Abstract
The objective of this article is to provide an operational definition of recovery from alcohol use disorder (AUD) to facilitate the consistency of research on recovery and stimulate further research. The construct of recovery has been difficult to operationalize in the alcohol treatment and recovery literature. Several formal definitions of recovery have been developed but have limitations because 1) they require abstinence from both alcohol and substance use, 2) they do not include the DSM-5 diagnostic criteria for AUD as part of the recovery process (i.e., no focus on remission from AUD), 3) they do not link remission and cessation from heavy drinking to improvements in biopsychosocial functioning and quality-of-life constructs, and 4) they do not distinguish between alcohol and other drug use. The authors present a newly developed National Institute on Alcohol Abuse and Alcoholism (NIAAA) definition of recovery from DSM-5 AUD based on qualitative feedback from key recovery stakeholders (e.g., researchers, clinicians, and recovery specialists). The definition views recovery as both a process of behavioral change and an outcome and incorporates two key components of recovery, namely, remission from DSM-5 AUD and cessation from heavy drinking, a nonabstinent recovery outcome. The NIAAA definition of recovery also emphasizes the importance of biopsychosocial functioning and quality of life in enhancing recovery outcomes. This new NIAAA definition of recovery is an operational definition that can be used by diverse stakeholders to increase consistency in recovery measurement, stimulate research to better understand recovery, and facilitate the process of recovery.
Alcohol use disorder (AUD) is a complex and devastating disorder that causes myriad medical, psychological, social, economic, and personal problems. Currently, over 14.5 million Americans suffer from AUD (1). Problem drinking costs the United States more than $249 million annually (2), and it causes 95,000 deaths in the United States (3) and 3.3 million deaths worldwide (4) each year. Globally, alcohol misuse is the seventh leading risk factor for premature death and disability (5). Fortunately, many individuals recover from AUD through a wide variety of recovery pathways (6).
The purpose of this article is to present a new operational research definition of recovery that was developed by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) with input from key stakeholder groups. This definition will allow researchers, clinicians, and policy makers to define recovery using a common, operationalizable, and formal set of criteria that pertain specifically to individuals who recover from AUD. We briefly discuss the importance of defining recovery, review existing definitions, describe the methodology for developing the NIAAA definition, and present the final new research definition of recovery from DSM-5 AUD. We then elaborate on major components of recovery.
Importance of Defining Recovery
Currently, no agreed-upon definition of the term “recovery” exists in the alcohol treatment literature (7–9). The construct of recovery from AUD has been difficult to operationalize and measure in addiction research and has often involved various key stakeholders (e.g., patients, policy makers, and researchers) who have diverse perspectives on key domains of recovery (7). The development of a formal research definition of recovery that has broad consensus in the alcohol treatment field would be useful in several ways. First, it would provide a benchmark to consistently measure and standardize recovery research across studies and by various stakeholder groups. Second, it may assist in providing greater understanding of the clinical course of AUD by providing better characterization of the patterns of drinking and changes in AUD symptoms across time. Third, it can provide greater insights into the ways in which individuals respond to specific AUD treatment and intervention modalities by examining and defining short- and long-term trajectories of treatment response from those in recovery. Fourth, it can be studied from various theoretical orientations and diverse perspectives (e.g., economics/cost-effectiveness), which has the potential to enhance public perceptions and knowledge of the components that are involved in recovery.
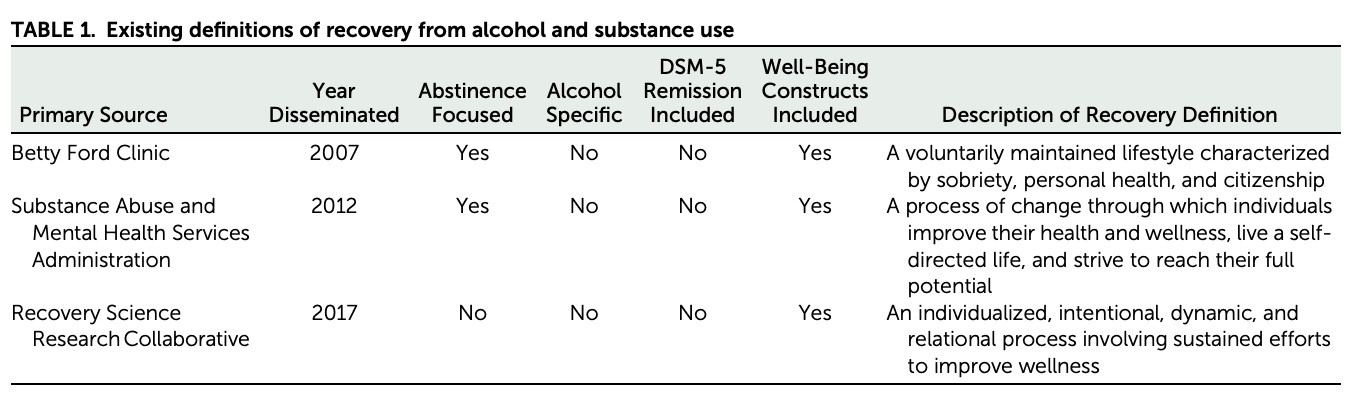
Several formal definitions of recovery from substance use disorders have been developed (10–13) (Table 1). Although these definitions are distinct, each centers on the notion that recovery is an ongoing process that consists of improvements in functioning and well-being and that abstinence from alcohol or other drug use is a necessary component (10–13). Despite the utility of these elements, these definitions have several limitations, with direct implications for enhancing research on recovery in the alcohol treatment field. Most definitions specify that complete abstinence from alcohol use should be the only goal in recovery. However, many people in recovery do not endorse abstinence as their recovery goal and may perceive abstinence as too high a bar and be deterred or discouraged from seeking or following through with treatment. Moreover, recent evidence indicates that individuals in recovery who engage in non-heavy drinking fare similarly to those who remain abstinent across indices of biopsychosocial functioning, alcohol-related risk factors, and other measures of well-being (14, 15) (see discussion of component 2 below). Current definitions also do not necessarily align with AUD criteria as set forth in DSM-5. Given that remission from DSM-5 AUD symptoms is considered integral to tracking the recovery process, DSM-5 criteria should be considered a central component of any definition of recovery (8). Similarly, although most of today’s definitions of recovery recognize that improvements in biopsychosocial functioning and well-being are integral to recovery, we know very little about how best to operationalize these constructs or how they interact and relate to other key recovery processes, such as cessation from heavy drinking or remission from DSM-5 AUD symptoms. We also have yet to determine which of these measures can be used to predict successful recovery (see discussion of component 3 below). Lastly, although most recovery definitions define recovery as an ongoing “process of change,” whereby individuals attempt to make positive changes in their lives, most recovery definitions do not provide clear benchmarks or other criteria on which to judge the degree to which these efforts have actually been successful. Thus, it is unclear from these definitions whether recovery has actually occurred for a given individual. Relatedly, because a definition of “recovered” is not offered in prior definitions, it is not possible to determine how long an individual has been recovered (or been in a state of remission). Overall, the development of a more formal research definition of recovery from DSM-5 AUD may bridge gaps in prior definitions and enhance conceptualizations of the recovery process.
TABLE 1. Existing definitions of recovery from alcohol and substance use
Methodology for Developing NIAAA Recovery Definition
The process of developing the NIAAA definition of recovery consisted of a series of steps, which are outlined in Figure 1.
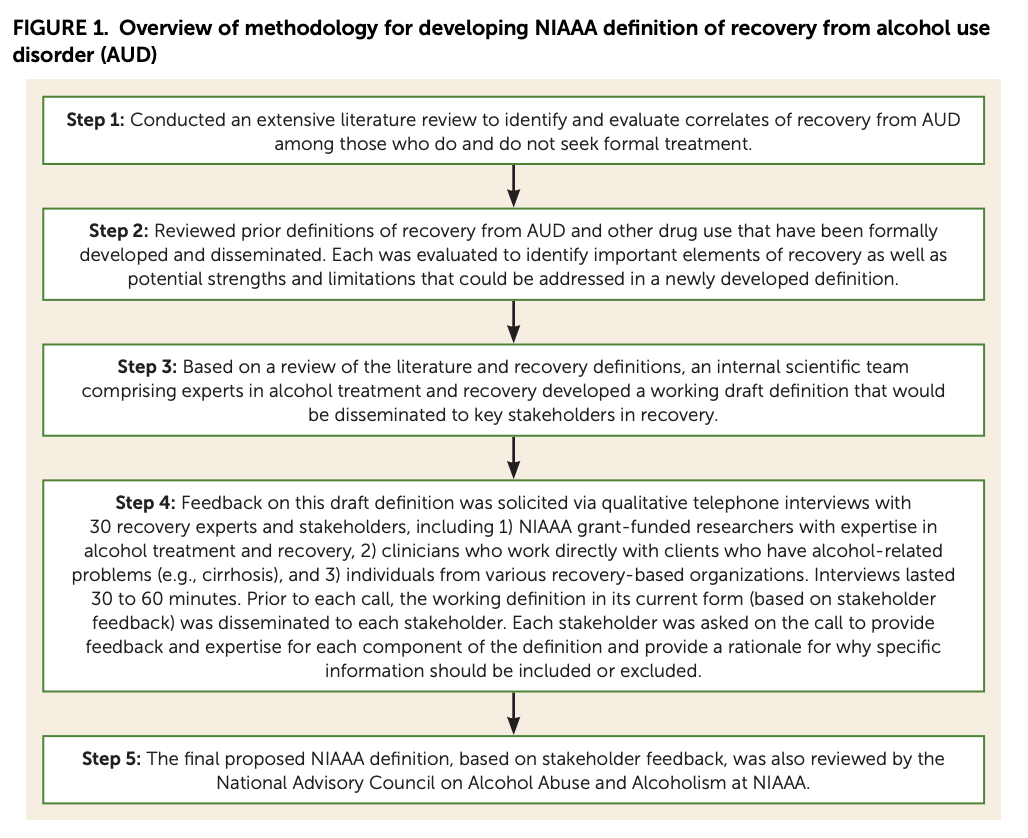
FIGURE 1. Overview of methodology for developing NIAAA definition of recovery from alcohol use disorder (AUD)
The Final NIAAA Definition of Recovery From DSM-5 AUD
The NIAAA research definition of recovery from AUD is provided in Figure 2. The definition also includes criteria for meeting its primary two components (see review of components in the next section): 1) remission from DSM-5 AUD, and 2) cessation from heavy drinking. Footnotes are provided for clarification and to define certain constructs.

FIGURE 2. Final NIAAA research definition of recovery from alcohol use disorder (AUD) and definitions of its components: cessation from heavy drinking and remission from DSM-5 AUDa
NIAAA Definition of Recovery
“Recovery is a process through which an individual pursues both remission from AUD and cessation from heavy drinking. Recovery can also be considered an outcome such that an individual may be considered ‘recovered’ if both remission from AUD and cessation from heavy drinking are achieved and maintained over time. For those experiencing alcohol-related functional impairment and other adverse consequences, recovery is often marked by the fulfillment of basic needs, enhancements in social support and spirituality, and improvements in physical and mental health, quality of life, and other dimensions of well-being. Continued improvement in these domains may, in turn, promote sustained recovery.”
In refining the final definition, NIAAA recognizes that “recovery” is both an ongoing process and an outcome/endpoint or a primary marker of success (subject to duration qualifiers; see the section on DSM-5 AUD remission below for a review of qualifiers). The definition then specifies that achieving two components is necessary to demonstrate that an individual has recovered, namely, remission from AUD and cessation from heavy drinking (see components 1 and 2 below). Because recovery is both a process and an outcome, an individual who does not remit from AUD or an individual who exceeds the heavy drinking criteria (e.g., has a heavy drinking day) would not meet the outcome portion of the definition but could still meet the process portion of the definition, provided the individual is still pursuing both remission from AUD and cessation from heavy drinking. Importantly, the definition acknowledges that recovery is associated with greater well-being and enhancements in biopsychosocial functioning (i.e., basic needs, enhancements in social support and spirituality, and improvements in physical and mental health and quality of life; see component 3 below). Several other empirically supported dimensions of well-being are highlighted, such as enhancing self-care, personal growth, subjective experiences (e.g., happiness), engagement in the community, and concern for others, that reflect the experiential processes of those in recovery from alcohol use (7) (see Figure 2 footnotes). Stakeholder feedback stressed the importance of incorporating well-being and biopsychosocial functioning constructs as integral to any definition of recovery. However, additional research is needed to better define the link between these constructs and recovery from AUD. Thus, the well-being and biopsychosocial functioning constructs, albeit important, are considered ancillary in the definition of recovery until additional research can address how best to operationalize these constructs, identify threshold values to mark clinically meaningful progress, and identify the constructs that are most integral to success in recovery from DSM-5 AUD.
Component 1: Definition of Remission From DSM-5 AUD
“Remission from alcohol use disorder (AUD), as defined by DSM-5 criteria, requires that the individual not meet any AUD criteria (excluding craving). Remission from AUD is categorized based on its duration: initial (up to 3 months), early (3 months to 1 year), sustained (1 to 5 years), and stable (greater than 5 years).”
The first component of the NIAAA recovery definition incorporates DSM-5 AUD remission guidelines (16), stating that individuals who have recovered should no longer meet any AUD diagnostic criteria (except craving). Four remission duration qualifiers are provided to reflect the two DSM-5 AUD qualifiers but include further subdivisions to demarcate temporal milestones where the risk of relapse may particularly decrease during the recovery process. The duration qualifiers are “initial” (up to 3 months; i.e., a highly unstable period when individuals are at the greatest risk for relapse [17]), “early” (3 months to 1 year; i.e., a still tenuous but relatively more stable period that matches the DSM-5 qualifier), “sustained” (1–5 years; i.e., a period of greater stability), and “stable” (greater than 5 years; i.e., when individuals in recovery are more likely to remain in remission) (18, 19).
Component 2: Definition of Cessation From Heavy Drinking
“Cessation from heavy drinking is defined as drinking no more than 14 standard drinks per week or 4 drinks on a single day for men and no more than 7 drinks per week or 3 drinks on a single day for women. Cessation from heavy drinking can be categorized based on the duration: initial (up to 3 months), early (3 months to 1 year), sustained (1 to 5 years), and stable (greater than 5 years).”
The second component of the NIAAA definition of recovery incorporates cessation from heavy drinking (see Figure 2), based on NIAAA’s empirically based no-heavy-drinking daily and weekly guidelines (20). The guidelines provide recommendations for both men and women with regard to daily or weekly limits that one should not exceed to engage in non-heavy drinking. This second component includes the same duration qualifiers as component 1, thus providing consistency and standardization across both components. Because there is no amount of drinking without risk, footnotes in Figure 2 are provided to highlight this important caveat, particularly for certain vulnerable populations. The footnote also highlights that physical, mental, and functional well-being are expected to result from the cessation of heavy drinking.
Primary Components of Recovery from AUD: Elaboration and Importance
Component 1: Remission From DSM-5 AUD in Recovery
Remission from AUD symptoms has long been considered integral to recovery (6, 21, 22). DSM-5 includes 11 AUD diagnostic criteria that reflect the deleterious effects of hazardous alcohol use on biological and psychosocial functioning (16). A diagnosis of a DSM-5 AUD is made by endorsing two or more AUD criteria within the past year. The severity of disease is determined by the number of criteria: two to three indicate “mild AUD,” four to five indicate “moderate AUD,” and six or more indicate “severe AUD.” Of the 11 criteria, several are associated with clinically meaningful changes in psychosocial functioning and well-being (e.g., continued drinking despite its causing problems with families and loved ones). Thus, improvements in psychosocial functioning criteria can also serve as markers of progress toward recovery. Additionally, the DSM-5 AUD diagnostic guidelines include two remission duration qualifiers—“early” and “sustained”—based on how long the individual has ceased to show AUD symptoms (16). Individuals who meet the “early remission” duration qualifier have been symptom free (except for craving) for more than 3 months and less than 12 months. Those who meet the “sustained remission” duration qualifier have been symptom free (except for craving) for at least 12 months. These qualifiers can be useful for capturing the stability of AUD symptom improvement across time. Incorporating DSM-5 AUD criteria into a formal definition of recovery also provides a unique opportunity to track changes in symptoms and psychosocial functioning throughout the recovery process, with clear benchmarks on which to judge the degree to which recovery has actually occurred.
Component 2: Cessation From Heavy Drinking in Recovery
Current definitions of recovery from AUD and other drug use signify that maintaining abstinence is critical to successful recovery (7, 10, 11). Indeed, abstinence is considered the optimal goal and outcome for those in recovery (23). Research shows that individuals who achieve abstinence in recovery experience the most significant improvements in psychosocial functioning, quality of life, and physical health (24–26). However, a growing body of research has shown that nonabstinent reductions of drinking are also associated with clinically meaningful improvements in physical health and well-being (15, 27–33). For example, Kline-Simon et al. (15) monitored the long-term progress of individuals following AUD treatment and found that those who achieved abstinence or no heavy drinking after treatment had, on average, similar health care utilization outcome costs at 5 years posttreatment and similar psychosocial functioning outcomes at 1 and 9 years posttreatment. Moreover, both abstainers and non-heavy drinkers had, on average, greater improvements in these outcomes than heavy drinkers. Indeed, the cessation of heavy drinking has been adopted by NIAAA in its alcohol use guidelines (i.e., non-heavy drinking is defined as drinking no more than 14 standard drinks per week or four drinks on a single day for men and no more than seven drinks per week or three drinks on a single day for women) and in guidance by the U.S. Food and Drug Administration (FDA), which defines cessation from heavy drinking as treatment success, to be used as a primary endpoint in pivotal pharmacotherapy trials for AUD (20, 34). As such, adoption of the empirically validated NIAAA non-heavy drinking guidelines within a definition of recovery can expand drinking thresholds of previous recovery definitions.
It should be acknowledged, however, that the heavy drinking threshold used in the recovery definition, as with any cutoff used to create a dichotomous outcome, draws a “line in the sand” on a continuous construct (i.e., number of drinks consumed per week and number of heavy drinks in a day), and there may be other cutoffs that could have been used to delineate heavy drinking in the recovery definition. For example, NIAAA considered alternatives to the cutoff of three to four drinks on a single day (used to define a “heavy drinking day”). However, we could not justify using other cutoffs, such as a cutoff of five to six drinks, because the three-to-four-drink cutoff has received the largest body of empirical support for its validation in terms of its health consequences, with significantly less support for other cutoffs. Moreover, this cutoff is correlated with blood alcohol levels by which an average person could be considered “intoxicated,” which increases the risk of adverse consequences (20, 35).
NIAAA also considered a two-level reduction in World Health Organization (WHO) drinking risk levels as a potential drinking threshold, instead of cessation of heavy drinking, as there is increasing evidence for its validity as an endpoint in clinical trials (36–38). However, NIAAA believes that this endpoint would not be appropriate as an outcome on which to judge that an individual has “recovered,” because a successful “responder” on this endpoint could still be drinking at quite high levels and, while improved from baseline, could still be experiencing quite a high number of consequences. For example, individuals who are in the WHO very-high-risk drinking level at baseline and then reduce to the WHO medium-risk drinking level after treatment would be considered “responders” on this endpoint. However, they could still be averaging more than four drinks per day, which would likely include multiple heavy drinking days (because this quantity is typically obtained by averaging daily drinking over 4 weeks and then dividing by 28 days). Thus, even though these individuals may have substantially reduced their drinking and showed clinical improvement, the possibility of multiple heavy drinking days may still be associated with alcohol-related harms (particularly physical harm), and thus these individuals would not be considered “recovered” using the NIAAA definition.
Component 3: Biopsychosocial Functioning and Quality of Life in Recovery
Inherent to most definitions of recovery from AUD and other drug misuse is the notion that improvements in biopsychosocial functioning and well-being are markers of recovery and are critical for continued success in recovery (8–10, 24, 39). For example, the Recovery Science Research Collaborative, an interdisciplinary collaboration of recovery researchers and other stakeholders, operationally defined recovery as “an individualized, intentional, dynamic, and relational process involving sustained efforts to improve wellness” (10). Additionally, the Substance Abuse and Mental Health Services Administration also developed a definition of recovery from substance use disorder, defined as “a process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential” (12). Moreover, the Betty Ford Institute convened a consensus panel in 2007 comprising various recovery stakeholders and defined recovery as “a voluntarily maintained lifestyle characterized by sobriety, personal health, and citizenship” (11). From a research perspective, the inclusion of biopsychosocial functioning and enhancements in quality-of-life criteria provides a way to define more precisely what constitutes recovery and may afford the opportunity to identify thresholds that might mark clinically meaningful improvements in well-being that affect recovery. Overall, each of these frameworks highlights the importance of biopsychosocial functioning and well-being as integral to maintaining success in recovery and acknowledges that recovery is a dynamic and heterogeneous process and that improving one’s well-being is intentional and multidimensional.
Concluding Remarks
NIAAA’s newly developed formal research definition of recovery extends prior definitions by incorporating key empirically supported alcohol-related processes (i.e., remission from DSM-5 AUD and cessation from heavy drinking). It permits non-heavy drinking as progress toward a successful outcome, recognizing that recovery is an ongoing process. It also supports aspects related to empirically supported improvements in well-being and biopsychosocial constructs that have been linked to successful drinking outcomes in treatment and recovery. By adopting a uniform definition, researchers and health care professionals can more precisely operationalize and measure recovery-related processes. This will allow us to conduct more consistent and accurate comparisons across different studies and settings. Although this definition should help standardize how we view and measure recovery, NIAAA expects to continue to refine it over time. Research is encouraged to better understand how aspects of well-being and biopsychosocial functioning, remission from AUD, and cessation from heavy drinking affect recovery. For example, research is needed to identify which are the most reliable and valid measures of well-being, quality of life, and biopsychosocial functioning that accurately predict successful drinking and recovery outcomes. It would be important also to evaluate how the NIAAA daily and weekly drinking guidelines predict recovery outcomes in relation to other empirically supported non-heavy drinking practice guidelines (e.g., the WHO drinking guidelines). Moreover, a detailed understanding of the unique typologies (e.g., improvement in certain areas of quality of life) and risk of relapse that characterize each of the four remission duration qualifiers will provide a greater sense of their reliability and validity in profiling different phases of recovery. Ultimately, NIAAA’s goal in developing this definition is to provide a useful framework to advance recovery science and the treatment of AUD.