawal symptoms: “I don’t really use any strategies to protect myself. If that’s what they have, it’s what they have. It’s what I do to not be sick,” (“Brianna,” a 33-year-old female who used heroin). For some, the overdose risks associated with fentanyl were minimal compared to the pain associated with withdrawal if they decided to avoid it: “being an addict, you know, you don’t have too many choices like especially if you’ve already bought it and you’re guessing. Well, you taste it, you know, and you’re like oh is there fentanyl in it? Yes, well probably. Well, I’m getting sick. So, it is what it is,” (“Steve”). Aware of the risks of fentanyl, but reliant on it to avoid withdrawal, some people shared a sense of fatalism in what felt like inevitable exposure: “Just try to use a little bit amount and pray that that little bit won’t take you out really, because there really is no amount to stop you from ODing [overdosing],” (“Jose,” 60-year-old male).
3.4. Strategies to mitigate overdose risk
In addition to the identification techniques utilized prior to use, some participants also engaged harm reduction techniques to reduce the risk of overdose when using drugs that were suspected to contain fentanyl. These techniques included carrying naloxone and using in the presence of others. A 32-year-old female shared, “I carry Narcan everywhere. We always have Narcan everywhere.” Others shared that they used slower than they normally would, or they started with smaller doses to see how the supply affected them: “[I] do a tiny bit at a time. That’s the only thing I know; just do a little bit to see how it is” (“Michael,” 34-year-old male).
While these strategies provided some participants with a sufficient sense of security to continue to use despite their fears of overdose, for others, these measures lacked reliable protection and led them to abstinence. “Jose” shared:
Since that fentanyl came out — This is why I left drugs. I thank God that it switched because I love heroin to be honest with you. Heroin is my choice of drug, but ever since they came out with this poison that’s killing people. I don’t want to be part of the statistic. I don’t want to die like that. Bad enough I’m killing myself. I just don’t want to just die like that.
Even though many people continued to use fentanyl despite these risks, many agreed that avoiding drug use was the only dependable way to eliminate fentanyl’s overdose risk. As “Stephanie,” a 34-year-old female shared, “my strategy is just to stay the hell away from it; all of it.” This was echoed by others: “Just don’t do it. That’s the best thing I can say,” (“Dejuan,” a 35-year-old male) and “I just don’t use; that’s my strategy,” (“Rachel,” a 47-year-old female).
3.5. Relationship between MOUD and fentanyl
The people interviewed were all enrolled in the RIDOC MOUD program, where they were receiving treatment that included methadone, buprenorphine or naltrexone under the care of a health professional. While participants’ motivation for MOUD use varied, as did their illicit substance use while receiving MOUD, the reduction of overdose risk while receiving MOUD emerged as a core rationale for program participation.
3.5.1. MOUD use to reduce risk of fentanyl exposure
Many people shared that they sought out MOUD to reduce the risk of overdose. While some used MOUD to cease drug use and eliminate the risk of overdose altogether, others used MOUD to decrease the risk of overdose while continuing to use. Fears of fentanyl’s strength and overdose risk led many to seek out or continue MOUD treatment. “Harry,” a 22-year-old male shared how the uncertainty surrounding the putative presence of fentanyl in other drugs led him to MOUD:
I’m just worried because they’re putting that fentanyl in everything. Everything. So, it’s like you could pick up some weed and go to smoke some weed and die which that is part of the reason why I got on the naltrexone because you know, yeah, I want to stay sober, but I do smoke marijuana.
Although Harry no longer used opioids, he was wary of fentanyl in other drug supplies. Later, he shared that if he did relapse, naltrexone could be his saving grace, “Naltrexone. That’s about the smartest thing I’ve ever done. It’s probably going to save my life, if I do end up going back out and using,” (Harry).
This was a common sentiment echoed in many of the interviews – people wanted to use MOUD under the assumption that if they were to use opioids again, MOUD would offer a protection against overdose. Andrew went as far as to suggest that given the increasing number of overdoses, all people who use opioids should be on MOUD:
A guy’s going to get high. Unfortunately, they do, but people are scared because there’s fentanyl. You know what I mean? People are scared, but I think if people are wanting to get high the best thing for them is to get on this because people are dying out there like seriously. It’s bad, it’s bad. I wouldn’t sell dope. I won’t. You couldn’t pay me enough money to sell heroin right now or fentanyl. You couldn’t pay me enough. There’s not enough money in the world. Shit’s bad. I’m straight, I’m good but dudes want to get high, they still want to get high, but a lot of guys are scared, you know. I don’t know. If they can keep on methadone, they’ll be all right, or Suboxone (buprenorphine).
Other participants sought MOUD to discontinue drug use and cravings all together. For example, “Brian,” a 35-year-old male was committed to the RIDOC MOUD program due to his fear of relapsing given the prevalence of fentanyl:
I want to stay away from this fentanyl that’s killing people, you know, but you never know what you’re going to get. Like if I, I missed the methadone for a few days, based upon whatever’s going on out there, and I’ll have to get a bag to not be sick. And sometimes you don’t know what you’re getting. It’s like Russian Roulette, so I don’t want that.
Without access to MOUD in corrections, several people shared their belief that overdose deaths related to fentanyl would be much worse than they already were:
They’d be overdosing around here. More overdoses, and people would be dropping like flies because of the potency of the heroin in the street now with fentanyl. And they would bring it in the system, and people would be dropping. It would be more people in caskets than anything else (“Bruce,” 55-year-old male).
3.5.2. MOUD and increased preference for fentanyl
Unlike participants who sought out MOUD to avoid drug use, participants who continued using illicit opioids while in treatment with MOUD sometimes preferred fentanyl. A few participants explained how they felt that MOUD inhibited their ability to get high, thus only fentanyl’s strength and potency could “cut through” and provide their desired drug effects. “Lily,” a 31-year-old female shared her experience using fentanyl to get high while on methadone:
I know it sounds crazy, but I’m on methadone. It’s a blocker; and when I really do want to get high, I can’t just get high on heroin. So, I wanted the fentanyl. Isn’t that sad? It’s scary.
While some shared that methadone reduced the frequency of their use, when they did use drugs, they sought out fentanyl, believing, as Lily did, that it was the only way to get high. Likewise, one participant candidly shared his thought process in deciding to try fentanyl while prescribed buprenorphine:
Participant: I had taken a Suboxone [buprenorphine] in the morning. So this was about 3:00 in the afternoon and I knew if I was going to do any of it, I’d have to do a good portion to cut through. So that’s what I did. I did about … just a little bit to see what it would do and it fucking basically...
Interviewer: A little bit of the gram that you got?
Participant: Yeah, a very little bit. Probably about $10 worth. It put me on my ass and almost killed me. That was the other time I overdosed. My wife said she found me in the backyard basically laying in the fucking ground. So I called the kid up and I was like ‘hey man, something is wrong with that shit.’ This was later that night. He went, ‘yeah, I know, my roommate just died off the same stuff.’ So that was my introduction to fentanyl, but I didn’t know what it was (Robert, 41-year-old male).
This participant believed that while receiving MOUD, he would need to take a larger quantity to get high; however, his strategy to start first with a small amount still led to a nonfatal overdose due to the presence of fentanyl in his supply.
4. Discussion
We found that people enrolled in a carceral-based MOUD program had extensive knowledge of and experiences with fentanyl. They employed several identification and harm reduction techniques to detect fentanyl and reduce their risk of overdose. While a number of previous studies have explored fentanyl preferences, ours is the first to our knowledge to identify a complex and nuanced relationship between MOUD and fentanyl among people who are incarcerated. Fear of the potency and dangers associated with fentanyl led many people to seek out MOUD to reduce risk of overdose. A preference for fentanyl emerged among people who continued to use illicit substances while on MOUD. However, regardless of people’ preferences regarding fentanyl, participants universally advocated for MOUD to reduce the risk of overdose.
Our findings add to the existing literature on fentanyl perceptions and strategies to reduce risk (Stein et al., 2019, Latkin et al., 2019, Goldman et al., 2019, Rouhani et al., 2019, Victor et al., 2020). In line with the participants in Ciccarone et al. 2017’s study, which explored heroin user’s perception of fentanyl, our participants utilized comparisons with heroin when describing fentanyl and identified the same core differences (i.e., more intense rush, greater potency and shorter duration). Additionally, like the participants in Ciccarone’s 2017 study, despite prior identification techniques, many people found out about fentanyl in their supply through toxicology screenings, especially when under community supervision. The pattern, of people lacking complete knowledge of the content of their drug supply, has been explored previously in studies on expected versus actual exposure to fentanyl among people seeking treatment (Stone 2018, Stone 2020, Wakeman 2019, Martinez et al., 2020, and Kenney et al. 2018). Much like participants noted here, these previous findings all suggest while people believe they are aware of all substances in their drugs, they underestimate the likelihood of fentanyl exposure. Since the time of the interview, there has been an increase in prevalence of fentanyl test strips (FTS) in the community, which provide drug users a strategy to identify fentanyl at point-of-use (Laing et al., 2018). Recent studies suggest that people take protective measures, such as using a small sample (tester shot) or using more slowly, when awareness of fentanyl in their drug supply occurs though the use of FTS (Peiper et al., 2018, Rouhani et al., 2019). While more research is necessary to fully understand the relationship between the use of FTS and overdose outcomes, these initial studies suggest a correlation between knowledge of fentanyl though FTS and an increase in harm reduction strategies (Peiper et al., 2018, Rouhani et al., 2019, Sherman et al., 2019).
Due to the range in fentanyl preference among study participants, our findings contradict Carroll et al.,’s 2017 study wherein almost all participants disliked fentanyl. This may be in large part due to Carroll et al.’s study was conducted a few years earlier than the current study, when fentanyl was relatively new to the illicit drug market in Rhode Island. With time, some people who use and sell drugs may become more accustomed to fentanyl and come to prefer it. Findings from our study are consistent with McLean (2019) who found that “although the association of fentanyl with overdose did not deter most interviewees, many still described attempts to avoid fentanyl specifically, heroin more generally, or to stop using opioids overall.” Interestingly, a more recent qualitative study suggested age-based variations in preference for fentanyl. Specifically, younger participants appeared to display more perceptions of an immunity to fentanyl’s lethality, while older people seemed to express a stronger aversion to fentanyl, particularly due to the heightened risks associated with it (Gun et al., 2021). While our study did not analyze preference differences in relation to age, we did find that many participants in this study chose treatment with MOUD out of the belief that it would reduce their risk of overdose, even with continued use of illicit drugs. In fact, a number of participants who continued to use marijuana shared that they engaged in MOUD due to suspicion of fentanyl in their supply, however, it is important to note that there are no confirmed examples of fentanyl in marijuana. Numerous studies have demonstrated that continued MOUD use even with ongoing drug use is correlated with reduced overdose mortality (National Academies of Sciences, Engineering & Medicine, 2019; Schwartz et al., 2013; Schuckit et al., 2016). Notably, people on methadone or prescribed buprenorphine, may require higher doses of MOUD to appropriately treat people with OUD who have been using fentanyl (Stone 2018, Stone 2020, Herring et al., 2021).
While many of our findings have been corroborated by previous research, this is the first study to document attitudes and perceptions of fentanyl among persons enrolled in treatment with MOUD, and to explore the relationship between treatment with MOUD and fentanyl preferences among people who were incarcerated. Many of the participants were very willing to share their personal, and often graphic, experiences with fentanyl. Often without prompting, and early in the interview before the section focused on fentanyl (Table 1), participants brought up fentanyl; this suggests that fentanyl is conspicuous in the consciousness of people with opioid use disorder who are receiving MOUD behind bars.
The opioid crisis is rapidly evolving. It is clear, however, that illicitly manufactured fentanyl remains highly prevalent in illicit drug supplies. The increasing presence of this powerful synthetic opioid, and a persistent fear of fentanyl among many people who use illicit drugs, underscores the need for alternative methods to support people as they navigate their drug use and withdrawal symptoms. As brought forth from the participants themselves, broad access to MOUD may both aid people seeking recovery due to the increased overdose risk of drug use and reduce overdose morbidity for people who continue to use drugs. Thus, increasing access to MOUD in both correctional settings and the communities to which people are released, may serve as an effective strategy to mitigate the crisis (National Academies of Sciences, Engineering, and Medicine, 2019). McLeod’s 2021 study in British Columbia demonstrated how connecting with community health workers within the first 30 days of release from prison, was correlated with a significant reduction in fatal overdoses (McLeod et al., 2021). The use of community health workers to connect people who are leaving prison with MOUD services in the community might be essential to minimize fatal overdoses during the reentry period in our current era of fentanyl. Additionally, given the vast lack of awareness of fentanyl in other illicit drugs (especially counterfeit medications and stimulants like cocaine) harm reduction measures such as provision of fentanyl test strips and naloxone distribution, paired with educational efforts, may greatly reduce fentanyl involved overdoses (Nolan 2019, Park 2018).
The most notable limitation of this study is that the population being interviewed is not generalizable to everyone with opioid use disorder, as all participants were enrolled in a MOUD treatment program and were being asked to talk about their experience with MOUD.
5. Conclusion
Our semi-structured qualitative interviews with people who were incarcerated at the RIDOC explored the impressions, preferences for and experiences with fentanyl. Our findings emphasized an increased prevalence of and ongoing fear surrounding fentanyl in the community. Most of the participants were familiar with fentanyl and utilized harm reduction techniques when using drugs. All the participants described their perception of MOUD as a means of reducing their risk of overdose. This is the first paper, to our knowledge, to identify the increasingly complex relationship between MOUD, ongoing drug use, and fentanyl preference, especially in a setting of people at elevated risk of overdose. Participants expressed an appreciation and need for MOUD, ranging from supporting abstinence from illicit drugs for some to reducing overdose risk with ongoing drug use for others.