Abstract
## Background People with substance use disorders are considered at increased risk of COVID-19 and its more serious complications, however data on the impact of COVID-19 are lacking. The study aimed to describe the clinical characteristics and outcomes of COVID-19 on people with substance use disorders.
## Methods an observational study was carried out including patients aged ≥ years with COVID-19 pneumonia admitted to an urban hospital during March 12 to June 21,2020.
## Results Among 2078 patients admitted, 27 (1.3%) were people with substance use disorders: 23(85.2%) were men with a median age of 56.1 + 10.3 years and. The main SUD were alcohol in 18(66.7%) patients, heroine in 6(22.2%) and cocaine in 3(11.1%) and 24(88.8%) patients were on ongoing substance use disorder treatment. One or more comorbidities associated to COVID-19 risk were observed in 18(66.6%) of patients. During a median length of stay of 10 days (IQR:7-19), severe pneumonia developed in 7(25.9%) patients, acute respiratory distress syndrome in 5 (18.5%) and none died.
## Conclusion Larger sample sizes and sero-epidemiological studies are needed to confirm the low incidence of severe COVID-19 on patients with SUD.
Introduction
The novel coronavirus disease 2019 (COVID-19) is an acute respiratory illness, which raises mortality rates in older people and those with underlying medical conditions such as cardiovascular disease, chronic respiratory disease, diabetes and cancer.
People with substance use disorders (SUD) are considered at increased risk of COVID-19 and its more serious complications for multiple physiological and social causes.
Comorbidities prevalent among people with SUD, such as cardiovascular diseases, chronic respiratory diseases, diabetes, obesity and cancer, increase vulnerability to COVID-19 and are associated with more severe COVID-19 symptoms, complications and fatalities.
Moreover, high-risk behaviors such as sharing drug-using paraphernalia, difficulties to maintain quarantines and living in close contact with others in crowded shelters may contribute to the spread of COVID-19 among people with SUD.
In addition, social and economic changes caused by the pandemic, along with the inconvenients regarding treatment access and adherence, can aggravate the SUD. Healthcare policies, including physical and social distancing isolation and restricted medical visits during the pandemic make it difficult for healthcare providers to address the needs of people with SUD with the availability of medications, harm reductions programs and mutual supports groups.
Despite this emerging health threat for people with SUD, data on COVID-19 and its intersection with SUD are scant. Therefore, this study aimed to describe the clinical characteristics, related factors and clinical outcomes of COVID-19 in people with SUD admitted to a reference hospital during the pandemic.
Methods
This observational study was conducted at the Hospital del Mar, which is located in one of the district in Barcelona (Spain) with the highest prevalence of people with SUD. This institution is an urban, tertiary, teaching hospital, which offers cost-free acute-care for the district reference population.
All individuals (aged ≥ 18 years) with SUD who were admitted for COVID-19 pneumonia from 12 March to 21 June 2020 (national state of alarm period) were included in the study.
Confirmed COVID-19 pneumonia was defined by clinical and radiological findings and a positive real time reverse-transcription polymerase chain reaction for SARS-CoV-2 in respiratory samples. CURB-65 scale was used to assess the severity of pneumonia. SUD were diagnosed according to the DSM-V-TR criteria.
The main variable of the study was the percentage of patients admitted for COVID-19 pneumonia with SUD. The secondary variables were the prevalence of subtypes of SUD, prevalence of comorbities associated to COVID-19 risk, incidence of acute respiratory distress syndrome and mortality among patients admitted for COVID-19 pneumonia with SUD.
For the purpose of the study, socio-demographic and clinical characteristics were extracted from the patients’ medical records. Recorded variables were age, gender, comorbidities, clinical characteristics of COVID-19 and outcomes.
Descriptive statistics were expressed as mean, standard deviation, median and range for quantitative variables and absolute frequencies and percentages for qualitative variables. The chi-square test was used to compare categorical variables and Mann–Whitney U test for variables that did not follow a normal distribution. A P value < 0.05 was considered significant.
Analysis was made using SPSS software, version 17.0.0 (Chicago, Illinois).
The study complied with the ethical statements in the Declaration of Helsinki (64th General Assembly, Fortaleza, Brazil, October 2013) and approved by the local Ethics Committee.
(Ethics Committee for Scientific Research IMIM, Barcelona, Spain, CEIm-2020/9355/I).
Results
During the study period, there was 2023 patients admitted for COVID-19 pneumonia in the hospital, of whom 27(1.3%) had SUD.
Clinical and social characteristics of 27 patients with SUD included in the study are showed in Table 1. The majority of patients were Spanish men, with mean age of 56 years and stable housing.
Table 1. Social and clinical characteristics of 27 individuals with SUD admitted for COVID-19 pneumonia
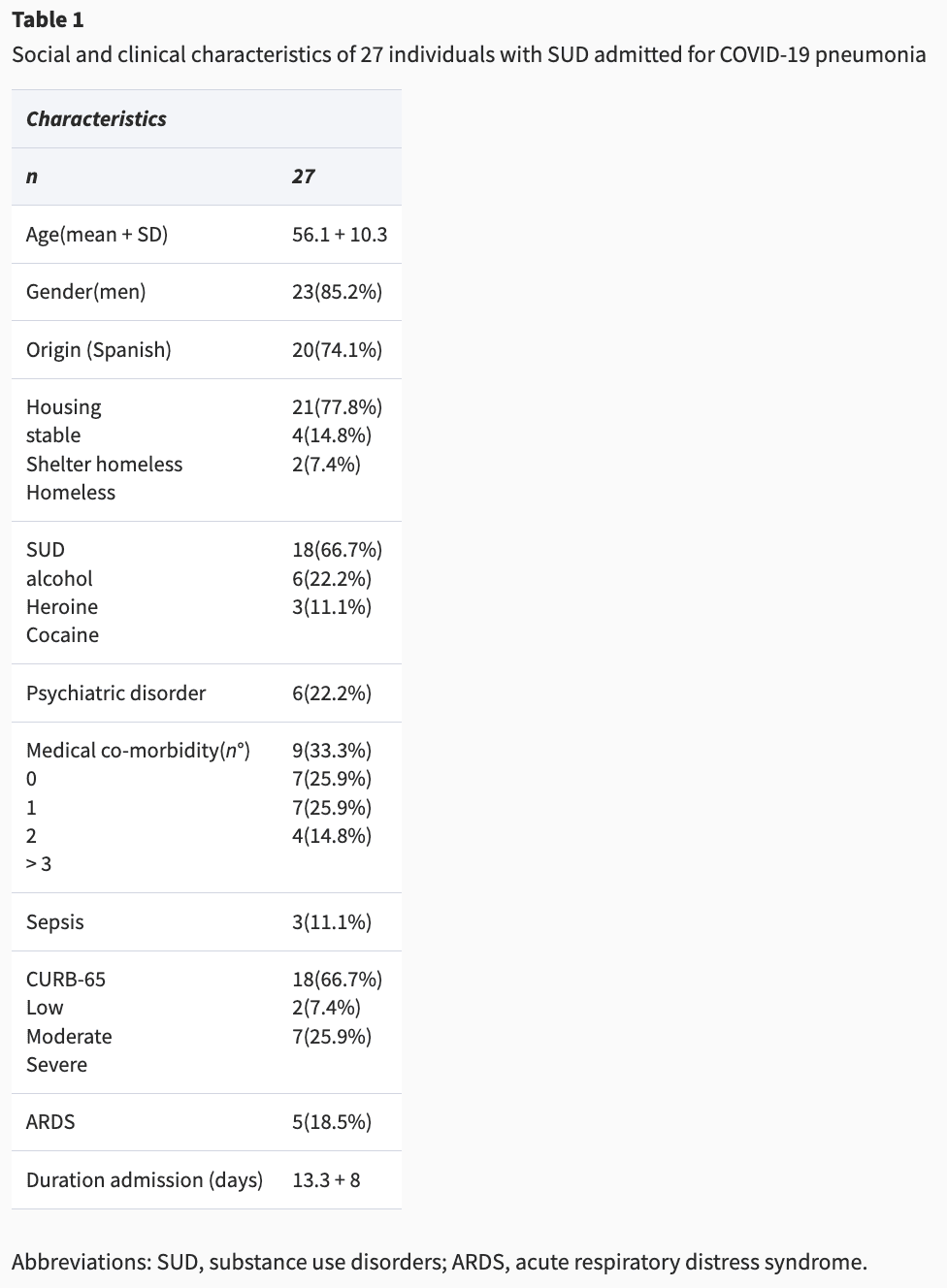
The main SUD was alcohol and a quarter of patients had psychiatric comorbidities. Ongoing SUD care previous to the admission was observed in 24(88.8%) patients.
About two third patients had one or more comorbidities associated to COVID-19 risk. The main observed were: hypertension in 8(29.6%) patients, chronic respiratory disease in 7(25.9%), liver cirrhosis in 5 (18.5%), chronic heart disease in 4(14.8%), chronic renal disease in 3 (11.1%), diabetes in 2(7.4%) and cancer in 2(7.4%). Patients with alcohol use disorder had more median COVID-19 risk factors than other patients (3 versus 1; P 0.02).
HIV infection was present in 2(7.4%) patients and chronic hepatitis C in 1(3.7%).
Fever and respiratory symptoms were present in all 27 patients, astenia and myalgia in 21(77.8%) and gastrointestinal in 4(14.8%).
During a median length of stay of 10 days (IQR: 7–19), severe pneumonia developed in 7(25.9%) patients, acute respiratory distress syndrome in 5 (18.5%) and none died.
Discussion
Main finding of this study
In spite of the hypothetical risk for COVID-19, this study showed that a small number of people with SUD were admitted for COVID-19 pneumonia in a public referral hospital.
What is already known on this topic?
Several factors could explain the low percentage of patients with SUD admitted for COVID-19 pneumonia in this study.
First, despite Spain has been one of the European countries most affected by the COVID-19 pandemic so far, the findings from the recent nationwide seroprevalence study for SARS-CoV-2 have indicate that the prevalence of IgG antibodies against this coronavirus is ~5%, reflecting a low incidence of the disease in the general population.
Second, among adults, the risk for severe illness from COVID-19 increases with age, with older adults at highest risk and representing more than 80% of admitted patients with COVID-19 from the general population. By contrast, younger adults < 40 years represent only 10% of hospital admissions. In this sense, the median age of patients on SUD treatment in Barcelona is ~40 years and the main type of substance use is alcohol. According to these data, the majority of admitted patients with SUD had alcohol use disorder a median age of 56 years old in this study.
Finally, three quarters of patients scored low-moderate risk in the pneumonia severity index according to CURB-65 scale, so that the low severity of symptoms could have been confused by patients as withdrawal syndrome, or that patients could have decided not to go to overwhelmed hospital emergency department during the epidemic, In this sense, only 20% of symptomatic participants with antibodies against SARS-CoV-2 reported a previous PCR in the national prevalence survey, which was positive in ~75 of cases, suggesting that a substantial number of symptomatic patients with COVID-19 did not undergo medical assessment in the general population.
Moreover, asymptomatic infections, which are more frequent in young adults under 40 years of age of the general population, could have contributed to the low number of COVID-19 among people with SUD, given the same median age of people with SUD on ongoing SUD of the local area.
What this study adds
The group of patients with SUD admitted for COVID-19 was represented by patients over 50 years of age, diagnosed of alcohol use disorder and with a high prevalence of comorbidities associated to COVID-19 risk. This data should be taken into account when planning COVID-19 prevention measures, since the aging of populations with SUD and the progressive increase of older adults seeking treatment in drug addiction care centers.
Limitations of this study
Although this observational data collected from one hospital alone may limit the generalization of the findings, Hospital del Mar is the reference hospital for one of the district of the city with the highest prevalence of people with SUD and a large number of patients were admitted during the study period, thus the sample was representative. Otherwise, rates for inhabitant would have better indicated the COVID-19 risk among people with SUD, however, there was only local data about the population on ongoing SUD treatment which could exclude a considerable number of patients of the denominator.
Conclusion
The low number of people with SUD and COVID-19 admitted to the hospital in this study highlights the urgent need to carry out larger sample sizes and sero-epidemiological studies of SARS-Cov-2 infection in order to more completely understand the effects of COVID-19 among people with SUD. Meanwhile, it is mandatory to guarantee access to healthcare during the pandemic, including social and medical assistance for SUD and COVID-19.