Abstract
Opioid overdose deaths and opioid-related harms have reached unprecedented levels, particularly as compounds such as xylazine and fentanyl have infiltrated the drug supply. Harm reduction strategies are especially relevant in this climate, as they aim to reduce drug-related harms independently of whether an individual chooses to enter treatment or abstain from opioid use. Assessment of harm reduction strategies should consider targets beyond substance use. The purpose of this narrative review is to summarize existing harm reduction strategies in the United States and elsewhere and to describe how outcomes of these strategies could be assessed. Strategies designed to reduce opioid-related harms include syringe exchange programs, overdose education and naloxone distribution, supervised consumption sites, injectable opioid agonist treatment, safer supply programs, drug checking, and decriminalization. Outcomes besides abstinence that could be considered include reductions in substance use patterns that are associated with a high likelihood of negative consequences (e.g., solitary use and polydrug use), reductions in severity of opioid use disorder or early remission of opioid use disorder, improved quality of life and psychological health, improvements in community functioning including linkage and adherence to treatment, and reductions in the incidence of infectious disease. As opioid overdose deaths and related harms continue to rise, harm reduction strategies have become critically important. Harm reduction strategies for opioid use disorder should be considered in the context of outcomes that extend beyond measuring drug use, to capture benefits such as reduced mortality and greater well-being and quality of life.
The opioid crisis is one of the most significant public health challenges of our time. Since the turn of the century, more than 1 million individuals in the United States have died of a drug overdose, the majority of which involved an opioid. Worsening trends in opioid overdose deaths have been driven by increased accessibility of opioids in the illicit market, an increased number of individuals using opioids, and a progression of risk factors associated with the opioid drug supply. The early 2000s were marked by wide accessibility to and use of licit opioids (e.g., prescription opioids) and illicit opioids, with prescription opioids accounting for the majority of opioid overdose deaths during this time. Decreased accessibility of prescription opioids starting around 2010 led many individuals to a growing heroin market, which was relatively less expensive but conferred greater risk of overdose death compared with prescription opioids because of the variable potency of illicit heroin. The introduction of illicitly manufactured fentanyl into the heroin supply began to increase substantially around 2013, and fentanyl has now largely replaced heroin in many regions across the United States. Illicitly manufactured fentanyl and many fentanyl analogues are far more potent than heroin and carry increased risk of respiratory depression relative to other opioids, further compounding the risk of overdose deaths among persons who use these drugs. Finally, recent trends in opioid-stimulant co-use, along with the introduction of additives such as xylazine and nitazenes into the opioid supply, have further increased overdose deaths in the United States, as well as having other health consequences, such as skin ulcers.
Treatment for opioid use disorder with the goal of abstinence from opioids and other substances is the best approach to eliminate the risk of overdose death. In particular, medication treatments, including methadone, buprenorphine, and naltrexone, are considered the gold standard for management of opioid use disorder. Agonist (i.e., methadone) and partial agonist (i.e., buprenorphine) treatments reduce withdrawal symptoms and craving in persons with opioid use disorder, improving quality of life. In contrast, antagonist treatment (i.e., naltrexone) blocks the effects of opioids. However, only about 20% of individuals with opioid use disorder initiate medication treatment for opioid use. Moreover, many persons with opioid use disorder do not have treatment goals that include complete abstinence. In light of the unprecedented morbidity and mortality currently associated with opioid use, there is a pressing need to employ public health initiatives that reduce harms and save lives for persons exposed to opioids. The aim of this review is to characterize and describe strategies for harm reduction and identify potential outcome measures for public health research and practice in the United States.
Methods
We reviewed the Scale for the Assessment of Narrative Review Articles guidelines in preparing this review. The search strategy involved searching databases (e.g., Web of Science, PubMed, and PsycInfo) and academic search engines (e.g., Google Scholar) with keywords related to opioid use disorder (e.g., “opioid,” “opioid use disorder,” “OUD,” “heroin,” “fentanyl,” and “xylazine”) and keywords related to harm reduction (e.g., “harm reduction,” “syringe exchange,” “needle exchange,” “overdose prevention,” “supervised consumption,” “naloxone,” “Narcan,” “injectable opioid agonist treatment,” “safer supply,” “legalization,” and “decriminalization”). We also reviewed our personal collections, articles cited in papers returned in the search, and previous reviews on harm reduction to identify relevant literature (i.e., articles describing implementation of a harm reduction strategy in the context of opioid use disorder).
Strategies for Harm Reduction
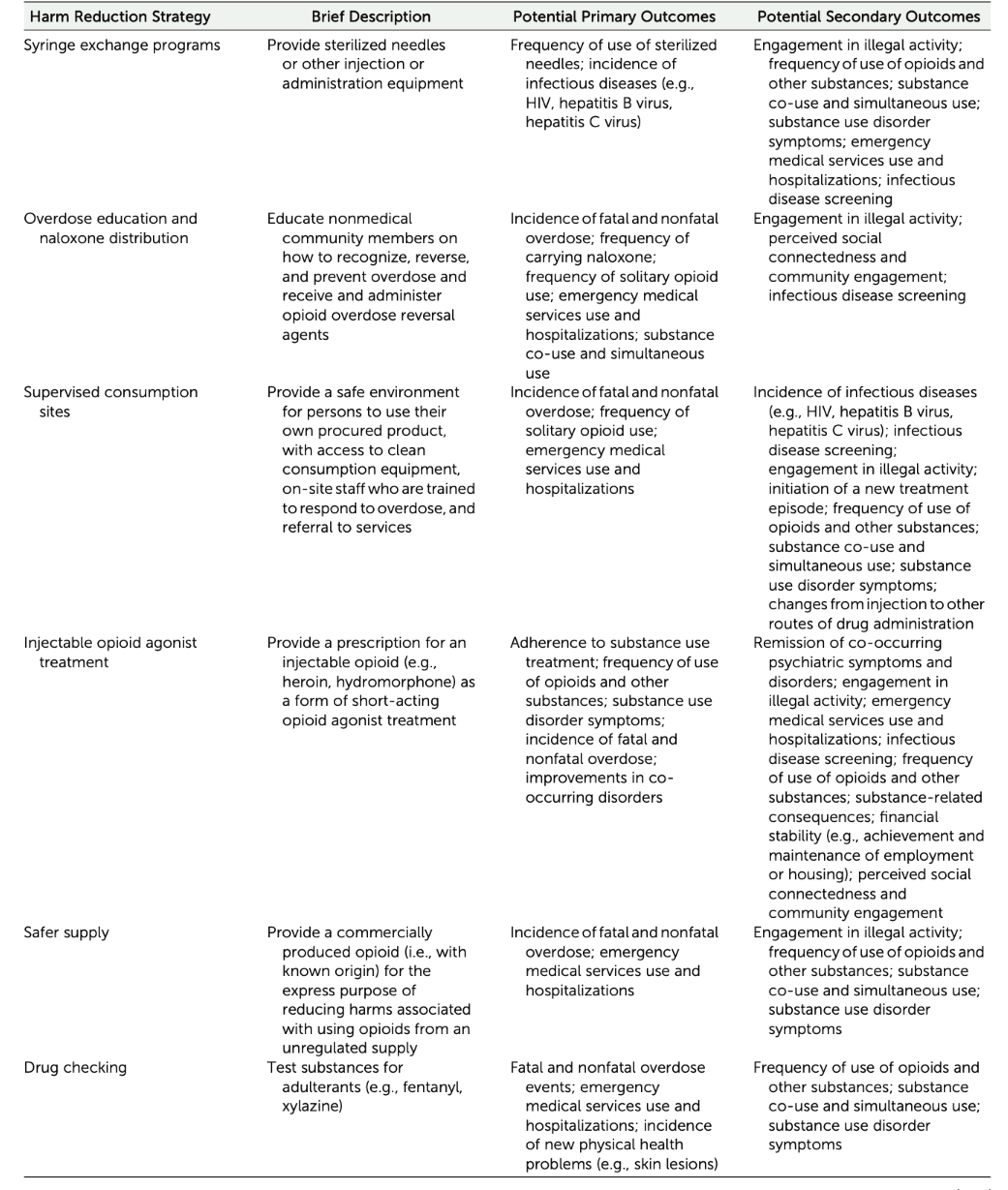
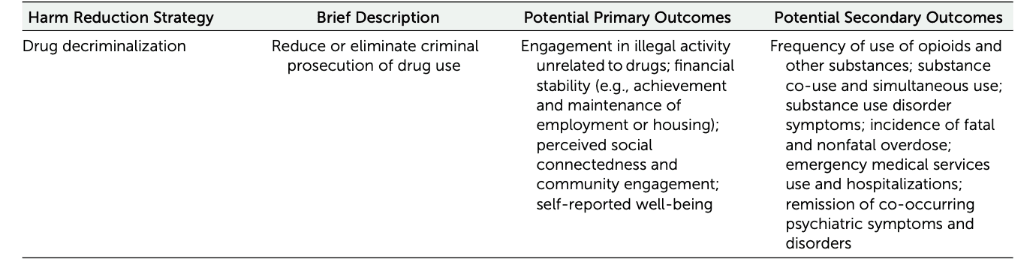
Harm reduction is an approach or a set of strategies focused on reducing the negative consequences of drug exposure. Harm reduction approaches are designed to meet individuals where they are in their drug use experience, emphasizing respect for the individual and helping them to remain safe while using substances. Harm reduction strategies may help individuals move from active use to a state of abstinence; however, their primary focus is on improving an individual’s safety independently of changes in use patterns or abstinence initiation. Harm reduction can take many forms, and there are some robust and successful harm reduction strategies being implemented in the United States. Many additional strategies with proven success have been implemented outside the United States and are worth considering in the context of our ongoing crisis. Below we outline existing harm reduction approaches in the United States and elsewhere where outcomes have direct relevance to the opioid epidemic. Additional harm reduction strategies that intersect with other efforts to keep individuals safe—such as protection of sex workers, decreasing the impact of poverty on health, and increasing access to housing—are not discussed here, for brevity, but they provide valuable support to persons who use drugs. An overview of the harm reduction strategies discussed below is provided in Table 1.
Syringe Exchange Programs
One of the original forms of harm reduction established in the United States—syringe exchange programs—was developed during the HIV/AIDS epidemic in the late 1980s to help mitigate the risk of disease infection and transmission. Syringe exchange programs provide persons who use drugs an opportunity to receive sterilized needles and injection equipment. These programs can be stationary or mobile and can educate individuals on safe injection practices to limit disease transmission or infections. Although critics have pointed out that the success of these programs is largely contingent on the provided syringes being returned to syringe exchange programs, one review of return rates for syringe exchange programs found an average return rate of 90%. Furthermore, studies have repeatedly demonstrated that syringe exchange programs successfully reduce the risk of infection and are cost-effective and safe, without increasing the risk of unintended consequences, such as crime or increased drug use. Moreover, evidence suggests that persons who use syringe exchanges are five times more likely to enter treatment than persons who do not, suggesting that syringe exchange programs may be serving as the first step along the continuum of care.
Overdose Education and Naloxone Distribution
A second long-standing harm reduction strategy in the United States is overdose education and naloxone distribution. These programs were pioneered in the late 1990s in response to increasing rates of overdose related to the launch of several commercial opioids, such as oxycodone, and the increasing purity and availability of heroin. Enterprising public health workers procured ampoules of the injectable form of naloxone (a potent overdose antidote) intended for administration in hospital-based settings to train nonmedical community-based bystanders to identify and reverse overdoses with naloxone in their community.
These programs have faced and surmounted numerous regulatory barriers over the past several decades, including challenges to the legal provision of naloxone (previously a prescription medication) to nonmedical persons for third-party administration, the need for Good Samaritan laws to absolve bystanders (many of whom were also drug exposed) from legal consequences for contacting medical support, and the need for standing orders to make naloxone products widely available without the need to visit a provider for a prescription. Many of these regulatory barriers emerged in the context of concerns about the capacity of bystanders to administer naloxone and fear that the availability of such medications could encourage overconsumption or decrease the likelihood of contacting emergency services.
Over time, aspirators that could be affixed to the injection ampoules were developed to enable intranasal administration (followed by formal development and approval of an intranasal product), and the training and education curriculum was standardized. This movement has been associated with profound reductions in opioid overdose mortality and has been particularly impactful since the introduction of illicitly manufactured fentanyl and fentanyl analogues into the opioid supply. Overdose education and naloxone distribution programs have also been integrated into syringe exchange programs, community sites, and health care systems, such as the Veterans Health Administration. Although outcomes are challenging to track, data routinely suggest that these programs dispense thousands of doses of naloxone and are responsible for thousands of lives saved. Although it is unclear how the recent approval of an over-the-counter formulation of naloxone will affect these programs, overdose education and naloxone distribution programs are crucial community-based harm reduction programs.
Supervised Consumption Sites
Supervised consumption sites have robust support outside the United States and more variable support within the United States. Supervised consumption sites (previously known as supervised injection sites) can be viewed as an adaptation of syringe exchange programs. Beginning in Switzerland in the mid-1980s to mitigate risk of HIV/AIDS transmission and infection, supervised consumption sites provided persons who use drugs a safe space in which to self-administer their drugs (generally via injection). The sites served as a safe and monitored environment that also provided individuals access to clean injection equipment. This approach was adopted by several other European countries, leading to the development of formal recommendations for implementing these programs. Although supervised consumption sites were established to provide a safe place for injecting substances, transitions in use patterns led them to expand support to include other forms of administration (leading to the change in terminology from supervised injection to supervised consumption). There are more than 200 sanctioned sites throughout the world; there is evidence of consumption sites in the United States, but they are not yet formally sanctioned by the federal government and thus confer legal risk to the operators. Furthermore, logistical considerations have been raised in the literature regarding whether to impose restrictions on particular groups (e.g., pregnant persons and adolescents) or on use practices (e.g., number of use events per visit and bodily injection sites); consensus on these points has not yet been achieved. Much like syringe exchange programs, supervised consumption sites are associated with a variety of health benefits, including reductions in disease transmission and drug-related mortality and morbidity, with no evidence of increases in drug use or social problems such as crime. Many sites have also incorporated overdose education and naloxone distribution programs, and there is a growing discourse suggesting that supervised consumption sites become a formally approved and endorsed strategy in the United States.
Injectable Opioid Agonist Treatment
Supervised consumption is often conflated with injectable opioid agonist treatment, a practice in which patients receive a prescription to self-administer injectable diacetylmorphine (heroin) or hydromorphone as a form of treatment. Although supervised consumption is a valuable component of injectable opioid agonist treatment, these are two distinct strategies. Injectable opioid agonist treatment has been approved in some countries for several decades and was approved most recently in Canada, following the pivotal North American Opiate Medication Initiative (NAOMI) trial. The legal requirements for prescribing injectable opioid agonist treatment vary, but often require some evidence that an individual is not responsive to other long-acting or noninjected forms of agonist treatment (e.g., methadone or buprenorphine) before injectable opioid agonist treatment can be initiated. It is somewhat debatable whether injectable opioid agonist treatment is a harm reduction technique. On the one hand, the fact that injectable opioid agonist treatment incurs risks associated with injection practices suggests that its reduction of harm is incremental. On the other hand, injectable opioid agonist treatment can be viewed as a distinct form of agonist treatment for persons who respond preferentially to short-acting opioids. Studies of persons who initiated injectable opioid agonist treatment after treatment with long-acting opioids find they have better treatment outcomes relative to persons who did poorly with long-acting opioid medications but were not transitioned to injectable opioid agonist treatment; yet these studies also highlight the increased risk that is inherent in repeated injections, further emphasizing that injectable opioid agonist treatment may be viewed as an important part of the harm reduction continuum.
Safer Supply Programs
The establishment of safer supply programs was a strategy made possible in Canada after the approval of hydromorphone as an injectable opioid agonist treatment based on the successful NAOMI trial. Hydromorphone was of particular interest as an injectable opioid agonist treatment because it has been approved and used routinely for pain management for decades, and thus, existing regulatory structures and pharmacy pathways made its dispensing and prescribing as an injectable opioid agonist treatment easier than for diacetylmorphine. In the context of the illicit fentanyl crisis, there has been growing consumer interest in having hydromorphone (and other opioid products) be prescribed directly to patients to address what is being increasingly referred to as a “drug poisoning problem.” Advocates for safer supply programs emphasize that increases in overdose deaths are not confined to persons using high quantities of potent opioids like fentanyl but are occurring increasingly among persons who have accidental or unintended exposure to illicit fentanyl, fentanyl analogues, xylazine, or other adulterants. The concept of safer supply is premised on the notion that providing persons who use drugs a product of known origin and manufacturing (e.g., a regulated supply) eliminates the risk of exposure to illicitly manufactured fentanyl. This aspect of such programs strongly differentiates safer supply from injectable opioid agonist treatment or other treatments because its endpoint is a reduction in harm related to improving the safety of the drug supply rather than an endpoint based on a therapeutic goal. Because safer supply programs have been implemented largely by community (vs. research) programs (much as naloxone for bystander administration once was), the data supporting or refuting this strategy are sparse and challenging to collect. Emerging evidence suggests that safer supply programs may improve functioning and reduce risky injection behaviors and overdose risk, ultimately increasing safety as intended, although concerns have been raised regarding dispensing of safer supplies that occurs outside the umbrella of opioid treatment providers. Safer supply programs have been formally embraced as a harm reduction strategy by Health Canada but have not yet been adopted in the United States.
Drug Checking
Drug checking is a harm reduction strategy used to combat unintentional exposure to illicitly manufactured fentanyl and other adulterants by gaining knowledge of drug contamination from unregulated supplies. Drug checking may include physical stations where trained experts test small quantities of substances for persons using drugs, or it can involve the dissemination of test strips intended to be used by individuals who want to check their drug supply at home before ingestion. Physical drug-testing programs can be located in mobile vans that travel to events (such as music festivals) or are parked in highly trafficked locations to conduct testing for individuals, and these programs are often embedded in other harm reduction programs, such as supervised consumption or overdose education and naloxone distribution programs. Brick-and-mortar programs have also been established for individuals to bring their products in for testing; these programs may have a greater range of tests available but often require more technical knowledge to run the test assays compared with mobile van–based or home-based analyses. Drug-testing programs can increase safety for persons who use drugs and also provide valuable surveillance regarding emerging trends in adulteration or drug concentration that can be used to inform broader prevention campaigns. Drug checking has received some criticisms, most notably the continual cost, as well as potential privacy concerns for people who use the services and the limited ability of drug-checking services to accurately test for all substances that could induce a reaction. Nonetheless, the available evidence supports drug checking as a harm reduction strategy; persons who use drug-checking programs routinely learn that their drugs contain adulterants that are unexpected and unintended (27), and 1 in 5 people report changing their use as a result.
Drug Decriminalization
Drug decriminalization is a harm reduction strategy that reduces or eliminates legal consequences of substance use, with the intention of reducing burden on the criminal justice system. Individual-level consequences associated with justice system involvement, including challenges related to individuals’ financial, social, employment, and housing situation, as well as the racial inequities in drug law enforcement, are also mitigated. In 2001, Portugal became the first country to decriminalize possession of all illicit drugs, when it designated drug possession as an administrative violation; simultaneously, access to treatment and harm reduction services and education about drugs in schools were increased. Since that time, numerous other regions have passed broad drug decriminalization policies. In the United States, for instance, voters in Oregon passed Measure 110, which decriminalized possession of small amounts of drugs and increased treatment and harm reduction services. Although decriminalization in Portugal has been cited as an effective model for reducing drug-related harms without increasing use, early findings after Measure 110 have yielded mixed results. Ultimately, drug decriminalization has the potential to minimize legal harms associated with drug use and to simultaneously emphasize access to harm reduction services to mitigate nonlegal risks.
Outcomes of Interest in Harm Reduction Studies
Evaluating harm reduction strategies requires a conceptual framework in which abstinence or a reduction in substance use is not the primary desired outcome. Harm reduction strategies should instead be evaluated based on their effectiveness in reducing morbidity and mortality, improving quality of life, and minimizing individual and community harms. Below, we review specific outcomes that warrant consideration in studies of harm reduction strategies and underscore the relevance of these outcomes for policy makers evaluating the effectiveness of new harm reduction initiatives.
Reductions in Opioid and Other Substance Use
Evaluation of harm reduction policies and initiatives has sometimes included opioid use as an outcome. However, when doing so, it is important to consider that many individuals who access harm reduction services or initiatives are not seeking treatment and that abstinence is unlikely to emerge from harm reduction strategies alone. Alternative drug-related outcomes include reductions in opioid use disorder symptoms or reductions in opioid-related consequences. Furthermore, any meaningful change in opioid use following implementation of a harm reduction strategy should be viewed in the context of overall functioning and well-being. For example, if an individual garners some benefit from harm reduction services (e.g., reduced criminal justice system contact or improved financial functioning) and does not engage in more use than individuals who did not access harm reduction services, then this may be seen as a positive outcome.
Reductions in co-use of substances (i.e., using different substances in the same time period) or simultaneous substance use (i.e., use of different substances at the same time) should also be considered when evaluating harm reduction strategies. High levels of substance co-use have been found among individuals with substance use disorder, and as many as 77.2% of individuals with opioid use disorder meet criteria for at least one other substance use disorder. The use of multiple substances substantially increases risks of substance-related harms; for instance, use of stimulants (e.g., methamphetamine or cocaine) in combination with opioids can increase risk of overdose and result in difficulties with treatment, and the use of opioids with sedative or anxiolytic medications can increase risk of respiratory depression. Thus, ongoing substance use that is accompanied by reduced substance co-use and related sequelae may be regarded as a positive outcome.
Engagement in Safer Opioid Use Practices and Reductions in Opioid-Related Harms
Recurrent opioid use in physically hazardous situations is a symptom of opioid use disorder that is commonly targeted in harm reduction strategies, and increases in safer opioid use behaviors should be considered as outcomes in the evaluation of harm reduction programs. Examples of safe opioid use behaviors targeted by harm reduction policies include carrying naloxone, using sterilized needles, properly disposing of syringes, and using drug administration routes other than injection. Less commonly measured outcomes that are nonetheless relevant in harm reduction include refraining from solitary use and refraining from using opioids when driving or operating machinery.
Relatedly, fatal and nonfatal overdose events should be considered as primary endpoints in evaluations of harm reduction. For several types of harm reduction initiatives, including the establishment of safe consumption sites, safer supply programs, and naloxone distribution efforts, overdose rates have been a primary outcome of interest. For instance, a systematic review examining effects of safe consumption sites found that overdose mortality was an outcome in five of 22 studies. Furthermore, overdose was included as a primary outcome in one of the first evaluations of decriminalization policies in Oregon and Washington; that study found that fatal drug overdose rates did not significantly decrease or increase in the year following decriminalization relative to rates in control states.
Nonetheless, there are some limitations to using overdose as an outcome. In the case of using fatal overdose as an outcome, death certificates are often imprecise, and it is often difficult to determine whether an overdose was intentional or unintentional. Overdose data are often reported for broad geographic levels (e.g., the county or state level), making it difficult to determine the effects of smaller-scale interventions (e.g., the impact of a single site or a few sites) on fatal overdose. In the case of using nonfatal overdose as an outcome, the population-level prevalence of nonfatal overdose is difficult to determine, and subjective reports of nonfatal overdose are subject to stigma associated with reporting overdose. As an alternative or complementary outcome, use of emergency medical services could potentially be considered a proxy of nonfatal overdose or an overdose-related accident. Harm reduction strategies that reduce fatal and nonfatal overdose and reduce the use of emergency medical services have the potential to play a pivotal role in reducing substance-related harms.
Improvements in Community Functioning
Improvements in community functioning are also vital outcomes for harm reduction initiatives. First, financial stability, which can be qualified as residing in stable housing for a greater number of days, attaining independent housing, attaining and maintaining employment, and reducing money spent on substances, is essential to community functioning. Financial stability has historically been used as an outcome in studies evaluating Housing First interventions and other harm reduction interventions providing financial supplements. However, financial stability can be considered across a broader number of harm reduction strategies, including drug decriminalization (in which the lack of a criminal record may be expected to increase financial stability, employment, and housing opportunities) and in terms of long-term outcomes such as safe consumption and linkage to treatment.
Minimizing interactions with the criminal justice system is another community-based outcome relevant to harm reduction strategies. When individuals are released from incarceration, they face an elevated risk for overdose because of reductions in opioid tolerance. Although attention has been given to this issue, and an increasing number of facilities offer medications for opioid use disorder on release from incarceration, a sizable number do not. Additionally, a criminal record can substantially complicate other treatment goals, such as attaining housing or employment. Some harm reduction policies (e.g., decriminalization) may reduce arrests directly, and therefore, examination of engagement in other illegal behaviors (i.e., those not related to drug use) can be considered. For example, in one of the first evaluations of decriminalization in Oregon and Washington, results suggested that although drug-related arrests decreased slightly, overall arrests, nondrug arrests, and arrests for violent crimes did not significantly change. These findings should be viewed in the context of local and national averages and the fact that Portland, Oregon, experienced a particularly large increase in overdose deaths and homicides leading up to and following their drug decriminalization efforts. Illegal activity around safe consumption sites has also been of particular interest, with a recent review finding that five of seven studies evidenced beneficial effects of safe consumption sites on crime and public nuisance, and two studies found null results. Collectively, these results highlight the significance of examining involvement in the criminal justice system as an outcome.
Finally, perceived social connectedness and engagement in the community are important aspects of community functioning that should be evaluated in harm reduction studies. One of the DSM-5-TR criteria for opioid use disorder is that important occupational, social, or recreational activities are given up because of substance use. Isolation is also common among persons who use drugs, and it can negatively impact quality of life. Thus, if an individual makes no changes in their substance use patterns and does not initiate treatment but is able to make social connections that are meaningful or engage in recreational activities outside of substance use, this may be considered a positive outcome.
Improvements in Psychological and Physical Health
A recent systematic review estimated that as many as one-third of individuals with opioid use disorder have co-occurring major depressive disorder, generalized anxiety, or antisocial personality disorder, approximately one-fifth meet criteria for attention deficit hyperactivity disorder or posttraumatic stress disorder, and approximately 8.7% meet criteria for bipolar disorder. Co-occurring symptoms may be inconsistently associated with opioid use disorder treatment outcomes, or they may be attributed to substance use treatment only among some individuals. However, improvements in or remission from co-occurring disorders can substantially improve the quality of life for individuals with opioid use disorder, even when collateral improvements in drug use outcomes are not observed.
Additionally, many individuals with opioid use disorder who do not meet full diagnostic criteria for a co-occurring disorder may still experience mental health symptoms that negatively impact their quality of life (e.g., loss of pleasure that occurs outside the context of a major depressive episode). Reductions in symptom presentation and severity, as well as progression to a co-occurring disorder, can all be considered as outcomes. Positive affect and well-being are aspects of psychological health that could be considered as outcomes, particularly for interventions designed to improve quality of life (e.g., housing or financial assistance) and for initiatives that promote access to methods that enable safe use.
Improvements in physical health are also valuable outcomes in the context of harm reduction interventions. Substantial efforts have been made to reduce the spread of infectious diseases that can be transmitted through the sharing of needles, such as HIV, hepatitis B virus, and hepatitis C virus. Harm reduction initiatives could examine effects on engagement in infectious disease–screening opportunities, linkage to treatment for health conditions, and decreases in community transmission rates. Among persons who have already contracted an infectious disease, adherence to treatment, health care utilization, reductions in viral load, and decreases in hospitalizations and mortality have been examined as outcomes. With the increase in physical health consequences (e.g., skin lesions) related to xylazine use, occurrence of new physical health symptoms and adherence to treatment will be particularly important to track.
Intensive longitudinal designs could be leveraged to conceptualize, measure, and quantify changes in mental and physical health symptoms, using indices of intraindividual variability (e.g., symptom stability and decreased variability), ideally using measures tailored to the co-occurring disorder or symptoms in question to assess symptom status and resolution. For example, for individuals with a mental health condition characterized by severe mood lability (e.g., borderline personality disorder), outcomes may include reductions in variability and severity of symptoms. However, for individuals with other symptoms and conditions (e.g., those with anhedonia), variability in emotion—particularly positive emotion—may be seen as an improvement (e.g., if individuals are becoming increasingly reactive to naturally reinforcing stimuli).
Linkage and Adherence to Evidence-Based Opioid Use Disorder Treatment
Many individuals who utilize harm reduction services (e.g., safe consumption sites) may be seeking treatment or may become treatment seekers; thus, initiating a treatment episode after engaging with a harm reduction service may be considered a successful outcome. Safe consumption sites will sometimes offer on-site information about how to initiate treatment, or they may be directly affiliated with a treatment program, which highlights the importance of collecting data about the frequency with which individuals using these services decide to pursue treatment. However, it will be important to interpret any findings in the context of the low base rate (<5%) of treatment seeking among individuals who need treatment for a substance use disorder in the United States.
Harm reduction studies can also evaluate whether adherence to treatment among persons already in treatment is influenced by harm reduction interventions and policies. In these analyses, finding that harm reduction programs have not decreased adherence to substance use treatment can sometimes be an outcome of interest. For example, in one study with unhoused patients who were receiving methadone treatment, access to a Housing First model, in which individuals received housing and adjunctive community treatment, did not reduce the proportion of days during the observation period in which a medication was dispensed. In this case, a null result may be perceived as a beneficial outcome, if benefits unrelated to substances can be conferred without unduly affecting treatment outcomes for the substance use disorder. Assessing harm reduction outcomes can also be useful in the context of administering medications for opioid use disorder (e.g., methadone or buprenorphine), because improved mental health and social functioning might be an indication that these treatments are working in the absence of complete abstinence from opioids or other substances.
Conclusions
The harm reduction strategies reviewed here prioritize reducing morbidity and mortality associated with opioid use disorder as well as improving social functioning and quality of life. Efforts to distribute naloxone with proper education and to provide a safer opioid supply might be the most immediate actions to reduce overdose deaths. Endpoints for public health studies and clinical trials should include fatal and nonfatal overdoses along with a host of physical and mental health outcomes to understand fully how distinct harm reduction initiatives might benefit persons who use opioids. Linking individuals to long-term opioid use disorder treatment is another important factor in harm reduction initiatives, even if the primary goal does not include treatment. Initiating and retaining persons with opioid use disorder in long-term, meaningful treatment remains a priority for the medical community. Harm reduction strategies are important options that can help keep people alive long enough to enter treatment on their own terms and also improve health, social relationships, and community conditions.