Abstract
Background The COVID-19 pandemic and measures have placed various burdens on societies and individuals. Emerging evidence suggests that people in drug addiction recovery were negatively affected. This study investigates whether risk and protective factors associated with return to problematic substance use differed between the periods before and during the pandemic for those in recovery.
Methods A convenience sample of persons in drug addiction recovery for at least three months completed an assessment at baseline before the pandemic (T0, N = 367) and at two consecutive follow-ups 12 months apart (T1, N = 311; T2, N = 246). The final follow-up took place during the pandemic (2020−2021). We analyzed rates and predictors of problematic substance use in both periods, and whether relations between predictors and problematic use differed between the periods.
Results Rates of problematic use did not differ significantly before and during the pandemic for those who were followed-up. However, the relationship between problematic use and commitment to sobriety differed between both periods (OR = 3.24, P = 0.010), as higher commitment was only associated with lower odds of problematic use during (OR = 0.27, P < 0.001), but not before, the pandemic (OR = 0.93, P = 0.762). In both periods, persons who were engaged in psychosocial support had lower odds of problematic use.
Conclusions The COVID-19 pandemic was not followed by significant return to problematic substance use in a cohort of people who were already in drug addiction recovery for some time before the pandemic. However, with restricted access to environmental resources, they may have been more dependent on internal motivations. Targeting personal recovery resources with interventions could therefore reduce the chances of return to problematic substance use during a pandemic.
Highlights
The COVID-19 pandemic was not followed by an increase in problematic substance use in a drug addiction recovery cohort.
Different variables predicted problematic substance use in recovery in the period before and during the COVID-19 pandemic.
During the pandemic participants seem to have been more dependent on commitment from themselves to prevent problematic use.
Building up internal recovery resources may reduce vulnerability for return to problematic substance use during a pandemic.
1. Introduction
Since the first cases of COVID-19, the pandemic placed a burden on societies and individuals. In response to the quickly spreading virus, governments launched measures such as quarantine, lockdowns, and social distancing. Although these measures slowed the spreading of the coronavirus, concerns existed about how they have affected public health, including access to addiction recovery services, as well as individuals' anxieties, fears, and social contacts (Marsden et al., 2020).
The pandemic is likely to have impacted the markets and use of illicit drugs through effects of the virus itself, restrictions on movement and gathering, as well as social, economic and health consequences (Dietze & Peacock, 2020; Price et al., 2022). Access to (face-to-face) treatment, (peer) support, work, and other meaningful activities was limited (Blanco et al., 2020; Nadkarni et al., 2020). So far, one of the most notable changes in drug treatment has been the expansion of online digital services in clinical and community practices to compensate for the lack of face-to-face support (Bergman & Kelly, 2021; Blanco et al., 2020). Some studies suggest that people in treatment settings were affected in both positive and negative ways (Liese & Monley, 2021; Smith et al., 2021). A longitudinal study among US veterans conducted before and during the pandemic (2019–2020), found that the prevalence of alcohol use disorders remained stable, but that those with more COVID-related stressors were at higher risk of developing alcohol use disorder (Na et al., 2021). In Spain, patients attending outpatient addiction service in Barcelona were more likely to screen positive for alcohol and drugs during the lockdown compared to a prior period (Barrio et al., 2021). However, limited data are available on populations in addiction recovery outside treatment or support settings.
A cross-sectional study in the United States found that the COVID-19 pandemic “did not affect recovery at all” (as reported by participants) for the majority (89 %) of participants in recovery from alcohol use disorder, and that mild relapses (i.e. violation of abstinence, but resolved at the time of data collection) were infrequent (Gilbert et al., 2021). Another study found that during a lockdown period in Israel, about half of all adult participants in recovery from a substance use disorder reported cravings, prompted by boredom, loneliness, lack of support, and financial stress (Bonny-Noach & Gold, 2021). A review further suggests that discontinuation of opioid substitution therapy delivery because of the pandemic may have caused involuntary withdrawal, which can lead to relapse to illicit opiate use (Mallet et al., 2021). Lastly, a study identified pandemic-related recovery barriers, including cancelled support meetings, changes in job format (i.e., being fired or furloughed), and lack of social support, which people coped with through self-care, leisure activities (or hobbies), taking caution against exposure, and strengthening personal relationships (Shircliff et al., 2022). Yet, the impact of the pandemic on people in addiction recovery is only beginning to emerge and early publications about expected impacts from the pandemic suggest a high risk of relapse, impacting recovery stability (Da et al., 2020; Dunlop et al., 2020; Marani et al., 2021; Melamed et al., 2020; Volkow, 2020).
Addiction recovery research from the last two decades agrees that recovery is a personal process that takes place in various ways, depending on circumstances, and may include improvements in multiple life domains, including housing, relationships, employment, and well-being (Kaskutas et al., 2014; Neale et al., 2014). Reviews estimate that more than half of all individuals with a lifetime alcohol or drug dependence will achieve stable recovery (Kelly, 2017; Sheedy & Whitter, 2009; White, 2012). Still, drug addiction is often described as a chronic relapsing disorder (McLellan et al., 2000). Relapse is therefore considered a serious risk for persons in recovery, particularly in the early stages of recovery (Laudet & White, 2010; Martinelli, Nagelhout, et al., 2020). A considerable amount of research has focused on short-term relapse among individuals after treatment. However, we know much less about relapse among individuals in long-term recovery outside treatment settings, and relapse is often poorly defined in research (Moe et al., 2022; Sliedrecht et al., 2022). While many studies consider (any) violation of abstinence a relapse, it remains unclear to what extent such an event impacts broader recovery processes (Moos & Moos, 2006). This knowledge gap applies particularly to research on people who use(d) illicit drugs, as the literature tells us much more about alcohol relapse (Connors et al., 1996; Miller et al., 2001; Vaillant, 1988; Vuchinich & Tucker, 1996; Witkiewitz & Marlatt, 2007).
Factors known to increase the risks of relapse include stressful and negative life events (e.g. death of a spouse) (Marlatt & Gordon, 1985), negative mood states such as (psychological di)stress, social isolation, perceived stigma (Connors et al., 1996; Friedmann et al., 1998; Link et al., 2001; Marlatt & Gordon, 1985; Miller, 1996; Sinha, 2007), low self-efficacy (DiClemente et al., 1985), and low motivational states (Miller, 1985). In contrast, social support, social group membership, treatment engagement, and recovery capital (Cloud & Granfield, 2008) are considered protective against relapse (Havassy et al., 1991; Vaillant, 1988). In the United States and the UK, a rise in psychological distress was observed in the general population in 2020, compared to 2018–19 (McGinty et al., 2020; Pierce et al., 2020). Furthermore, studies conducted during the pandemic found that an increase in substance use was associated with more psychological distress (Lommer et al., 2022; Taylor et al., 2021) and that persons with pre-existing mental health problems reported higher psychological stress compared to control groups (Hofer et al., 2022). In the Netherlands, persons with mental health problems also reported higher levels of negative impact of COVID-19 on their mental health and poorer ability to cope compared to people without mental health problems (Pan et al., 2021). Consequently, the COVID-19 pandemic and related measures may also be followed by negative experiences of people in drug addiction recovery.
The current study is part of a larger, multi-year longitudinal study of individuals in drug addiction recovery that was already initiated before the pandemic and continued during the pandemic. This timeline provides a unique insight into the impact of the pandemic on stability of people in recovery as it allows us to examine outcomes before and during the pandemic. Furthermore, two recent reviews established that many studies define relapse poorly, leading to contentiousness and vagueness around the concept (Moe et al., 2022; Sliedrecht et al., 2022). Therefore, in this article, we focus on past 12-month problematic alcohol or drug use among a drug addiction recovery cohort. Participants defined whether the use was problematic themselves. Revealing which factors are related to return to problematic use, particularly in an event like the COVID-19 pandemic, will provide insights into how services should sustain, and potentially improve, support for people in recovery during insecure times when access to treatment and support is restricted. Therefore, this article examines rates and (changing) risk- and protective factors for problematic substance use among individuals in drug addiction recovery in the period before (2018–2019) and during the COVID-19 pandemic (2019–2020).
2. Method
2.1. Study sample
Starting in 2018, we recruited a convenience sample of 722 adults from the Netherlands (N = 230), United Kingdom (N = 311), and Flanders (Belgium) (N = 181) (Best et al., 2018). Participants were included if they considered themselves to be in recovery from illicit drug addiction for at least three months at recruitment. We used the Life in Recovery survey (LiR) as a screening and recruitment instrument (Martinelli, Nagelhout, et al., 2020). The sample included persons in different stages of recovery: early (<1 year), sustained (1–5 years), or stable (>5 years). We recruited via available networks of recovery agencies and treatment services, social media, and snowball sampling.
Following the LiR, we performed a comprehensive baseline assessment with two follow-ups, measuring a range of recovery markers to map recovery pathways over time (Best et al., 2021). Each participant who left contact details in the LiR was invited to start with a baseline measure at the end of 2018 (N = 367), with follow-ups in 2019 (85 % of baseline cohort) and 2020–2021 (68 % of baseline cohort), outlined in Fig. 1. The last wave of data collection took place during the COVID-19 outbreak between November 2020 and March 2021, as Fig. 2 shows. Data collection involved online surveys or structured (telephone or face-to-face) interviews, depending on the participants' preference. Participants received 15 Euro or British pounds for each completed survey. Each country team ensured local ethics approval (METC Erasmus MC, the Netherlands; Sheffield Hallam University Ethics Committee, UK; Ethical Committee of Ghent University, Belgium). All participants provided informed consent.
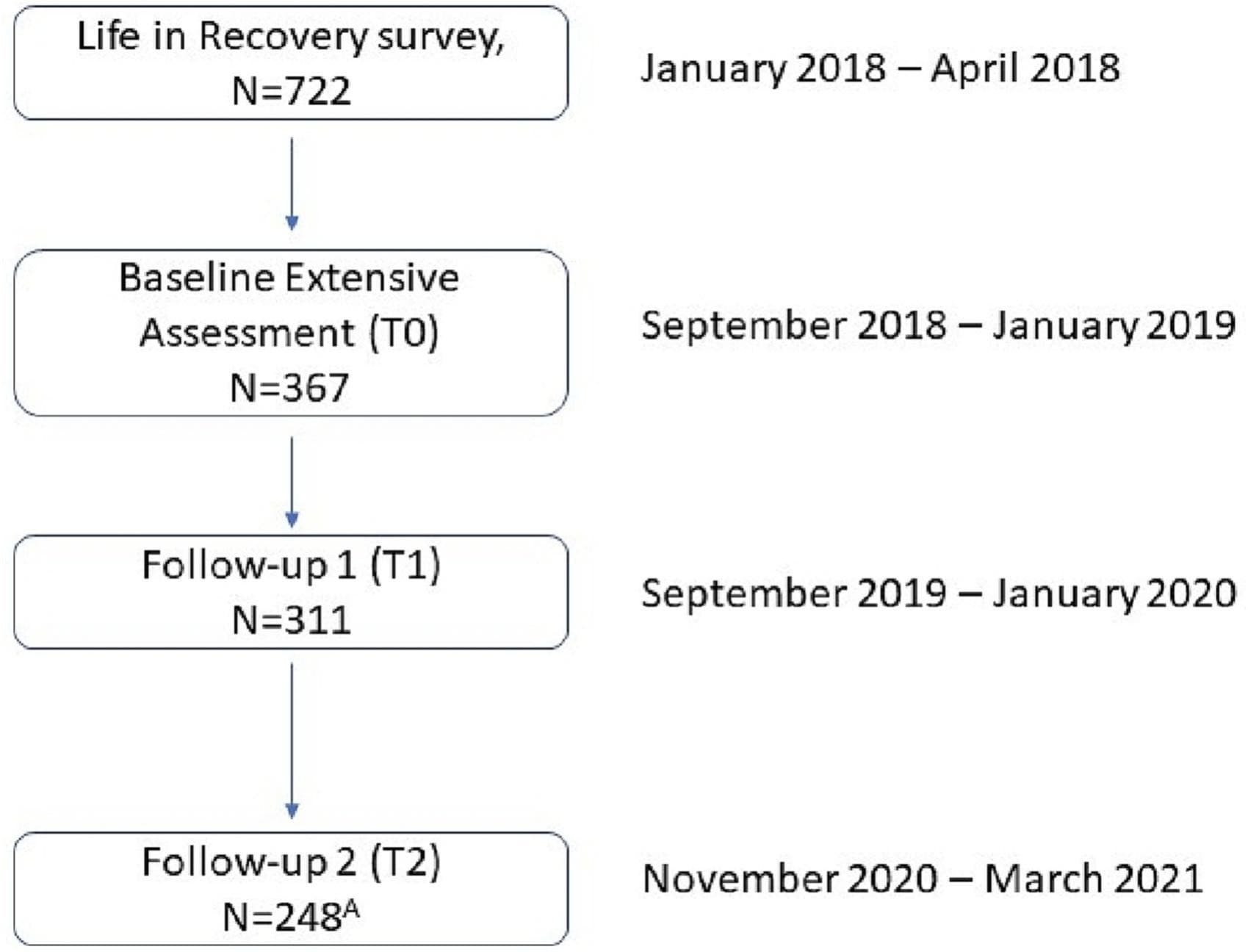
Fig. 1. Flow chart of data collection.
A Two participants from the final follow-up (T2) were excluded from analyses because of missing data.

Fig. 2. Daily confirmed cases of COVID-19 between July 10, 2020, and May 10, 2021, in the UK, Netherlands and Belgium and timing of measurements.
2.2. Procedures and measures
We obtained sociodemographic data (age, gender, and education level) and recovery stage from the LiR in 2018 (Fig. 1) (Martinelli, Nagelhout, et al., 2020). Furthermore, participants completed a questionnaire three times (Fig. 1). Each questionnaire included validated measures of substance use, involvement with formal and informal support services, recovery capital, quality of life, physical and psychological health, and social networks, which are described below.
2.2.1. Outcomes
Past 12-month problematic substance use was assessed by asking: “Have you used this substance PROBLEMATICALLY in the past 12 months?” [yes/no] separately for alcohol, cannabis, heroin, cocaine, crack, amphetamines, ecstasy/MDMA, and other drugs (open category). Although our sample consists of persons in recovery from illicit drug addiction, we have included problematic use of alcohol in the outcome measure because it is an addictive psychoactive substance and because research provides indications that so-called substitute use can potentiate relapse to former or new addictive behavior (Sinclair et al., 2021). We measured problematic alcohol or drug use at follow-up one (T1) and follow-up two (T2).
2.2.2. Risk- or protective factors for relapse
The study measured the variables described below at baseline (T0) and first follow-up (T1), which served as predictors at T0 for relapse at T1, and as predictors at T1 for relapse at T2 respectively in the regression analyses. In the GEE-analyses, we used these variables as time-varying variables (combining the measurements at baseline and follow-up).
Engagement with psychosocial support was measured by asking participants “Are you currently engaged with this kind of service/support?” [yes/no]: Mental health services, housing support, and employment service. ‘Yes’ to one of the items was scored as ‘yes’ for the variable.
Past 12-month negative life events consisted of eleven dichotomous items, derived from the Australian social networks and recovery (SONAR) study (Best et al., 2016), which asked whether participants had experienced impactful negative life events in the past 12 months: “death of a spouse”; “death of a close family member”; “death of a close friend”; “accident”; “witness a fatal overdose”; “own overdose”; “loss of a job”; “divorce”; “child taken into care”; “relationship separation” and; “eviction” [yes/no]. ‘Yes’ to one of the items was scored as ‘yes’ for the variable.
Social group membership (range 1–7, Cronbach's Alpha = 0.918) was assessed using the four-item (averaged) Exeter Identity Transition Scale (EXITS) about current group membership (Haslam et al., 2008). A higher score means that the participant agrees more with the statements about being a member of different social groups.
Recovery capital (range 1–6, Cronbach's Alpha = 0.838) was assessed with the Brief Assessment of Recovery Capital scale (BARC-10) (Vilsaint et al., 2017) and consisted of ten items (averaged) with a six-point Likert scale: strongly disagree to strongly agree. A higher score indicates more recovery capital.
We assessed commitment to sobriety (range 1–6, Cronbach's Alpha = 0.762) using the Commitment to Sobriety Scale (Kelly & Greene, 2014), which consisted of five items (averaged) with a six point Likert-scale: strongly disagree (1) to strongly agree (6). A higher score indicates a higher level of commitment.
Social support (range 1–7, Cronbach's Alpha = 0.878) was measured using four items (averaged) with a seven-point Likert scale. The items came from studies investigating the relationship between social identity and addiction recovery (Best et al., 2016; Haslam et al., 2005), asking about emotional support, help, resources, and advice received from other people. A higher score indicates more perceived social support.
Psychological health (range 1–5, Cronbach's Alpha = 0.915) was measured using a ten-item (averaged) scale from Maudsley's Addiction Profile (MAP) (Marsden et al., 1998). A higher score indicates better psychological health.
Self-stigma (range 1–5, Cronbach's Alpha = 0.841) was assessed through the eight-item (averaged) Perceived Stigma of Addiction Scale (PSAS) (Luoma et al., 2010). A higher score indicates more perceived self-stigma.
2.2.3. Covariates
Age was used as a scale variable defined in years.
Education level was assessed by asking participants “What is your highest educational qualification?” [Never went to or completed primary school/Primary level of education/Secondary level of education/Higher education]. Due to insufficient cases, the study combined the first three categories into one category: ‘lower education’.
Country was measured by asking participants “Where do you live?”. England, Wales, Northern Ireland, and Scotland were combined into one category: ‘the UK’.
Recovery stage was measured by asking “How long do you consider yourself in recovery?” [years, months]. We categorized this into three groups: early (<1 year), sustained (1–5 years), and stable recovery (>5 years). These stages of recovery are based on the model from the Betty Ford Institute Consensus Panel (Betty Ford Institute, 2007).
2.3. Analysis
The study team processed and analyzed the data using SPSS 27. To assess whether participants who were lost to follow-up differed from those who continued in the study, we compared characteristics between participants with and without follow-up data using chi square tests, independent sample t-tests, and Spearman's rho tests. A p-value <0.05 was considered significant. To assess to what extent the risk- or protective factors were associated with subsequent relapse, we performed prospective multivariate regression analyses, separate for each follow-up period. Furthermore, to assess whether the associations differed between waves, we performed generalized estimating equation (GEE) analyses and examined the interactions between predictors and follow-up wave while controlling for covariates. We omitted missing values from the analyses.
3. Results
The study sample (N = 367) had a mean age of 41.5 years (SD = 10.8) and consisted of 65 % men, spread over the UK (N = 118, 32 %), Netherlands (N = 136, 37 %) and Belgium (N = 113, 31 %). Among participants, 16 % were in early recovery (<1 year), 40 % in sustained recovery (1–5 years), and 44 % in stable recovery at baseline. Drop-out analyses revealed that compared to participants with data on the first follow-up (T1), participants without follow-up data were more often from the UK and Belgium, and reported membership of social groups less often. Participants without data on the second follow-up (T2), were also more often from the UK and Belgium, were educated to a lower level, and reported having less social support compared to participants with follow-up data (T2). No other statistically significant differences were found between participants who remained in the study versus those who dropped out.
As Table 1 shows, in the period between baseline and the first follow-up (before the COVID-19 pandemic), 19 % of participants had used substances problematically. In the period between the first follow-up and second follow-up (during the COVID-19 pandemic), 15 % of participants had used problematically. This difference was not statistically significant (Chi2 = 1.93, P = 0.165). Of the persons who reported problematic use at T2 (N = 36), 64 % (N = 23) also reported problematic use at T1.
Table 1. Characteristics of the study population at baseline and follow-ups.
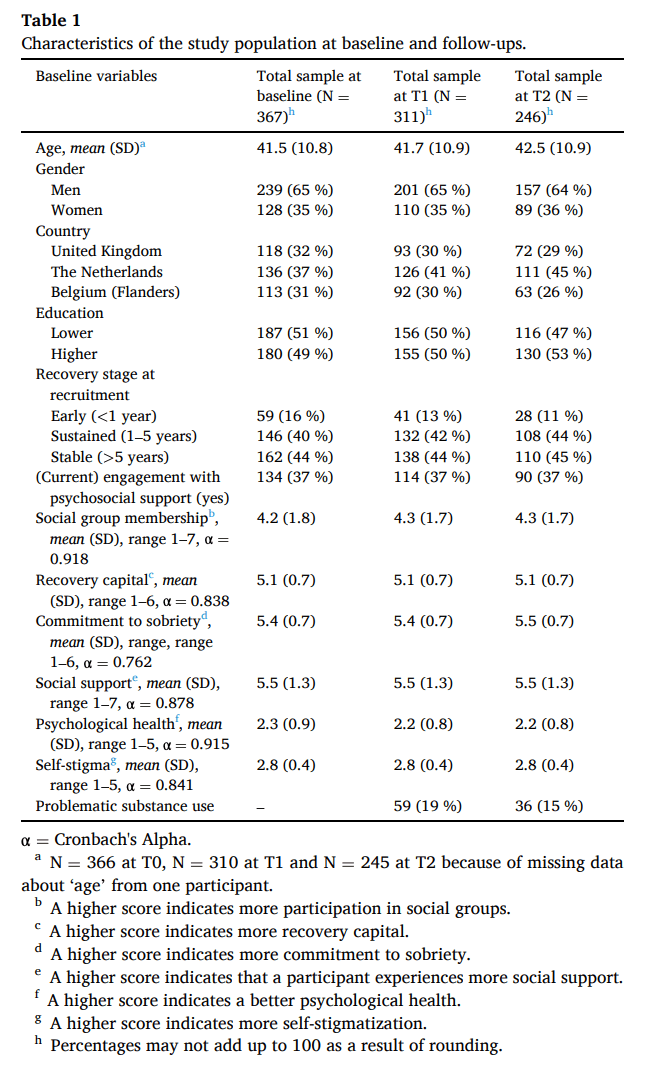
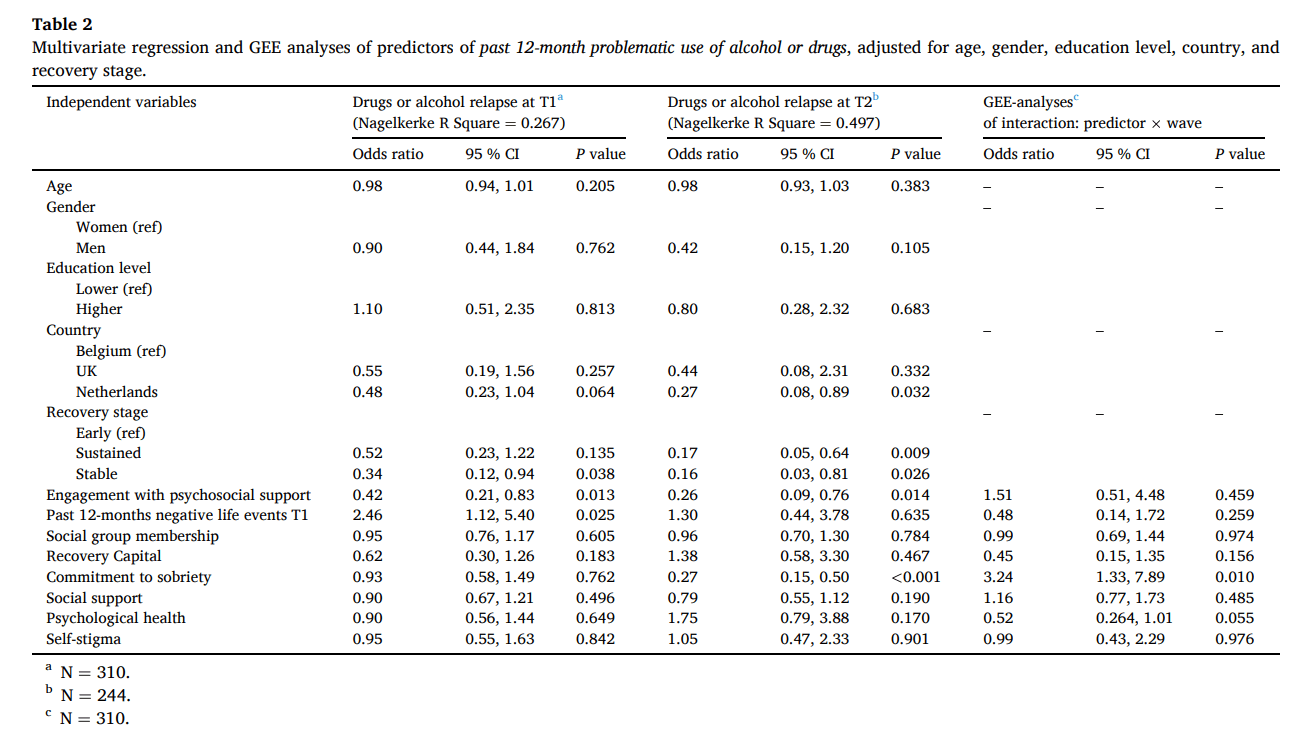
Table 2 shows that in the first period (before the COVID-19 pandemic), not engaging in psychosocial support at baseline and experiencing past 12-month negative life events is associated with higher odds of problematic substance use at T1 (before the pandemic). At T2 (during the pandemic), not engaging in psychosocial support and having less commitment to sobriety at baseline is associated with higher odds of relapse. Table 2 further shows that the relationship between commitment to sobriety and relapse differed between T1 and T2 (GEE: OR = 3.24, 95 % CI = 1.33, 7.89, P = 0.010). At T1, commitment to sobriety is not associated with problematic substance, while at T2 a lower commitment to sobriety is associated with higher odds of problematic use.
Table 2. Multivariate regression and GEE analyses of predictors of past 12-month problematic use of alcohol or drugs, adjusted for age, gender, education level, country, and recovery stage.
4. Discussion
This study builds on data from a multi-year longitudinal study that was initiated before, and continued during, the COVID-19 pandemic. This provides a unique insight into how the pandemic may have affected individuals in recovery from drug addiction. Among a cohort of persons in drug addiction recovery for some time—mostly persons in sustained (1–5 years) and stable recovery (>5 years)—rates of problematic substance use were approximately equal in the period before (19 %) and during (15 %) the COVID-19 pandemic. Furthermore, persons with the most time in recovery were the least likely to have used problematically, which is in line with a previous study comparing recovery outcomes between the same recovery stages (Martinelli, Nagelhout, et al., 2020). Although these rates appear low compared to previous literature on return to problematic use and relapse (McLellan et al., 2000; Miller et al., 2001; Moos & Moos, 2006), the comparability to such studies is limited. Return to problematic use or relapse is often pre-defined by the researchers (i.e., as any violation of abstinence) in such studies, and they often contain post-treatment study samples (Moos & Moos, 2006; Witkiewitz & Marlatt, 2007). The approximately equal problematic use rates are in line with a study that found that the pandemic did not affect recovery nor led to high rates of relapse for persons in recovery from alcohol use disorder (Gilbert et al., 2021). Still, the factors associated with problematic use in our study, differed before and during the pandemic. In the period before the COVID-19 pandemic, participants who did not engage in psychosocial support (with housing, employment, or mental health) at baseline and participants who experienced negative life events had higher chances of problematic use. In the period during the pandemic, participants who did not engage in psychosocial support and those with less commitment to sobriety had higher chances of problematic use.
Factors associated with problematic use and relapse can be categorized as either internal factors of the person (i.e., distress and self-efficacy) or external factors of the environment (i.e., social support and treatment engagement) (Marlatt & Gordon, 1985). Unlike before the pandemic, lower commitment to sobriety is associated with more chance of problematic use during the pandemic. Given that access to external resources, such as face-to-face contact with professional, social, and peer support, was limited during the pandemic (Bergman & Kelly, 2021; Blanco et al., 2020), internal resources, such as commitment, may have been needed more to prevent a return to problematic substance use. Thus, those with stronger commitment were potentially more resilient. Earlier studies found that commitment to sobriety is associated with more participation in mutual aid groups (Martinelli, van de Mheen, et al., 2020), a change in social identity (from ‘user’ to ‘in recovery’) (Dingle et al., 2019), and less substance use (Kelly & Greene, 2014) among people in addiction recovery. This suggests that mutual aid groups and other interventions aimed at social identity and commitment may increase internally driven resilience that is needed during a pandemic.
Both before and during the pandemic, engaging in psychosocial support is associated with lower risks of problematic substance use, suggesting continued support needs during recovery. Psychosocial factors, such as mental health, housing and employment, are important factors associated with recovery stability and progress (Martinelli, Nagelhout, et al., 2020; McQuaid & Dell, 2018). In line with our findings, engagement with such psychosocial support is also protective in studies of relapse (Vaillant, 1988). Our findings may indicate that persons in recovery continue to have long-term external support needs. In line with recovery literature, this suggests that support needs may continue to persist over time while in recovery (Ingram et al., 2022) and thus that continuous assessment of these needs and support may prevent return to problematic use (McKay, 2021).
4.1. Limitations
While we were able to recruit and retain a substantial recovery convenience sample over an extended period, the extent to which our findings are generalizable to the entire population of persons in (drug) addiction recovery is unknown. The sample size is also insufficient to conduct more in-depth analyses stratified by gender or recovery stage, for example. Second, for the outcome measure that was collected during the pandemic, the “past 12 months” also included a short period before the COVID-19 outbreak for some participants who responded early during the data collection. Thus, we do not know for all participants whether the problematic substance use occurred before or during the pandemic. This last follow-up is also two months further from the predictors compared to the first follow-up which may have affected the relation. Furthermore, while antecedent events and states may be predicting factors for problematic use, they may also be coincidental, or the consequence of third factors that triggered both the antecedent and the problematic use. Third, the retention rates in the last follow-up are significantly lower (68 %) compared to the first follow-up (85 %). We do not know which proportion of the population lost to follow-up used problematically in the last period. Thus, we do not know the problematic substance use rates of all participants during the COVID-19 pandemic. If all participants who were not followed-up would use problematically, the estimated relapse rate would have been around 43 %, while if none of the drop-outs at T2 use problematically the total relapse rate would be almost 10 %. This wide range and considerable uncertainty should be taken into account when interpreting the results. Despite this limitation, our findings are consistent with other studies that reported no increased rates of alcohol relapse during the pandemic. Problematic use rates may have been higher among the dropout-sample, as we expect that persons who returned to problematic substance use may not want to participate anymore in research about recovery. Another reason problematic use rates were not higher in the last follow-up is that participants may have gained more recovery experience over time, becoming more stable compared to the early stage. Fourth, the responses to the COVID-19 outbreak and infection rates differed among the participating countries (see Fig. 2). Thus, their impact on problematic substance use may have differed between countries. To compensate for this, we included country as a covariate in our main analyses. Finally, we let participants judge whether their use was problematic. On one hand, this can be seen as a weakness, as we do not know exactly what problematic use entailed (any violation of abstinence or return to heavy use over a certain period, for example). On the other hand, it can also be seen as a strength, as we allowed participants to put the experience in the context of their own lives and flow of behavior. In doing so, we may have avoided the binary “failure versus success” dichotomy, which Miller (1996) criticizes as an oversimplification of the addiction relapse process. Furthermore, this subjective measure allowed participants (instead of the researchers) to determine whether their substance use was problematic, putting their experience central. The survey and this measure explicitly, were discussed with persons with first-hand experience with drug addiction that were involved in the design of the study and who preferred this operationalization. The operationalization of relapse as self-reported problematic substance use may be useful in future studies to give insight into which factors shape stability in certain recovery domains. Its validity, however, may be strengthened by also juxtaposing results with less subjective measures of substance use. Further qualitative follow-up interviews with study participants who reported problematic substance use are crucial to our further understanding of why participants experienced their substance use as problematic.
4.2. Conclusion
In this study we explored how the COVID-19 pandemic may have impacted risk and protective factors for relapse. Despite anticipated negative effects (Da et al., 2020; Dunlop et al., 2020; Marani et al., 2021; Melamed et al., 2020; Volkow, 2020), but in line with another study focused on alcohol recovery (Gilbert et al., 2021), we found no evidence that people who were in recovery some time before the pandemic are more likely to return to problematic substance use during the pandemic compared to before the pandemic. This finding suggests that most people can sustain recovery, even in the context of significant adversity and reductions in access to (face-to-face) support. Still, we found that the relation between problematic use and commitment to sobriety differed between the two periods. During the pandemic, more commitment to sobriety is associated with lower chances of problematic substance use. This finding suggests that in events when access to external and social resources is limited, personal factors, including commitment, become more important for recovery stability. Therefore, personal factors and coping resources may serve as suitable intervention targets as they can be trained and developed with therapy (Kelly & Greene, 2014). Last, engaging in support services was protective for relapse, regardless of the pandemic. This finding points to the importance of keeping environmental resources available during events similar to the COVID-19 pandemic, which is crucial to mitigating the vulnerability of persons with less internal recovery resources.