Abstract
Studies have yielded mixed findings regarding changes in adolescent substance use during the COVID-19 pandemic; some report increased alcohol and cannabis use, others show less binge drinking and vaping behaviors, and others no change. In 2019, only 8.3% of the 1.1 million adolescents with a substance use disorder received specialized treatment. Treatment rates for 2020 have not yet been published. Stay-at-home orders and social distancing guidelines put into place in March 2020 caused the partial closure of many outpatient substance use clinics. The implications of this treatment suspension and special considerations for working with adolescents during stay-at-home orders are discussed.
Key points
The impact of the COVID-19 pandemic on adolescent substance use is not clear, because emerging studies have yielded inconsistent results.
The COVID-19 pandemic has significantly disrupted daily life for adolescents, leading to increased stress, social isolation, boredom, anxiety, and depression, all of which are risk factors for adolescent substance use.
Stay-at-home and social distancing orders might create unexpected benefits for reducing adolescent use.
The full impact of partial clinic closures on substance abuse treatment for adolescents is currently unknown. Special considerations should be taken by clinicians working remotely with adolescents.
Although substance abuse treatment may be affected by clinic shutdowns, health care workers may use adolescents’ lack of access to substances as a means for setting substance cessation goals.
Adolescence is a critical period for social and emotional development. Important tasks during this time include fashioning a social identity, developing a degree of emotional and personal independence from parents and caregivers, and moving toward self-reliance.1 The coronavirus disease 2019 (COVID-19) pandemic has caused tremendous upheaval and disruption of this process. Since March 2020, most teens have been unable to go to school in person, interact with peers, or engage in sports and extracurricular activities. Traditional milestone events like prom, graduation, and going away to college have been missed. Many teens have had to take on childcare duties, such as caring for younger siblings while their parents work. Remote schooling requires hours of screen time and remaining engaged and motivated can be difficult. Sheltering in place is a drastic shift for adolescents who are accustomed to spending much of their time with peers, teachers, coaches, and others. The loss of routine and few opportunities to take healthy risks or to express developmentally appropriate independence may be slowing the individuation process that is a critical part of adolescence.2 It is unsurprising that pandemic-related isolation, uncertainty, and fear are leading to increased depression, anxiety, stress, and boredom and it is possible that a new cohort of adolescents may be at heightened risk for developing substance use disorders.3 , 4
Substance use prevalence before the COVID-19 pandemic
Experimentation with alcohol and drugs often begins during adolescence,5 and in nonpandemic times alcohol and drug use by adolescents are quite common. The Monitoring the Future (MTF) survey, administered annually to middle and high school students across the United States, asks about substance use and attitudes toward various drugs. According to results from the 2019 MTF survey by the time teens reached their senior year of high school more than 50% reported alcohol use, more than 40% had vaped, and about 36% had used cannabis in the past year. The use of other substances was fairly low. Table 1 shows the percentage of twelfth graders reporting past year use of various substances in 2020 compared with 2019.6
Table 1.
Past-year prevalence rates of various substances reported by twelfth graders in the 2019 and 2020 MTF surveys
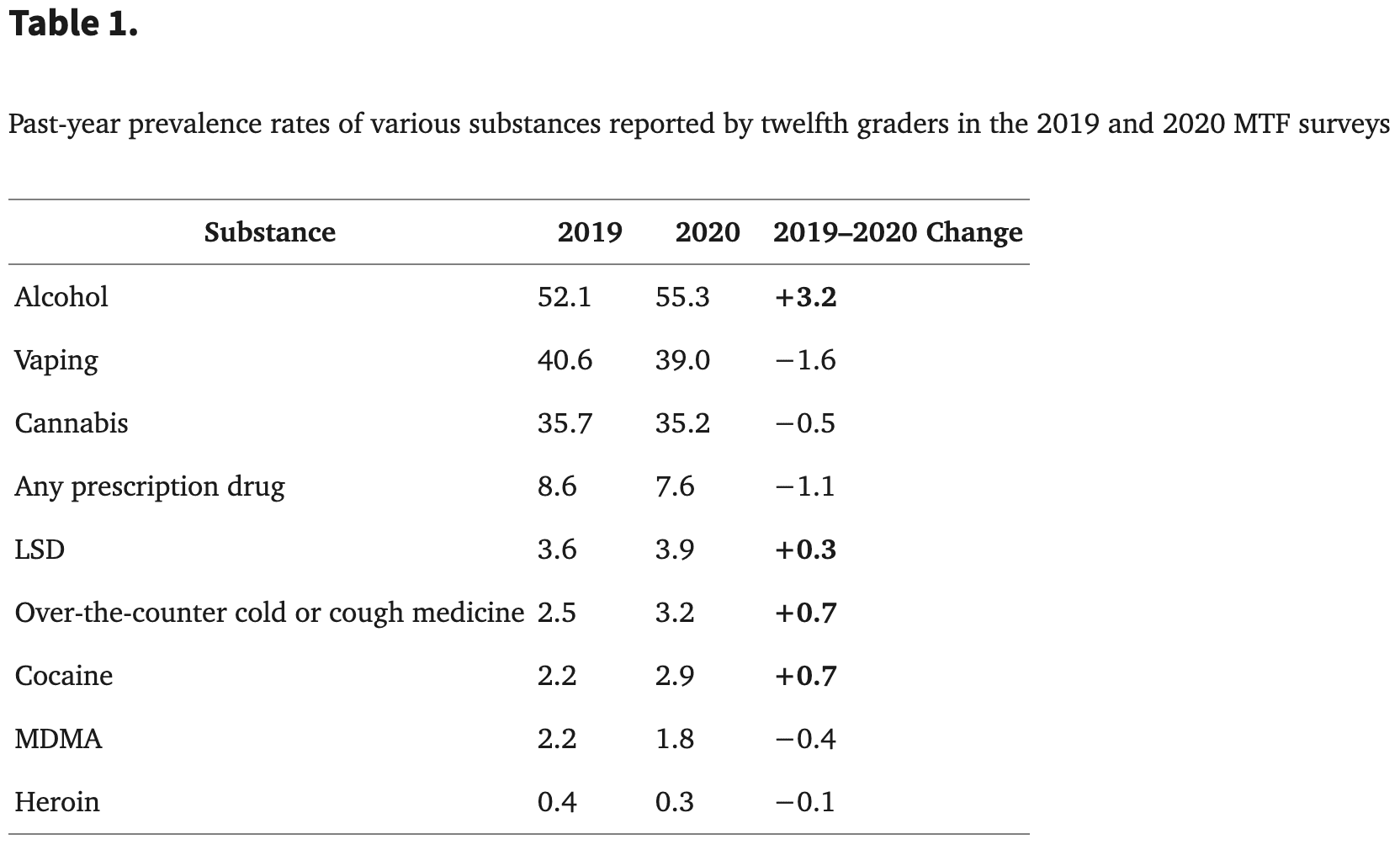
From 2019 to 2020, there were nonsignificant increases in alcohol, LSD, over-the-counter cold and cough medications, and heroin use.7 However, it is not clear whether these changes are related to the COVID-19 pandemic, because annual surveys on substance use also have been impacted by the pandemic. For example, the MTF generally is administered from February through May, with results released later in the year. Because of the pandemic, schools closed in-person operations in mid-March 2020 and only one-quarter of the usual sample had completed the survey.8 These 2020 data are considered nationally representative, however, and indicate that the rates of vaping of both nicotine and marijuana had leveled off somewhat compared with the alarming increases in previous years. The use of drugs like cocaine, MDMA, and heroin remained relatively low among twelfth graders. Whether these trends will continue throughout the pandemic will not be known until this year’s MTF survey data are available in late 2021.
The National Survey on Drug Use and Health (NSDUH) is another major national survey that provides data on the use of alcohol, tobacco products, and illicit drugs. According to results of the 2019 survey, 13.2% of adolescents (12–17 years of age) reported cannabis use in the past year, and 9.4% reported past year alcohol use.9 Of note, 1.4 million teens initiated cannabis use in 2019, which equates to 3700 teens a day starting cannabis use. The overall use rates differ between the MTF and NSDUH surveys owing to differing methodologies, different age groupings (ie, the NSDUH groups 12- to 17-year-olds together and puts 18-year-olds, who generally have high rates of use, in an 18- to 25-year-old group, whereas the MTF groups by grade level). In addition, the NSDUH interviews are conducted in homes, where a lack of privacy might result in adolescents underreporting their drug use.10 The NSDUH 2020 results will not be available until fall 2021.
Effects of the COVID-19 pandemic on adolescent substance use
Although data are lacking, it seems that adult substance use has increased in response to the stress and isolation associated with months of lockdown and social distancing.8 This point may be true for adolescents, as well; data from the Centers for Disease Control and Prevention indicated that 10% of individuals aged 18 to 24 in their sample of 5412 online survey respondents increased their substance use in the past month (the survey was completed during June 2020), with the greatest increases observed at the younger ages within the cohort.11 However, this study did not include teens under the age of 18 years. The only studies published to date that specifically examined the effects of the pandemic on substance use in younger adolescents include online surveys conducted in Canada and an online survey on vaping from Stanford University.12, 13, 14 The results of these studies indicate that the impact of the pandemic on adolescent substance is far from clear.
An online survey was administered to 1054 Canadian teens (aged 14–18 years) who provided information about their alcohol, cannabis, and vape use in the 3 weeks before and 3 weeks after the start of the COVID-19 stay-at-home orders. The results indicated that, overall, fewer teens reported binge drinking, vaping, or using cannabis after COVID compared with before COVID, and alcohol use was unchanged. However, among teens who did use substances, the mean number of days they used alcohol (0.76–0.96 days) and cannabis (0.94–1.1 days) were significantly greater after COVID compared with before COVID.12
Interestingly, use patterns changed after COVID as well. Substance use by these respondents was most often solitary (49%), followed by with parents (42%), with friends via technology (32%), and face-to-face with peers (24%). Given that adolescent substance use is a highly social behavior, the proportion of teens who reported solitary substance use rather than virtual or face to face with friends is fairly unexpected. Solitary use was associated both with increased fears about COVID-19 and depressive symptomatology. The authors posited that teens who tend to use substances to cope with negative affect may increase their use in response to pandemic-related stress and isolation.12 This finding is in contrast with previous reports that teens are less likely to use drugs to cope with stress and less likely to use them alone.15 , 16 This change in use patterns is particularly concerning, because solitary teen substance use has been linked with poorer mental health,17
Similarly, the rather large percentage of teens who reported using alcohol with their parents is surprising and distressing, particularly because 26% of them reported binge drinking with their parents. Through this behavior, parents not only are communicating approval of alcohol use by their teens, which is a known risk factor for risky substance use,18 but they also are presumably providing alcohol to their teens. Although teens tend to use alcohol moderately when using with their parents, they are also more likely to engage in higher risk drinking outside of the home.18 , 19
Conversely, it is not surprising that teens would use substances with peers via video chat or post photos on social media of themselves engaged in substance use, because these behaviors offer a means of feeling more connected during social distancing. Finally, and somewhat alarmingly, 24% of teens reported using substances face to face with peers, apparently not adhering to emergency stay-at-home orders. It is not clear from the study whether parents were aware of or permitting social interaction with peers. It may be that adolescents do not consider themselves to be at high risk for developing severe coronavirus symptoms and were more willing to take chances with their health. Although this study was conducted very early in the pandemic and patterns of use may not have been established, results provide preliminary information on COVID-19–related substance use trends.
Other studies have demonstrated decreased substance use during the pandemic. Some evidence suggests that decreased commercial availability and access to vape products may have decreased rates of vaping.20 A survey on self-reported vaping habits was conducted in May 2020, 2 months after stay-at-home orders were issued. Data from 2167 e-cigarette users aged 13 to 24 years indicated that 67% of the 1442 participants who were 21 years and younger reported quitting or decreasing their use of vaping products in the 2 months since the pandemic started. Among reasons given for this change included concerns about lung function, an inability to purchase products, and worry about parents finding out. Because adolescents typically report obtaining e-cigarettes from friends or brick-and-mortar retail stores and not online, stay-at-home orders that closed vape shops and decreased social contact prevented many teens from obtaining vape products from stores or friends, resulting in decreased rates of vaping.21
Social distancing was offered as an explanation for the decrease in substance use during the first 2 weeks after closure of nonessential services in Canada, according to data collected using an online survey of 622 youth and young adults in established clinical and community settings.13 Unfortunately, no information was provided on the types of the substances used or the frequency or quantity of use, and the findings were not reported by age groups.
Additional COVID-19–related factors likely to impact adolescent substance use
Until it is possible to fully characterize the effects of the pandemic on adolescent substance use patterns, we can look to well-known risk and protective factors for substance use to anticipate potential use and plan for current and future treatment needs, even in these exceptional circumstances. For example, factors typically associated with an increased risk for use include drug availability, association with peers who use drugs, a lack of parental supervision, boredom, and coping with negative affect, among others. In contrast, parental monitoring, a lack of negative peer influence, academic achievement, and strong family and community attachments are considered protective factors. Although the pandemic might cause the rates of substance use to increase as teens seek relief from stress, isolation, or boredom, it is also possible that pandemic-related restrictions will decrease known risk factors and decrease substance use.2 , 22
Certainly, the COVID-19 pandemic has disrupted daily life and contributed to higher levels of stress and anxiety in both adults and adolescents. Adult drinking has increased substantially during the pandemic, resulting in greater teen exposure to parent alcohol use and possibly greater accessibility to alcohol and other drugs in the home.23 In turn, adolescents who have access to a variety of substances within their homes may be at risk for increased substance use. In 2019, 87% of reports made to poison control centers in the United States involving exposures among individuals 13 to 19 years old occurred in the home. The most common substances these adolescents were exposed to included prescription or nonprescription pain relievers, antidepressants, sedatives, hypnotics, antipsychotics, antihistamines, and stimulants or street drugs. More than 60% of these exposures were reported as intentional.24 A related potential risk factor involves parents modeling substance use to relieve stress, which increases the risk that teens will use substances to relieve stress, manage negative affect, and cope with feeling isolated. Similarly, older siblings in the home may also be facilitating use by their younger siblings through co-use or providing their younger siblings with access.22 Additional reasons for post-COVID increases in alcohol and cannabis use could include an increase in unstructured time resulting from asynchronous remote learning and a lack of extracurricular and other leisure activities, as well as social isolation, boredom, and life stress, which may all have increased for adolescents during stay-at-home orders.4 , 25
Conversely, several factors likely contribute to a decreased risk of substance use during the pandemic.2 Perhaps the greatest risk reduction comes from the increased time that parents are at home with their children. Not only are families eating meals together and participating in shared activities, which might decrease the risk of engaging in unhealthy behaviors like substance use, but parental and caregiver monitoring is likely increased, as well. Having parents and caregivers home much of the time might curtail activities conducive to binge drinking, such as parties, and make it much more difficult for teens to obtain and use vaping products and other substances.26 Similarly, stay-at-home orders have limited opportunities for teens to spend time with peers who engage in unhealthy behaviors like substance use, which is significant, because the time spent with substance-using peers is a major risk factor for substance use.27
For teens who experienced academic or social pressure at school, remote or hybrid learning offer less anxiety and stress. This decreased stress may have decreased substance use by teens who use drugs to cope with stress and negative affect. In addition, remote learning does not require early morning start times, thus alleviating the sleep deprivation that is a risk factor for substance use.2
Finally, for teens who have not yet started substance use, fewer opportunities to engage in risky behavior and restricted access to alcohol and drugs that result from parents being at home and social distancing may translate into delayed initiation of substance use. Delaying the onset of substance use is a primary target of prevention strategies, given the effects of substances on the developing adolescent brain.28 In addition, the earlier the onset of use, the greater the risk of developing substance use disorder in adulthood.29 Thus, social distancing may be offsetting the first use of substances, which may decrease the risk of future problematic use.2
Effects of substance use on COVID-19 susceptibility and severity
Although it seems that younger people are less likely to contract COVID-19 than older adults, it is not clear whether using substances or having a substance use disorder makes an individual more susceptible to coronavirus transmission or increase the likelihood of severe infection.30 Alcohol and/or other drug use can lead to changes in immune, pulmonary, and respiratory function that affect the ability to fight infection.31 , 32 For example, alcohol consumption can impact the immune system and heavy use can lead to chronic weakening of lung function over time, increasing the risk of developing pneumonia.33 Stimulants like cocaine and methamphetamine act as vasoconstrictors that can cause pulmonary and cardiovascular damage. Opioids, particularly at high doses, can slow breathing and cause hypoxia, putting users at risk of overdose. Drugs that are administered via smoking or inhalation, such as nicotine or cannabis, can worsen respiratory conditions like asthma and may increase risk of severe illness from COVID-19, even for adolescents. Emerging evidence indicates that smoking and vaping can cause lung irritation, inflammation, and damage to lung tissue, which can increase the risk of viral infection.34, 35, 36 Youth who smoke or vape may be more likely to develop complications from coronavirus, such as pneumonia or acute respiratory distress. Behaviors associated with smoking and vaping also increase the risk of viral transmission. For example, teens often exhale forcefully when vaping and cannot wear masks while they are using. In addition, smoking and vaping behaviors typically include the sharing of joints, blunts, and vaping devices, which increases opportunities for exposure.37
Gaiha and colleagues14 conducted the first (and only, to date) population-based, cross-sectional online survey study to investigate associations among smoking, e-cigarettes, and COVID-19. A total of 4351 adolescents and young adults (13–24 years) completed the survey, and the results indicated that youth who used e-cigarettes were 5 times more likely to become infected with COVID-19 illness compared with nonusers, and those who co-used e-cigarettes and tobacco cigarettes were 7 times more likely to become infected.14 The high rates of vaping in teens combined with links between smoking and vaping and increased risk for COVID-19 illness underscore the need for health care providers to screen all youth and COVID-19–infected youth for cigarette and e-cigarette use.6 , 7 , 14
Adolescent substance use treatment
According to the most up-to-date NSDUH, approximately 1.1 million adolescents in the United States met diagnostic criteria for a substance use disorder in 2019, a significant increase from 2018.38 Despite a greater number of adolescents using substances, there was no significant increase in the number of adolescents engaged in treatment for a substance use disorder. Only 8.3% of these adolescents received substance abuse treatment in the year leading up to the survey.38 Among those who did not receive any treatment, approximately 98.5% reported that they felt they did not need treatment, despite meeting criteria for a substance use disorder diagnosis (Substance Abuse and Mental Health Services Administration, 2020).38 Thus, clinicians working with adolescents with a substance use disorder must consider the needs of the adolescent as well as their level of motivation to change when choosing a specific intervention. The following evidence-based treatment approaches have been found to be efficacious for treatment of substance use disorders among adolescents with varying needs and levels of readiness for treatment.39
Behavioral Interventions
Cognitive behavioral therapy (CBT), motivational interviewing (MI), contingency management (CM), and motivational enhancement therapy are all approaches to treating substance use that, according to Division 12 of the American Psychological Association, have strong research support. The National Institute on Drug Abuse has also recognized the adolescent community reinforcement approach (A-CRA) and 12-step facilitation therapy as acceptable treatments for adolescents with substance use problems.39
CBT for substance use encourages adolescents to monitor their emotions, recognize thought distortions, and identify substance use triggers. CBT therapists attempt to teach adolescents to anticipate high-risk substance use situations and to develop coping strategies for those situations.39 MI is used to enhance a person’s motivation for and commitment to change, largely using change talk facilitated by the therapist. It can be particularly helpful for adolescents who are ambivalent about their substance use.40 Motivational enhancement therapy is based on the principles of MI and incorporates individual assessment feedback. The goal of motivational enhancement therapy for adolescent substance use is to help patients to develop a motivation and desire to engage in treatment. Generally, both MI and motivational enhancement therapy are not used as standalone treatment methods, but are combined with CBT.39 , 40
CM uses the principles of reinforcement for decreasing substance use. CM for substance abuse usually involves monitoring drug use behaviors and reinforcing desired behaviors (treatment participation, achieving specified goals, not using drugs, etc) using tangible rewards. CM is typically used as an adjunct to other psychosocial treatment.39 , 40
A-CRA is a treatment that attempts to replace reinforcements for substance use in the patient’s life with more effective family, social, educational, or vocational reinforcers. Finally, the aim of 12-step facilitation therapy is to increase the likelihood that an adolescent receiving treatment for substance use will become involved in a 12-step program such as Narcotics Anonymous.39
Family-Based Interventions
Family-based therapeutic interventions involve the adolescent’s family in their substance abuse treatment. These approaches often address problems beyond the adolescent’s substance use, and may address issues regarding family conflict, co-occurring disorders, and school problems. Interventions that involve the family may be particularly useful for adolescents because most of them live with at least 1 parent or guardian and are subject to their rules and supports.39
Several iterations of family-based interventions have been shown to be efficacious for the treatment of substance abuse among adolescents. Brief strategic family therapy views problem behaviors as stemming from unhealthy family interactions and seeks to resolve negative interaction patterns among family members. Family behavior therapy combines the principles of CM with behavioral contracting to decrease problem behaviors, including substance use. Functional family therapy combines the principles of brief strategic family therapy and family behavior therapy; problem behaviors are viewed as a response to unhealthy family functioning, and behavioral techniques are used to increase family communication and problem solving. Functional family therapy also incorporates principles of CM.39
Multidimensional family therapy combines family- and community-based interventions for adolescents with substance use problems. The goal of multidimensional family therapy is to foster collaboration between the adolescent’s family and the school and/or justice system. For juvenile detainees, ‘Multidimensional family therapy is often used to facilitate their reintegration into their community. Similarly, multisystemic therapy incorporates the principles of family- and community-based interventions. In this model, the adolescent’s substance use is not only viewed in terms of the adolescent and their family, but also in terms of peers, school, and neighborhood qualities.39
COVID-19 impact on treatment
The majority of adolescents who were in treatment for a substance use disorder in 2019 received care in an outpatient setting; only 9.1% received nonhospital inpatient care, and 1.3% received inpatient care in a hospital setting.38 These percentages are similar to reports spanning 2009 to 2017. Although 2020 treatment data have not yet been published, it is likely that outpatient services will continue to be the most common setting for adolescents in treatment for substance use disorder.
Following the stay-at-home orders and social distancing guidelines that were put into place in March 2020, many outpatient substance abuse clinics experienced partial closures and were forced to suspend certain types of treatment. Group therapies may have been halted to comply with social distancing, and in some instances therapeutic interventions have moved to online formats such as video conferencing. Recent studies have indicated that telehealth interventions show promise in treating substance use disorder among adult patients. For example, the Houston Emergency Opioid Engagement System (HEROES) has transitioned to telehealth services for substance use disorder. Initial studies indicate that this system has maintained patient engagement and has actually experienced an increase in attendance at some virtual recovery group meetings.41
Other researchers have been in the process of creating various digital platforms aimed at supporting individuals with substance use disorder, such as RAE (Realize, Analyze, Engage). RAE is a digital treatment for substance use disorder that includes a wearable device that measures biomarkers of stress and craving. The platform also includes several levels of dialectical behavior therapy interventions, connection to a clinician when a need for help is indicated, and a clinician-facing portal that delivers client information to a treatment team. Clinical trials are set to take place throughout 2021 to better understand the efficacy of this type of platform.42
It is important to note that these studies only included adult samples. There may be unique considerations for using telehealth services to treat adolescents with a substance use disorder. Unlike adults, most adolescents live with a parent or guardian as well as other family members, which may result in limited privacy within their homes. Adolescents may be less likely to be open and honest with health care workers if they fear being overheard by others in the household. Additionally, adolescents with a substance use disorder are more likely to have a parent or caregiver who also has a substance use disorder and 1 in 8 children live with at least 1 parent with a substance use disorder.4 , 43 An adolescent who is seeking treatment for a substance use disorder but who has a parent with an active substance use disorder may feel particularly unsafe engaging in treatment from the confines of their own home. Community-based interventions may be particularly helpful for an adolescent in this position, but the lack of in-person outpatient services may hamper service providers’ ability to integrate an adolescent patient with community supports. Alternatively, adolescents may feel reluctant to seek out any form of in-person treatment for fear of COVID-19 exposure.
Adolescents who are members of at-risk groups likely face additional barriers to receiving treatment during the COVID-19 pandemic. Impoverished and homeless youth, for example, appear to be facing even greater resource insecurity during the pandemic than pre-pandemic. Many of these adolescents are likely unable to engage in telehealth services owing to a lack of internet, phone, or computer access. Additionally, the halt of in-person services and decreased admissions to community service providers/shelters may also create barriers to obtaining mental health and substance use disorder treatment. Not only do health risks associated with both homelessness/poverty and substance use disorder put these adolescents at heightened risk for COVID-19 infection, but lack of treatment may result in an increase in engaging in risky behaviors to obtain substances.44
Lesbian, gay, bisexual, transgender, and gender and sexuality questioning (LGBTQ) youth represent another at-risk group that may be disproportionately affected by the COVID-19 pandemic. Adolescents who identify as LGBTQ are at an increased risk for physical and sexual abuse; stay-at-home orders may inadvertently increase contact with abusers in the home and having an abuser in the home would likely decrease engagement in telehealth treatment. LGBTQ adolescents are already at a higher risk for a multitude of psychological disorders, including substance use disorder; this risk, coupled with the potential for increased victimization, may contribute to an increase in substance use.44
Finally, adolescents have not been spared from the opioid epidemic. From 1999 to 2016, overdose deaths owing to prescription opioids, heroin, and fentanyl increased by 95%, 405%, and 2925%, respectively, in youth under the age of 20.45 Recent findings indicate that opioid overdoses have increased during the COVID-19 pandemic46 with disproportionate increases observed among Black Americans.47 Data from the Centers for Diseaswe Control and Prevention48 from more than 42 states show that nonfatal opioid-related overdoses have also risen dramatically since the pandemic was identified in March 2020. Heroin overdose rates peaked in May 2020 and have gradually decreased, although the rate in September 2020 (the most recent month with available data) remained elevated compared with almost all of 2019. Similarly, nonfatal overdoses from opioids peaked in July and slightly decreased in August and September, although the rate in September is greater than prepandemic 2020 and any month in 2019.48 Although these COVID-19–related results did not examine adults and youth separately, the significant increases in adolescent opioid overdoses observed in prepandemic years largely mirrored those seen in adults. Thus, it is reasonable to suspect that the number of fatal and nonfatal opioid-related overdoses have also increased significantly in adolescents during COVID-19. The increase in opioid overdoses may be due to several factors, including disruption to treatment, an increase in mental health stressors, and an increased prevalence of solitary substance use, leading to a decrease in readily available assistance.
Implications for treatment
Although an increase in substance use among adolescents during the COVID-19 pandemic is not definitive, treatment providers may benefit from preparing for an increase in the number of adolescents who need treatment for a substance use disorder as services begin to return to in person. Pediatricians and primary care providers should screen for substance use during routine checkups and may want to consider administering urine drug screens to concerning patients.4 Additionally, clinicians who are providing general psychological services to adolescents should consider incorporating substance-related programming into their services; even adolescents who do not meet criteria for a substance use disorder may benefit from some substance-related treatment.39 Treatment providers who service impoverished, homeless, or LGBTQ adolescents in particular may experience an increase in demand for in-person services owing to barriers to telehealth treatment, as discussed elsewhere in this article.
In the meantime, there are steps that both families and clinicians can take during this time to help adolescents with substance use problems. Stay-at-home orders provide a unique opportunity for parents and caregivers to create and maintain structure in the home. For example, they may implement a morning routine, encourage activities that build connection among family members, and facilitate nonjudgmental open communication within the home to support adolescent recovery efforts. Parents and caregivers should also monitor the adolescent for signs of ongoing substance use or withdrawal symptoms. A publication by J. Wolfe offers some examples of substance use signs that parents and caregivers might report to health care professionals.49 Both withdrawal as well as continued substance use during social isolation may result in difficulty controlling emotions or extreme mood swings among adolescents. Attempts to isolate oneself in the home may also be a sign that an adolescent is hiding efforts to obtain or use substances. Isolation may look like sleeping throughout the day, staying locked in one’s room, or simple avoidance of interaction with family. Additionally, multiple arguments about leaving the home to be with friends or sneaking out behavior may indicate that the adolescent is attempting to obtain or use substances. Last, strange smells coming from the adolescent or the adolescent’s room may also indicate ongoing substance use. For example, marijuana has a distinct skunk-like smell when smoked. Unusually sweet scents may result from the use of a vape or from sweet drinks mixed with alcohol. Additionally, an excessive use of air fresheners, perfume, or cologne may be a tactic used to cover up the smell of substances. If a parent or caregiver is concerned that their adolescent is engaging in substance use, they may consider reaching out to their pediatrician for advice about treatment options.
Service providers who conduct remote services for adolescents with a substance use disorder should make efforts to check-in with the patient about their safety and difficulties they may be experiencing at home. If possible, health care workers should also encourage adolescents to seek out a private space from which to engage in remote treatment. If an adolescent is unable to openly discuss problems they are having because of lack of privacy or fear of safety, providers may want to consider resuming in-treatment services while following social distancing guidelines (ie, staying 6 feet apart, wearing masks, and washing hands and surfaces).
Health care workers may also see this time as an opportunity for encouraging complete cessation of substance use behaviors, including smoking and vaping. Adolescents may be experiencing increased difficulty in accessing various substances, including cigarettes and vapes owing to stay-at-home orders. Thus, treatment providers may use this time to increase motivation to quit; pediatricians or other health care professionals may also consider prescribing nicotine replacement treatments to help with craving or withdrawal symptoms experienced by adolescents.50 Last, many 12-step support groups such as Alcoholics Anonymous and Narcotics Anonymous have transitioned some of their meetings to an online platform. Their respective websites now have entire pages devoted to providing information about virtual meetings, including how to find and join a virtual meeting. Adolescents with substance use problems may benefit from receiving this type of support, particularly if they have experienced a disruption in their in-person treatment.
Future directions
Exploring the various impacts of the COVID-19 pandemic on adolescent substance use provides a unique opportunity to understand factors that both increase and decrease the risk of future substance use among teens. Some pandemic-related life changes, such as social isolation and boredom, seem to exacerbate the risk of substance use. Other changes seem to mitigate some of the risk, including increased family time, parental monitoring, and decreased access to substances.
Longitudinal studies are needed to monitor shifts in substance use patterns over time as the pandemic evolves to fully characterize the impact of pandemic-related stresses on teen substance use, motivations for use, and mental health correlates. Given the key role of peer pressure and social group dynamics in determining drug experimentation and use in teens, important factors to examine include the long-term consequences of school closures, remote and hybrid learning, social distancing, and quarantining. Studies also are needed to understand how the pandemic changed opportunities for teens, and their family members, to engage in substance use, and whether these changes increased or decreased use.
Studies should also examine the parental permissiveness that allowed for the parent–teen drinking and binge drinking behavior reported in the early weeks of the pandemic in the study by Sumas and associates.12 Although some parents may have relaxed some rules in the face of the exceptionally challenging circumstances created by the shutdown, perhaps considering alcohol use with parents at home relatively safer for their teens than sneaking out and drinking with friends, there may be lasting effects of this co-use drinking behavior, because parental permissiveness has been linked to higher rates of substance use.22 , 51
Summary
Currently, it is not clear whether substance use by teens has increased or decreased since the state of emergency was declared in mid-March 2020. Stressors such as uncertainty, fears about contracting the virus, social isolation, boredom, and sheltering in place potentially increase the risk of use, whereas increased parental monitoring and reduced access to substances and substance-using peers likely decrease the risk. Regardless, the sustained social disruption related to the COVID-19 pandemic will have lasting effects on adolescents. Future research should identify protective factors that decrease use, because these factors might be continued once normal life resumes. Similarly, identifying risk factors associated with increased use could provide targets for treatment. In the meantime, it is likely that partial clinic closures as well as the transition to providing services online uniquely affected the way adolescents engage in treatment. At-risk adolescents may have been particularly affected by these changes. As such, it is important that health care providers consider screening all adolescents for problematic substance use, and regularly monitor adolescents’ safety in addition to maintaining treatment gains. Although stay-at-home orders and social distancing guidelines have made certain aspects of substance use disorder treatment more difficult, these restrictions also present a unique opportunity for parents and caregivers, as well as for health care workers. Parents and caregivers can use this time to increase structure in the home and build stronger connections with their children, and health care workers can use lack of access to substances to set up substance cessation goals for their adolescent patients.
Clinics care points
Telehealth providers should be mindful that adolescents live with a parent or caregiver and because of possible limited privacy within their homes may be less open and honest about their substance use.
About 1 in 8 adolescents with a substance use disorder lives with at least one parent who is actively using substances; this adolescent may not feel safe engaging in substance use treatment while in their home.
Pediatricians and primary care providers should screen for substance use during routine checkups and may want to consider administering urine drug screens to concerning patients.
Treatment providers may want to take advantage of the limited access teens have to cigarettes and vapes during stay-at-home orders and increase motivation to quit; pediatricians may consider prescribing nicotine replacement treatments to help with craving or withdrawal symptoms experienced by adolescents.
Acknowledgments
Disclosure
Supported by the Lycaki/Young Funds from the State of Michigan.