Abstract
Altered reactivity to stress, either in the direction of exaggerated reactivity or diminished reactivity, may signal a dysregulation of systems intended to maintain homeostasis and a state of good health. Evidence has accumulated that diminished reactivity to psychosocial stress may signal poor health outcomes. One source of diminished cortisol and autonomic reactivity is the experience of adverse rearing during childhood and adolescence. The Oklahoma Family Health Patterns Project has examined a cohort of 426 healthy young adults with and without a family history of alcoholism. Regardless of family history, persons who had experienced high degrees of adversity prior to age 16 had a constellation of changes including reduced cortisol and heart rate reactivity, diminished cognitive capacity, and unstable regulation of affect, leading to behavioral impulsivity and antisocial tendencies. We present a model whereby this constellation of physiological, cognitive, and affective tendencies is consistent with altered central dopaminergic activity leading to changes in brain function that may foster impulsive and risky behaviors. These in turn may promote greater use of alcohol other drugs along with adopting poor health behaviors. This model provides a pathway from early life adversity to low stress reactivity that forms a basis for risky behaviors and poor health outcomes.
1. Introduction
Most models of stress reactivity and health outcomes assume that large stress reactions are harmful and that smaller responses are by definition better for the individual (Lovallo, 2005; Lovallo and Gerin, 2003). We have recently advanced the alternative hypothesis that both exaggerated and diminished stress reactivity indicate systems dysregulation with negative health implications (Carroll, et al., 2009; Lovallo, 2011). There has been little consideration of the pathways by which individuals become more or less stress reactive than normal. We will review data from our studies and others suggesting that one pathway to low stress reactivity is the experience of stressful or adverse circumstances in childhood and adolescence. Ultimately, this pathway may lead to disinhibited behavior that can increase risk for alcoholism and other substance use disorders.
This review will focus on studies of persons whose adverse experiences occurred in childhood and adolescence and who were studied as adolescents and young adults. We exclude studies of persons prenatally exposed to stress or those studied as infants, children, or in old age. With minor exceptions the review is confined to persons lacking serious psychiatric comorbidities. Although some studies have examined hypothalamic-pituitary-adrenocortical axis (HPA) reactivity using pharmacological challenges, we primarily confine this review to cortisol responses to behavioral and psychosocial stressors. We also exclude studies of recent but transient life stressors (Chida and Hamer, 2008; Luecken and Lemery, 2004) and touch only briefly on studies of resting or basal levels of cortisol secretion.
2. Adversity and stress reactivity in the Oklahoma Family Health Patterns Project
In a series of earlier studies conducted with patients undergoing alcoholism treatment at the VA Medical Center in Oklahoma City, we had observed that the alcohol treatment groups had lower cortisol and heart rate stress responses than matched controls (Bernardy, et al., 1996; Errico, et al., 1993; Lovallo, et al., 2000; Panknin, et al., 2002). Because these patients had an average daily alcohol consumption of approximately one fifth of hard liquor for 8-years, it was impossible to determine if the blunted stress reactivity of these patients was due to heavy drinking or some preexisting difference. Therefore, with the goal of exploring premorbid characteristics of persons at risk for alcoholism, we designed the Oklahoma Family Health Patterns Project (OFHP) to study healthy young adults with and without a family history of alcoholism (FH+ and FH−) who would therefore reflect either elevated or reduced risk for the disorder. With this goal in mind, we have recruited over 400 volunteers with an average age of 24 years, 58% women, who are free of psychiatric disorders including current abuse of alcohol and other drugs, and are nonobese. Because of limited initial data on FH characteristics, our organizing principle was to focus broadly on the emotions and associated behaviors since substance use disorders represent a failure to regulate motivated behavior. Accordingly data collection encompassed domains of personality and temperament, affect, cognition, behavioral regulation, and stress reactivity.
Our first and most pervasive finding was that FH+ are much higher in antisocial tendencies than FH− based on the California Personality Inventory Socialization Scale (CPI-So) (Sorocco, et al., 2006), indicating a pattern of risk taking and poor norm adherence (Sher, et al., 1991; Tarter, et al., 2004) with potential implications for risk for alcoholism. In our current sample, CPI-So sores are much lower for FH+ than for FH− persons (M ± SEM; 29.5 ± 0.37 vs 33.3 ± 0.31, respectively, t = 7.77, p << .00001), with low scores indicating low levels of socialization, norm adherence, and behavioral regulation reflecting a pattern of impulsive and disinhibited behaviors. The relevance of CPI-So scores for alcoholism risk is seen in a progressive relationship between low scores and a greater number of alcoholic relatives (Table 1).
Table 1
Persons high and low in sociability as a function of number of alcoholic relatives
CPI-So group | |||
> 30 | ≤ 30 | ||
FH− | 0 | 64 | 36 |
FH+ | 1 | 35 | 65 |
2 | 34 | 66 | |
3 > | 24 | 76 |
Note: A score of 30 is an empirically determined cutoff that separates relatively norm-abiding sample groups (> 30) from those that are less so (≤ 30), with lower scores indicating more antisocial tendencies (Gough, 1994). X2 = 104, p = 2.6 × 10−21
Recalling our earlier studies showing blunted stress cortisol responses in alcoholic patients, we then focused on adversity as a potential predictor of low reactivity prompted by work showing diminished reactivity in women exposed to traumatic stressors in adolescence (Carpenter, et al., 2007; Carpenter, et al., 2011). This rationale was also shaped by the influential work of Michael Meaney and others showing that variations in maternal nurturing or postnatal stress exposure could influence adult behavior and stress reactivity in rat models (Gutman and Nemeroff, 2003; Meaney, 2001). To assess adversity we drew on our subjects’ reports of socioeconomic status (SES) and their psychiatric data for reports of adverse experiences that were clearly not due to the subjects’ own behaviors but occurred due to the actions of others. We identified five questions that fit those criteria:
Have you ever been mugged or threatened with a weapon, or experienced a break-in or robbery?
Have you ever been raped or sexually assaulted by a relative?
Have you ever been raped or sexually assaulted by someone not related to you?
Before you were 15, was there a time when you did not live with your biological mother for at least 6 months?
Before you were 15, was there a time when you did not live with your biological father for at least 6 months?
Adverse experiences before age 15 and low SES were combined to form a three-level scale of low, medium, and high lifetime adversity. This scale resembles the self-report items assessed in studies by Caspi of maltreatment in the Dunedin cohort (Caspi, et al., 2002; Caspi, et al., 2003). We then examined our OFHP cohort of over 450 volunteers for stress reactivity, cognitive function and behavioral tendencies. The following summarizes our findings:
2.1 Early life adversity and diminished stress reactivity
Men and women in our high adversity groups showed diminished cortisol and heart rate responses to psychosocial stress (public speaking plus mental arithmetic) despite having normal diurnal cortisol curves (Figure 1) (Lovallo, et al., 2012). Significantly, preliminary analyses showed that the two largest predictors of stress cortisol responses were the subject’s sex followed by their experience of adversity. Figure 1 shows that relative to the group with no adversity, men experiencing two or more lifetime adverse events have a 40% reduction in cortisol response to our stressors and women have a 92%reduction (Cohen’s d’ = .38, and .41, respectively, indicating moderately large effect sizes). These values from our study may not generalize to other studies since the extent to which adversity has an impact on stress response would vary with different subject samples, methods of documenting adversity, and the stressors used. Reduced stress reactivity due to adversity, in the face of normal diurnal HPA regulation, implicates the stress axis at and above the hypothalamus as the portion of the system that is dysregulated in the high adversity group. This implies that brain areas including the limbic system, the amygdala and bed nuclei of the stria terminalis, along with medial and lateral prefrontal cortex are potentially affected in persons exposed to adversity. As noted elsewhere, these are brain regions involved in stress appraisals and shaping outputs to the body during states of stress (Lovallo, 2007). See Van Voorhees for a recent review of the impact of maltreatment on the HPA (Van Voorhees and Scarpa, 2004).
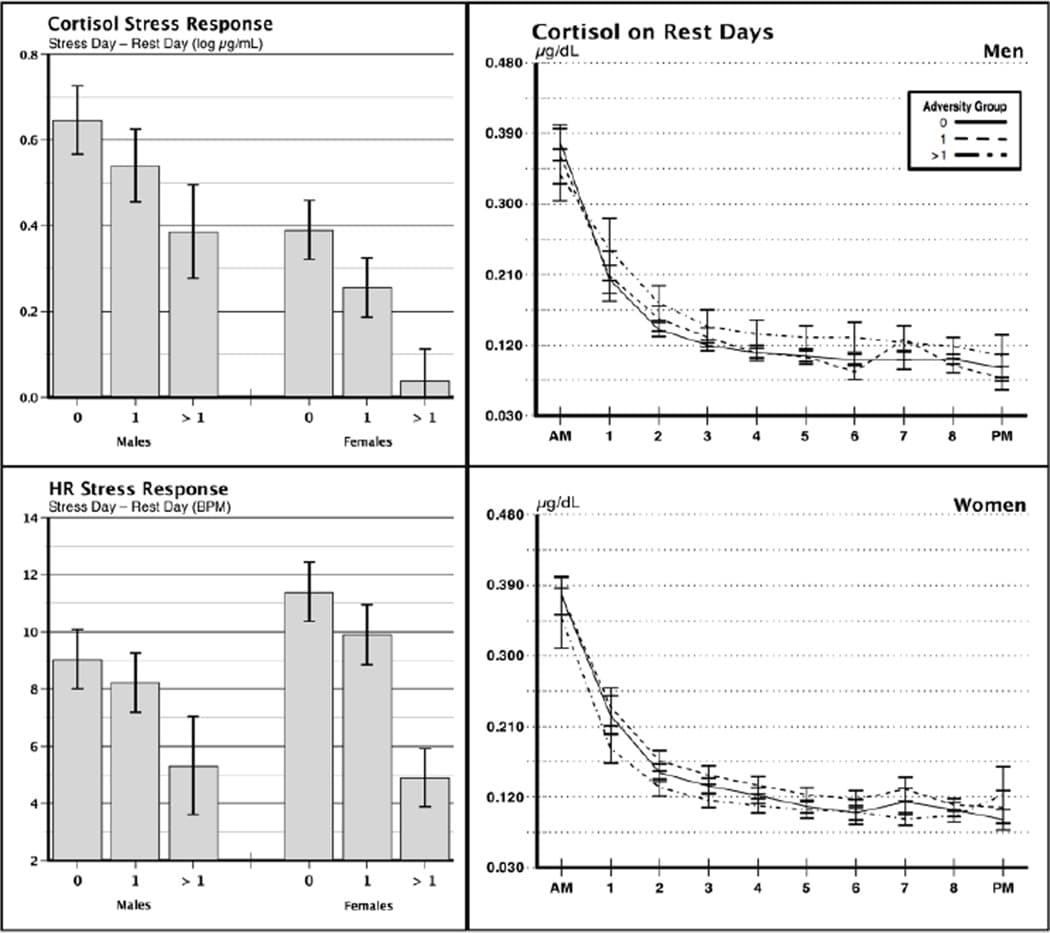
Figure 1: Cortisol and heart rate responses to psychosocial stress in persons low, medium, and high (0, 1, > 1) in lifetime adverse experience (Right Panels), and diurnal patterns of cortisol secretion in the men and women from the same adversity groups on a nonstress day (Left Panels). Subjects were exposed to 30 min of speech preparation and delivery (3 4-min speeches) and 15 min of mental arithmetic. Reprinted from “Lifetime adversity leads to blunted stress axis reactivity: studies from the Oklahoma family health patterns project,” by W.R. Lovallo, N.H. Farag, K.H. Sorocco, A.J. Cohoon, and A.S. Vincent, 2012, Biological Psychiatry, 71, pp. 344–349.
2.2 Early life adversity and altered cognition and behavior
In accord with the above list of possible brain regions reflecting the effects of adversity, we next explored whether exposure to adversity may have an impact on cognitive functions and behavioral tendencies. We observed that greater levels of adversity predicted: (1) higher interference scores on the Stroop color-word test (F = 3.07, p = .048), a measure sensitive to working memory capacity; (2) faster discounting of delayed rewards (F = 3.79, p = .024), a measure indicating a relatively immediate orientation to obtaining rewards and reduced self regulation; (3) lower Shipley mental age scores (F = 4.01, p = .019), a test of general intelligence; and (4) higher body mass indexes, in FH+ persons exposed to adversity (F = 3.40, p = .035), indicating a difference in eating habits and health behaviors (Lovallo, et al., In press). These effects were not explained by age, sex, race, education, or depression. Our results connecting adversity to poor working memory, impulsive behaviors, and lower general intelligence indicates that adversity during development has a long-term effect on central nervous system areas associated with decision-making and motivated behavior. Again, these would implicate lateral and medial prefrontal cortex and inputs from the septum and limbic system areas used in formulating motivations and adaptive responses.
2.3 Early life adversity and altered affect regulation
In keeping with our focus on emotions and motivated behavior, we next examined the impact of adverse experience on affect regulation and temperament. Persons higher in adversity were more likely to have antisocial tendencies as indexed by their CPI-So scores and Factor II (indexing antisocial and disinhibitory tendencies) from Lilienfeld’s Psychopathic Personality Inventory (Fs > 8.0, ps < .01) (Patrick, et al., 2006). Adversity was also associated with higher scores on the Eysenck Neuroticism scale and the Beck Depression Inventory (Fs > 10.0, ps < .01). Together these indicate that persons exposed to adversity during development are more disinhibited in their lifestyles, less socially connected, and have less stable mood regulation and more negative affect. Again, these results point to altered function in limbic system areas, the striatum, and medial prefrontal cortex.
2.4 Early life adversity in relation to risk for alcoholism
Since the population in the OFHP study is healthy and free of alcohol and other substance use disorders, we addressed whether adversity might be associated with greater risk of these disorders. We examined the FH composition of the OFHP adversity groups and saw that the proportion of FH+ persons was greater among groups experiencing greater degrees of adversity (Table 2, X2 = 67.1, p < .0001) (Lovallo, et al., In press). This indicates that the burden and consequences of early life adversity are likely to be borne most heavily by persons in families where alcoholism is prevalent.
Table 2
Levels of adversity in relation to family history of alcoholism
Adversity Group | |||
0 | 1 | 2 > | |
FH− | 86 | 63 | 26 |
FH+ | 14 | 37 | 74 |
Entries show percentage of FH+ vs. FH− persons in each adversity group. Columns add to 100%. Figures indicate that in the low adversity group, the preponderance of subjects are FH− while the high adversity group consists mainly of consists of 74% who are FH+. X2 = 67.1, p < .0001.
3. Integrative model
The present results reflect an impact of early adverse experience on a range of critical functions including stress axis reactivity, cognition, and emotional regulation, alterations that can contribute to impulsive behavioral tendencies, risk taking, poor health behaviors, and addiction risk. We summarize these relationships schematically in Figure 2. This constellation of results, incorporating components of the emotions and motivated behavior, are likely to derive from pervasive alterations in communication between the limbic system and the prefrontal cortex that then modify signals to the hypothalamus and brainstem during the generation of stress responses and formation of coping behaviors. We have discussed these relationships in terms of neurophysiological processes and specific brain structures (Lovallo, 2007; Lovallo and Gerin, 2003) and noted that altered stress reactivity can derive from three levels in the system: 1) the interpretation of events and choices of coping reactions at the level of cognitive processes (Everson, et al., 1995), 2) altered gain processes at the level of the hypothalamus, and 3) preclinical changes in peripheral physiology (Jennings, et al., 2004). Reduced stress reactivity is likely to diminish internal cues associated with danger when an individual confronts risky choices (Bechara and Damasio, 2002). Cognitive impairments and a reduced willingness to delay gratification may also contribute to risk-taking in daily life. Finally, unstable affect regulation and a tendency toward negative affect may also contribute to a behavioral style that seeks to redress this unease and dissatisfaction. Together, these may all plausibly contribute to an impulsive behavioral style and a greater willingness to take risks with a reduced aversion to the potential negative consequences. Over a period of years, these behavioral tendencies may contribute to risk for addiction and poor health behaviors more generally.
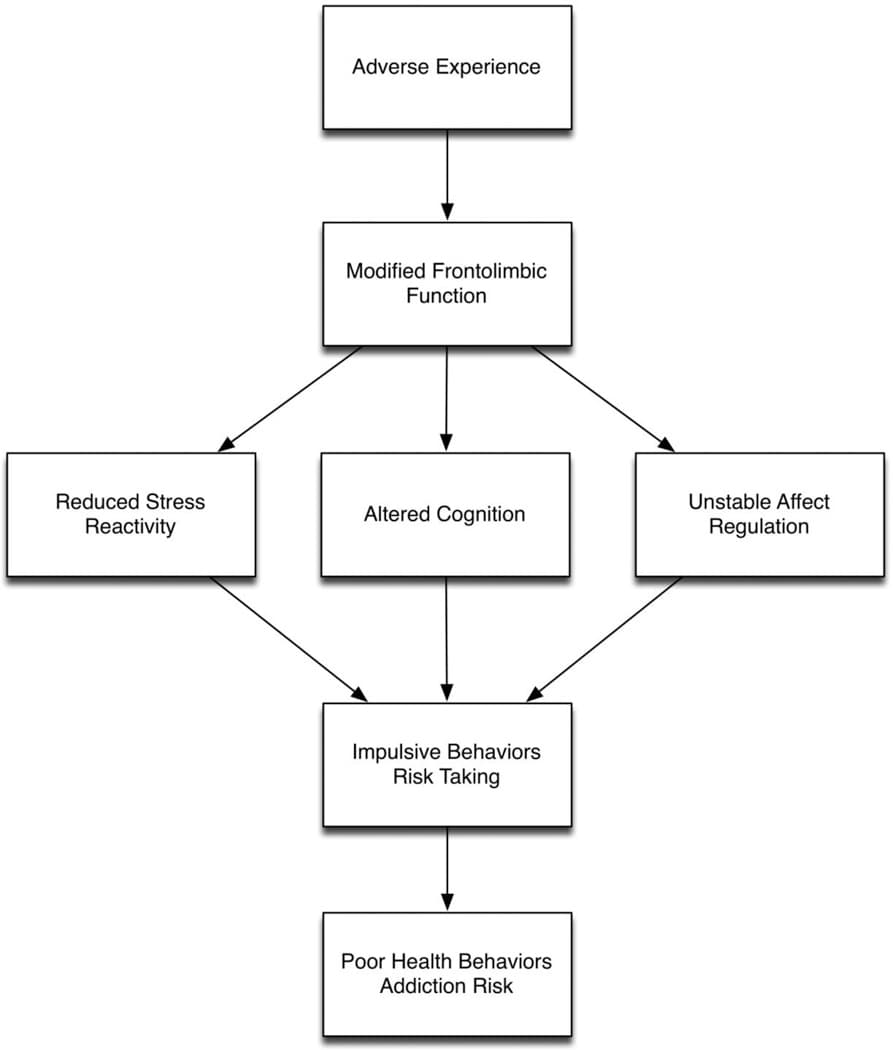
Figure 2: Pathway from adverse life experience to risky health behaviors. This conceptual model summarizes a series of steps through which the experience of stressful events in childhood and adolescence may alter behavior patterns in a way that can lead to adverse health outcomes. Life experience is seen as being processed through regions of the brain that evaluate ongoing events and shape coping behaviors and bodily responses that support these coping behaviors. These frontolimbic structures include key portions of the limbic system and the prefrontal cortex. Because these are areas whose functional connectivity is highly modifiabe by experience, there are at least three consequences of adverse experience based on empirical findings: 1) Stress reactivity is reduced; 2) Cognitive processing is shifted toward a focus on short term goals and a more impulsive response selection; 3) Regulation of affect is less stable and prone to negative states. It appears that these three immediate consequences of modified frontolimbic functions may result in an impulsive behavioral style that includes a tendency toward risk taking. Over the course of a lifetime, this behavioral style may have an impact on health through a tendency to use alcohol and other drugs and to engage in unhealthy behaviors such as smoking.
4. The impact of adversity on health and psychological and behavioral dysfunction
The effects of adverse rearing conditions have been studied in a number of other contexts, and these projects provide a framework for evaluating the data from the OFHP.
4.1 Adversity and reduced cortisol and autonomic reactivity to stress
A review of the literature indicates that there is substantial recent attention to the impact of early life adversity on the stress axis in early adulthood. As indicated in Table 3, we were able to find 9 papers, including our own study, showing that early adversity results in a blunting of cortisol responses to a variety of stressors, with the most common being public speaking and mental arithmetic (Carpenter, et al., 2007; Carpenter, et al., 2011; Elzinga, et al., 2008; Engert, et al., 2010; Gordis, et al., 2008; Kraft and Luecken, 2009; Lovallo, et al., 2012; Luecken, et al., 2009; MacMillan, et al., 2009). Few studies have examined the effect of adversity on autonomic responses although two reported diminished heart rate reactivity (Lovallo, et al., 2012; Murali and Chen, 2005). A minority of studies found that adversity produced either no impact on cortisol reactivity or an enhancement of reactivity (Kapuku, et al., 2002; Luecken and Appelhans, 2006; Moran-Santa Maria, et al., 2010; Murali and Chen, 2005).
Table 3
Papers reporting stress reactivity in adults in relation to types of abuse and adversity during childhood and early adulthood
Author | Date | N | Blunted response | Adversity | Stressor | ||
M | F | HR | CORT | ||||
Gordis | 2008 | 26 | 21 | X | physical, sexual, neglect | PS+MA | |
MacMillan | 2009 | – | 67 | X | physical, sexual, neglect | PS+MA | |
Lovallo | 2012 | 73 | 117 | X | X | physical, sexual, neglect | PS+MA |
Carpenter | 2007 | 6 | 17 | X | physical, sexual, neglect, emotional | PS+MA | |
Elzinga | 2008 | 23 | 10 | X | physical, sexual, neglect, emotional | PS+MA | |
Carpenter | 2011 | – | 20 | X | physical | PS+MA | |
Luecken | 2009 | 19 | 20 | X | poor family relationships | Role Play * | |
Engert | 2010 | 2 | 13 | X | low maternal care | PS+MA | |
Kraft | 2009 | 17 | 26 | X | divorce, low income | PS | |
Increase or No diff | |||||||
Luecken | 2006 | – | 45 | X | abuse, family conflict | PS | |
Heim | 2000 | – | 14 | X | physical, sexual | PS+MA | |
Moran-Santa Maria | 2010 | 19 | 22 | X | physical, sexual, neglect, emotional | PS+MA | |
Murali | 2005 | 62 | 38 | X | X | experience of violence | Debate, Puzzle Solving |
Kapuku | 2002 | 24 | – | X | low family SES | Video Game |
Note: Papers are based on comparisons of healthy controls and otherwise healthy persons experiencing abuse and adversity. Persons with psychiatric comorbidities are excluded. Sample sizes reflect the abused sample. PS = public speaking, MA = mental arithmetic
*Argue with “neighbor” about turning down loud music.
It appears difficult to find common factors to account for which studies did and did not find diminished reactivity in relation to experience of adversity. Most of the studies used public speaking alone or in combination with mental arithmetic to stress the subjects, a combination that produces a feeling of distress and reliably leads to an elevation of cortisol secretion (al'Absi, et al., 1997; Kirschbaum, et al., 1993). One study similarly used a role-playing scenario based on arguing with a neighbor about loud music (Luecken and Appelhans, 2006). Among studies not finding diminished stress reactivity with adversity, one assigned half the subjects to work on a difficult puzzle solving task and the other half to have a debate with the experimenter (Murali and Chen, 2005), the other used a video game (Kapuku, et al., 2002). In the study by Murali and Chen, the reported cortisol average following the challenges was a decline from baseline, suggesting that the responses as a whole were perhaps minimal. In the Kapuku study the average cortisol level increased to the video game. In short there is little evidence that the stressors were a primary factor in a failure to find a relationship Three other studies found no reduction in cortisol reactivity with adversity, although they used public speaking as a stressor. This overview indicates that the response characteristics of the stress axis can be reconfigured by the experience of adversity in childhood and adolescence, and this change leads to diminished reactivity in adulthood, although not all studies agree on this finding.
4.2 Diurnal cortisol and adversity
A smaller number of studies has examined the effect of adversity on diurnal HPA regulation in adulthood. These studies include daily secretion patterns as well as HPA activity in relation to awakening. As noted above, we found no effect of adversity on diurnal cortisol cycles in a large cohort of 354 men and women. Other studies have also found no effect of childhood trauma on diurnal secretion in adulthood (Klaassens, et al., 2009). Chen has reported that low SES combined with a sense of threat from the environment and perceived family disruption was associated with increasing daily cortisol output in children over a 2-year period (Chen, et al., 2010). One study reported that early sexual abuse by a family member contributed to decreased diurnal cortisol secretion (Brewer-Smyth and Burgess, 2008), and low basal cortisol secretion predicted risky decision-making in healthy volunteers(Takahashi, 2004), similar to a pattern seen in psychopaths (van Honk, et al., 2003). At present these studies are too few in number for definitive conclusions; sample characteristics differed, sample sizes were often small, and the measurement of cortisol levels, diurnal patterns or awakening responses varied. A recent review of adversity, antisocial tendencies, and reactivity (Hawes, et al., 2009) concluded that cortisol levels or diurnal patterns have a relatively weak link to adversity, relative to the more consistent impact of adversity on stress responses seen in the present overview.
4.3 Adversity, externalizing behaviors, altered cognition, and poor mood regulation
A large number of studies using different designs and methods have shown a connection between early life adversity, disinhibited behavior patterns, and future substance use disorders.
Family conflict and low levels of parental support relate to a range of the personality disorders in young adults (Klonsky, et al., 2000), and perceptions of poor parental care predicted habitual substance in high school students (Gerra, et al., 2004). However, externalizing disorders appear to be among the most common outcomes of early adversity, including increased aggressiveness in adolescence and young adulthood (Barnow, et al., 2002; Dohrenwend, 2000; Masten, et al., 1999; Maughan and McCarthy, 1997; Vaughn, et al., 2011). Physical maltreatment may have a causal relationship to development of antisocial personality disorder (Jaffee, et al., 2004). Also, early malnutrition contributes to aggressiveness, hyperactivity, and externalizing disorders in early adolescence (Liu, et al., 2004). Others have reported on disinhibited social behavior in internationally adopted children (Bruce, et al., 2009). A factor contributing to poor behavioral regulation in persons exposed to childhood adversity may be poor working memory, in which case diminished cognitive capacity is directly associated with poor behavioral regulation (Ginty, et al., 2011; Ginty, et al., 2012; Lovallo, et al., In press). These studies indicate that behavioral impulsivity can result from early adversity as part of a constellation of changes including reduced stress reactivity and poor cognitive function. Our OFHP data indicate that early adversity may affect a broadly normative group of persons with no history of psychopathology.
The importance of poor affect regulation as a risk factor for substance use disorders is illustrated in a longitudinal study of 18-year olds who reported heavy use of alcohol and experimentation with illicit drugs. Clinician ratings made at age 7 described these future heavy users as “maladjusted, insecure, and emotionally distressed.” At age 18, they were rated as: “undependable, irresponsible, unproductive, unable to delay gratification, rebellious, self indulgent, and ethically inconsistent,” and the authors concluded their heavy use was an expression of a “more fundamental, lifelong maladjustment” (Shedler and Block, 1990). Others have noted a clustering of risk taking, poor impulse control, and lack of positive affect as characteristic of drug abusers (Blum and Kozlowski, 1990). FH+ children are more likely to be lower in agreeableness and higher in impulsivity (Chassin, et al., 2004). Other work supports the association of disinhibitory early behavior as a predictor of adolescent unhealthy behavioral choices, including risky sexual behavior (Atkins, 2008) and early age of first drink (Kuperman, et al., 2005). Child abuse and household dysfunction predict psychological dysfunction and poor health outcomes including alcoholism, drug abuse, suicide, poor self-rated health, > 50 sexual partners, sexually transmitted disease, and obesity (Felitti, et al., 1998). Similarly, the likelihood of an alcohol use disorder is greater in persons with higher levels of psychological distress, neuroticism, childhood stressors, and behavioral under control (Jackson and Sher, 2003; Tarter, et al., 2004). Women with a history of sexual abuse were heavier users of alcohol, prescription, and nonprescription drugs and had initiated sexual intercourse before age 15 (Wilsnack, et al., 1997), indicating a co-occurrence of substance abuse and disinhibitory behavior in relation to early life abuse (Chapman, et al., 2007). Impulsivity is also associated with severity of pathological gambling among pathological gamblers (Alessi and Petry, 2003), and it also predicts disinhibited eating (Yeomans, et al., 2008).
These studies seem to suggest a pattern by which early life stressors contribute to behavioral disinhibition that can contribute to risk for addictive disorders.
4.4 Blunted stress reactivity, impulsivity, and risk for substance use disorders
Low levels of stress reactivity are associated a number of personal characteristics that are risk factors for substance use disorders, including poor mood regulation, impulsive behavioral tendencies, and risk taking. The experience of early adversity is an agreed contributor to development of psychopathic tendencies and blunted stress responsivity (Daversa, 2010). As noted, our own studies in alcoholics showed that alcoholic patients have diminished cortisol and cardiovascular stress reactivity (Bernardy, et al., 1996; Errico, et al., 1993; Lovallo, et al., 2000; Panknin, et al., 2002). But our earlier work did not address the question of the etiology of low stress reactivity and whether it might have been a consequence of drinking heavily or represent a preexisting characteristic. In a study of this etiology, adolescent boys from FH+ and FH− families were tested for cortisol responses to a psychological stressor and were typed as to temperament and behavioral tendencies. FH+ boys were more disinhibited and had lower stress cortisol responses than FH− boys (Moss, et al., 1995). Most importantly, the boys with low stress cortisol reactivity were more likely at ages 15–16 to be smoking and using marijuana than boys with more normative responses (Moss, et al., 1999), and low reactivity was more predictive of substance use than was family history. Tarter and colleagues formulated a model of adverse family influences on the antisocial characteristics of these offspring and their blunted stress reactivity as contributing to their increased substance abuse risk (Dawes, et al., 1999). Similarly, others have noted that reduced HPA reactivity may be predictive of risk of relapse risk to smoking (al'Absi, 2006) and alcoholism (Adinoff, et al., 2005; Lovallo, 2006). Similarly, drunk driving recidivists show blunted cortisol responses to stress (Couture, et al., 2008).
5. Brain function
Impulsivity and poor behavioral regulation in offspring from abusive families implicates subtle impairments of prefrontal cortex regulation over behavior that may persist into adulthood; in contrast, effective prefrontal function can contribute to adaptive regulation of emotional states and effective coping behaviors (Egan, et al., 2003). Although a lengthy discussion of frontolimbic mechanisms is beyond the scope of the present paper, a couple of points focus attention on mechanisms associated with personal experience that include decreased cortisol release, altered reward pathways, behavioral disinhibition, and risk for addiction. The key frontolimbic structures that determine the cortisol response to psychological stress are the amygdala, its outputs via the bed nuclei of the stria terminalis, the nucleus accumbens and the subgenual prefrontal cortex, and their collective outputs to the hypothalamus and brainstem. These structures are in turn regulated by cortisol feedback during states of stress (Lovallo, 2006). The adaptive purpose of this system is to motivate approach and avoidance behaviors. Dysregulation of these frontolimbic relationships can result in looser controls over motivated behavior with these consequences, poor regulation of affect, behavioral impulsivity, antisocial behavior, and a loss of motivational regulation leading to addiction.
Not surprisingly this motivational system is modifiable by experience, including exposure to stress (Heilig and Koob, 2007), such that stress-exposed animals are readily induced to self-administer alcohol and other drugs (Koob and Kreek, 2007). During acute stress, dopamine release at the nucleus accumbens is disinhibited by feedback from high levels of cortisol (Marinelli, 2007). Under this model, reduced cortisol secretion during stress could result in lowered cortisol feedback and less stimulation of dopamine release at the n. accumbens. George Koob has written extensively on the n. accumbens reward pathway and its role in the addictions, placing a central role on dopamine secreted at the n. accumbens during approach to anticipated rewards and following intake of all abused drugs (Koob, 2003). A deficiency of dopaminergic activity at the n. accumbens is thought to be accompanied by reduced experience of reward and potentially greater chronic dysphoria; while this reduced baseline may result in an enhanced hedonic response to the dopamine released following drug intake (Koob and Kreek, 2007). Pathological gamblers also show tonically reduced activation of the mesolimbic reward system (Reuter, et al., 2005). Under Koob’s model, stimulation of n. accumbens dopamine release could be seen as a way of reachieving hedonic homeostasis through drug or alcohol intake or stimulating behaviors. See McCrory for a recent review of these mechanisms (McCrory, et al., 2010).
Several threads of evidence indicate that stress exposure during development may affect brain structures needed for normal stimulation of cortisol release during stress. Severely traumatized children and adolescents exhibit smaller intracranial and cerebral volumes, smaller corpus callosum, and larger ventricles than controls (De Bellis, et al., 1999). Early maltreatment may affect development of the amygdala (Daversa, 2010), and children rated as disinhibited have smaller amygdala activations to unfamiliar faces (Schwartz, et al., 2003). We have shown reduced amygdala activation in FH+ persons who also had antisocial scores on the CPI-So scale, a measure that captures disinhibitory tendencies (Glahn, et al., 2007). Note that others have seen elevated amygdala activation to emotional faces in persons with low perceived SES, indicating that sources of altered limbic system reactivity and altered cortisol secretion remain to be fully understood (Aizenstein, et al., 2009). The foregoing suggests that stressful experience may alter development of critical brain structures in ways that can downregulate dopamine activity, potentially leading to disinhibited behaviors and a behavioral tendency toward stimulation of dopamine release through drug and alcohol intake and other behaviors.
6. Cause and effect?
The evidence above points to a pattern in which disrupted parenting, family discord, and related forms of adversity are associated with externalizing behaviors, risk taking, and a tendency to engage in substance abuse. This pattern raises the question of the respective roles of the environment, a genetic diathesis, or an interaction of the two. In the case of substance use disorders, there is a good deal of evidence for contributing family environment factors.
Physical maltreatment plays a causal role in the development of offspring antisocial behavior (Jaffee, et al., 2004) and conduct disorder (Foley, et al., 2004). Antisocial parents tend to be neglectful, leading to development of antisocial tendencies in the offspring (Eaves, et al., 2010). Twin studies indicate an effect of both environment and genetic factors on antisocial tendencies (Eaves, et al., 2010). Using a twin-adoption study, an adverse adoptive home environment contributed to increased adult antisocial behaviors, but this effect was stronger among adoptees from families with parental ASPD (Cadoret, et al., 1995). Variations in maternal warmth vs. coldness toward members of identical twin pairs reared together predicted differences in antisocial behavior problems (Caspi, et al., 2004). It is nonetheless difficult to eliminate the potential effect of small differences in twins’ behavior to influence the behavior of the mother.
In the OFHP study, we found a pervasive pattern of antisocial behavior and risk taking in the FH+ subjects, and this pattern was exaggerated in those with a larger number of FH+ relatives. Schuckit similarly reports increased adversity in FH+ families as contributing to alcoholism risk (Schuckit, et al., 2003). Statistical modeling indicates that environmental influences take precedence in causing internalizing symptoms following environmental stressors (Hicks, et al., 2009) but genetic risk factors also play a role in the emergence of externalizing disorders and alcoholism (Hicks, et al., 2009; Hicks, et al., 2004; Slutske, et al., 2002). In a large cohort “social causation” in the form of low SES was associated disproportionately with antisocial personality disorder (ASPD), depression, and substance use disorders (Dohrenwend, et al., 1992). Does this evidence indicate a greater genetic diathesis or a more adverse family environment as a cause of these outcomes? Our findings on the impact of adversity provide a partial answer; greater degrees of adversity had an effect in both FH− and FH+ groups, pointing to the likelihood that environmental factors are a significant contributor to the findings. Nonetheless, the impact of adversity is greater in the FH+ group because there is more of it.
Nonetheless, genetic polymorphisms may affect emotional reactivity of core limbic system structures such as the amygdala (Hariri, et al., 2005; Hariri, et al., 2002), and 5-HT transporter variants may affect amygdala-prefrontal coupling (Heinz, et al., 2005) raising the possibility that genes contribute to differential vulnerability to stress. The population prevalence of antisocial and disinhibitory behavioral patterns is associated with three genotypes, the short allele of the gene for the 5-HT transporter molecule, the low-activity allele of the gene for monoamine oxidase A (MAOA), and the high activity allele of the gene for catechol-o-methyltransferase (COMT) (Reif, et al., 2007).
A preponderance of studies has begun to favor a nuanced view of gene-environment interactions in determining risk for substance use disorders, with a significant role for parenting behaviors or other adverse influences acting on persons with genetic polymorphisms that confer vulnerability. The primary data on such gene-environment interactions shows differential vulnerability to early maltreatment in the form of adult violent behavior conferred by an allele of the MAOA gene (Caspi, et al., 2002) and a differential vulnerability to depression following early stress conferred by the serotonin transporter gene (Caspi, et al., 2003). Persons with other variants of these genes were found to be resistant to the effects of maltreatment. In another example of gene × environment interaction, in the val158met polymorphism of the COMT gene, val/val carriers are predisposed to poor working memory performance, and this cognitive alteration may confer differential vulnerability to environmental influences (Goldberg, et al., 2003). In a study of cocaine abuse, the short phenotype of the 5-HT transporter gene was a significant contributor to abuse potential, although the effect of the transporter allele depended on a pattern of poor perceived parental attachment and affection (Gerra, et al., 2007). The low activity allele of the MAOA gene confers greater vulnerability to conduct disorder in girls who experience early life adversity (Prom-Wormley, et al., 2009), and it contributes to increased aggression in maltreated children (Weder, et al., 2009), with similar findings by others (Enoch, et al., 2010).
Regardless of the initial source of the individual’s personal characteristics, conduct disordered children become poor parents and engage in assortative mating, perpetuating similar outcomes in their children through persistence of parenting styles and perhaps transmission of genetic polymorphisms (Ehrensaft, et al., 2004; Jaffee, et al., 2006). These recent findings provide a significant source of information on the potential for intricate feedback loops including disadvantageous rearing conditions, genetic vulnerabilities, and inherited forms of maladaptive parenting thus perpetuating the underpinnings of risky behavioral styles in future generations of offspring.
7. Protective effects
The prior review indicates a set of risk factors for substance use disorders. Other work indicates that some life-history factors may be protective against such outcomes, and that some persons may be less susceptible to adversity than others (Belsky and Pluess, 2009; Hinshaw, 1992). Constructive parenting styles contribute directly to positive adjustment in the offspring, engendering good parenting as adults (Kerr, et al., 2009). Positive parenting and parental warmth are positively associated with children’s effortful control and ego control (Eisenberg, et al., 2007; Eisenberg, et al., 2003). Similarly, social support moderates the ill effects of maltreatment (Kaufman, et al., 2004) and undercontrolled temperament (Adinoff, et al., 2005). Early childhood nurse home visits are also protective against antisocial behavior (Olds, et al., 1998). Maltreated children showed a flattened diurnal cortisol curve that became normal following a family-based therapeutic intervention (Fisher, et al., 2007) indicating a beneficial role for positive family behaviors in regulating HPA function in offspring. In addition to psychosocial factors, some genetic factors may be protective against the effects of early maltreatment as illustrated in the influential studies by Caspi and colleagues (Caspi, et al., 2002; Caspi, et al., 2003). Similarly an MAOA genotype associated with high levels of central 5-HTT is protective against the effects of maltreatment and adversity on antisocial behavior (Widom and Brzustowicz, 2006). These studies of protective effects reinforce our appreciation of the negative effects of adverse early life experience on health outcomes.
8. Implications for health behaviors
Social scientists carrying out studies of harsh social conditions and health outcomes have commented on the degree to which stress response systems may adapt to the social environment (Ellis, et al., 2006) a process termed “biological sensitivity to context” (Ellis and Boyce, 2008). The present study differs from their model in critical ways. Ellis and Boyce (2008) postulate a U-shaped function relating high, low, and high stress reactivity to rearing in benign, normal, and stressful environments, respectively. The data from the OFHP indicate greater stress reactivity in relation to benign rearing conditions, and decreasing reactivity as rearing becomes less benign. However, volunteers in the OFHP are not severely traumatized and none meets criteria for posttraumatic stress disorder. It is possible that the OFHP findings are not reflective of severe maltreatment and that exaggerated reactivity may emerge from severe maltreatment. A second difference in the OFHP and Ellis and Boyce models is that the latter was derived from assembling data from more than one study, whereas the OFHP data were from a single cohort with a range of adversity and who were all subjected to an identical stressor challenge.
However, within the range of relatively normal life experiences encompassed in the OFHP data set there are several possible implications for health and behavior. Data from the OFHP and several other studies indicate that persons exposed to adverse circumstances in childhood and adolescence may have reduced cortisol secretion to stress along with mild cognitive deficits, impulsive behavioral styles, and an unstable and negative affective disposition. Early stress exposure may alter dopaminergic signaling in the central nervous system, and this may result in a negative impact on health through three pathways. First, impaired cognition may result in poorer insight into the nature of possible threats and reduced exploration of alternative coping resources, two processes that are important when confronted with stressor challenges (Folkman and Lazarus, 1988; Lazarus and Folkman, 1984). Second, impaired recruitment of cortisol in response to stress may result in reduced dopamine activity during stress and may alter responses in critical brain systems that are sites of cortisol feedback. Third, these foregoing alterations may contribute to poor regulation of affect and a tendency toward negative affective states. Operating in concert these changes may plausibly contribute to less stable regulation of behavioral coping with challenge and may promote impulsive behaviors. This may accompany greater risk taking in the form of drug and alcohol abuse and poor behavioral choices that may impair health over the long term.